Abstract
While alcohol consumption is known to increase the risk of several types of cancer, evidence regarding the association between alcohol and melanoma is inconclusive. This pooled analysis was conducted to examine total alcohol consumption (grams per day), and type of alcohol consumed (beer, wine, beer and wine combined, and liquor) in relation to melanoma among women using original data from eight completed case–control studies (1886 cases and 2113 controls), with adjustment for the potential confounding effects of sun exposure-related factors. We found a positive association with ever consuming alcohol [adjusted pooled odds ratio (pOR) 1.3, 95 % confidence interval (CI) 1.1–1.5]. Specifically the pORs were 1.4 (95 % CI 1.1–1.8) for wine, 1.1 (95 % CI 0.9–1.5) for beer and 1.2 (95 % CI 1.0–1.4) for liquor. However, the pOR for the highest fourth of consumption compared with never consumption was 1.0 (95 % CI 0.7–1.3) without evidence of a trend with increasing amount of total alcohol, or separately with amount of beer, wine or liquor consumed. Stratifying by anatomic site of lesion, number of nevi, age group, or histologic subtype did not alter these results. Although the results showed a weak positive association between ever consuming alcohol and melanoma occurrence, our findings do not provide strong support for the hypothesis that alcohol consumption plays a role in the development of melanoma in women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Melanoma is a potentially fatal skin cancer with increasing incidence for several decades in most white populations worldwide. It is estimated that over 232,000 new cases of melanoma occurred in 2012 worldwide with more than 250,000 cases expected in 2015 [7]. The major environmental cause of melanoma is excessive exposure to ultraviolet (UV) radiation [19]. Given the consumption of alcohol increases the risk of developing several cancers, including a range of gastro-intestinal cancers [39], alcohol may also be related to the development of melanoma. The proposed mechanism is that the consumption of alcohol may exacerbate the production of oxidative stress. This process results in DNA damage and carcinogenesis by increased photosensitivity and compromised antioxidant defense mechanisms of the skin [30]. However, epidemiological evidence for an effect of alcohol consumption on the risk of melanoma remains inconclusive. This is despite suggestive findings from a recently published systematic review and meta-analysis where 14 case–control and two cohort studies of alcohol consumption and melanoma risk were identified [29]. Meta-analysis of their data suggested that people who had consumed any alcohol had a significant 20 % increased risk of melanoma compared with those who never had consumed alcohol. However, this significant association was seen mainly in women and the overall results of the meta-analysis when restricted to studies that had adjusted for sun exposure showed no significant association [29]. Thus the observed positive association may have been confounded by sun exposure.
In order to clarify whether there is an association between alcohol consumption and melanoma independent of sun exposure, we conducted a pooled analysis using the original data from eight completed case–control studies of melanoma in women. These studies had collected detailed information about both sun exposure and alcohol consumption. Our analyses also extend previous investigations by including amount of alcohol consumption, histologic subtype and anatomic site.
Materials and methods
This study was restricted to women because the original primary aim of the collaboration was to examine the effects of reproductive factors and sex hormones on the risk of melanoma. A detailed description of the general methods used in our collaborative analyses is provided elsewhere [20, 33]. Briefly, we analyzed studies completed before July 1994 that included melanomas diagnosed both as inpatients and outpatients, had collected data through a personal interview on important risk factors for melanoma (i.e., pigmentary traits and sun exposure history), and included at least 100 women with melanoma and 100 women controls. A total of 12 case–control studies were available [2, 6, 10, 12, 16, 17, 21, 24, 27, 32, 34, 40], but four were excluded from this analysis because information on alcohol consumption was not collected [16, 34, 40] or was no longer available [17]. Descriptive statistics for each of the variables used in the pooled analysis were compared with published results and provided to the original study investigators to ensure their accuracy. Six of the eight studies included in the pooled analyses were population-based [10, 12, 21, 24, 27, 32]; the remaining two [2, 6] were based in hospital/clinic settings (Table 1).
Study variables
Although measurement of alcohol use varied across studies, all had categorized alcohol consumption by drinks per day, per week, or per month. Thus drinks per day was our main variable for analysis of current alcohol intake, and was expressed as grams of alcohol per day, standardized to the portion size and alcohol content specific to each study and its locale [15, 35]. This approach is used routinely in epidemiologic studies of alcohol and health outcomes [38]. Data specific to beer and wine consumption were available for five studies [2, 10, 12, 21, 27]. One study asked specifically about beer and wine consumption combined [24]. To include these data with the rest, we created a beer plus wine intake variable and calculated the combined alcohol from both beer and wine from the five other studies with available data [2, 10, 12, 21, 27]. The information on liquor consumption was available from six studies [2, 10, 12, 21, 24, 27].
Participants were classified by alcohol consumption status (“never” or “ever”) and dividing consumption levels into equal fourths. We also assessed the risk of melanoma separately for each type of alcohol, and these consumption levels were categorized into equal thirds. The non-consumption category was used as the referent group.
We also examined variables that could potentially modify or confound the analysis of alcohol-related factors and melanoma risk namely educational level; hair, eye and skin color; freckling; family history of melanoma in a first degree relative; skin reaction to acute sun exposure; indoor tanning exposure, or outdoor sunbathing [20]. Level of education was categorized into: grade/high school, college, or graduate school, except two studies [21, 27] that included a category for technical school. We used the classification scheme developed for earlier pooled analyses for hair color, eye color and family history of melanoma [3, 9]. Skin reaction to acute sun exposure was categorized into three groups (never burn, burn then tan, or always burn). Information on the number of nevi was dichotomized as “none” or “any” as the definition and method to assess nevi differed greatly across studies, and categorical analysis resulted in insufficient numbers in each cell to undertake analyses. We selected the sun exposure-related factors most strongly associated with melanoma risk within each study i.e., history of sunburns [2, 6, 12, 32], history of sunburns in childhood [27], history of sunburns as a teenager/young adult [24], recreational sun exposure [10], and sun exposure in childhood [21].
Statistical analysis
A two-stage method of analysis was used to obtain both study-specific odds ratios (ORs) and pooled ORs (pORs) with 95 % confidence intervals (CIs) [33]. In the first stage of analysis, each study was analyzed according to its original design. Frequency-matched studies were fitted to unconditional logistic regression models with categories of age along with other covariates. Pair-matched studies were fitted to conditional logistic regression models, using the original matched pairs and additional covariates. To evaluate inter-study variability, we examined the study-specific ORs and tested for statistical heterogeneity using a χ 2 test. The pooled exposure effect was estimated in a second-stage linear model as the average of the study-specific ORs, weighted by the inverse marginal variances. The marginal variance was the sum of the individual study variance and the variance of the random study effect. In the absence of heterogeneity, the marginal variance was the study-specific variance alone [33]. We used a critical value of t = 2.36 for all two-stage analyses, regardless of number of studies in the analysis, to be consistent with the t statistic that would be used with joint-effects models. In the presence of heterogeneity, we examined potential sources of heterogeneity by stratifying on type of control group (population vs. hospital-based controls) and how the questionnaire was administered (telephone vs. in-person interview) and applied a random effects model.
All estimates were age-adjusted. To assess the effects of other potentially confounding factors (including educational level, hair, eye and skin color, freckling, presence of dysplastic nevi, family history of melanoma in a first degree relative, ethnicity, number of nevi on the arms, skin reaction to sun exposure, sun exposure history [20], and total energy intake (Kirkpatrick et al. [21] only), we examined the percent change in the age-adjusted pOR with the addition of each factor using standardized groupings [3, 9, 20]. Variables resulting in a 10 % or greater change in the estimate were included in the final models. To assess stratum-specific effects (e.g., age category or anatomical site), we broke the pairs and stratified on age (<50, or ≥50 years), anatomical site, histological subtype and the presence of nevi.
Our main analyses were based on all melanomas combined. Additionally, we separately computed odds ratios for each of the primary exposure variables by histologic subtype [superficial spreading melanoma (SSM), nodular melanoma (NM) and lentigo maligna melanoma (LMM)]. In the analysis of less common histologic subtypes (NM and LMM), we broke the pair-matched sets to increase statistical power and analyzed the studies adjusting for the original age categories using conditional logistic regression. All analyses were conducted using SAS (SAS Institute, Cary, NC).
Results
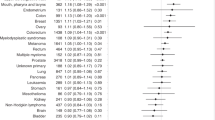
The eight case–control studies provided a total of 1886 melanoma cases and 2113 controls for the analysis. Among them, 72 % of cases (n = 1351) and 69 % of controls (n = 1460) had ever consumed alcohol and 8 % of cases (n = 115) and controls (n = 135) had consumed at least 10 g per day of alcohol on average. Compared with women who ‘never’ had consumed alcohol, the overall pOR for women who ‘ever’ consumed was 1.3 (95 % CI 1.1–1.5) (Table 2) with statistically significant heterogeneity in the results (Supplemental Table in Online Resource 1). When the amount of alcohol consumption was examined, the pOR for the highest fourth of consumption compared with women who never consumed alcohol was 1.0, and no trend in risk was observed with increasing amount of alcohol consumed. None of these results were changed by more than 10 % with the addition of potentially confounding factors. We also assessed whether alcohol consumption and exposure to indoor tanning devices or sun exposure interacted to affect risk of melanoma. We observed a statistically significant interaction between alcohol and never/ever-use of tanning devices (p interaction = 0.043). Among those who never used tanning devices, consumption of alcohol was positively associated with melanoma (Never vs. Ever OR 1.38; 95 % CI 1.17–1.64) whereas there was no association among women who ever used tanning devices (Never vs. Ever OR = 0.99; 95 % CI 0.72–1.33). There was no evidence of interaction of alcohol intake with history of severe sunburn in the association with melanoma (p interaction = 1.00). Regardless of history of severe sunburns, those who consumed alcohol had raised ORs although they were not statistically significant.
When alcohol consumption from the different types of beverages was examined, similar patterns of associations were observed (Table 2). The pORs for women who ‘ever’ had consumed wine, beer and wine combined, and liquor were slightly higher compared with those who ‘never’ consumed these beverages and in the case of wine, the association was statistically significant. However, there was no trend of increasing risk observed with increasing amounts of alcohol consumed for any beverage type. We further examined whether the relation between alcohol consumption and melanoma risk followed a nonlinear pattern by fitting parametric (quadratic, square root) and nonparametric nonlinear models (spline and loess) to total grams of alcohol consumed per day (untransformed, log transformed) but found no evidence of a nonlinear pattern (data not shown).
In analyses stratified by anatomic site (Table 3), the pOR was increased for melanoma of the trunk observed among women who ‘ever’ compared with ‘never’ had consumed alcohol (pOR 1.5, 95 % CI 1.1–1.9). But again, melanoma risk did not vary with the amount of alcohol consumed; and there was little to no evidence of an association with the other anatomic sites.
We further conducted an analysis stratified by the number of nevi (Table 4). Among women with any nevi present, higher pORs were observed for those who ‘ever’ had consumed alcohol compared with women who ‘never’ consumed (pOR 1.4, 95 % CI 1.1–1.7) but there was no trend with amount of alcohol consumed. Among women with no nevi, alcohol consumption was unrelated to melanoma.
As menopausal status could have modified the association, analyses were stratified broadly into pre- and post-menopausal groups (<50 years and ≥50 years). In both groups, a modest association was observed without evidence for dose–response effect (Supplemental Table in Online Resource 2). Finally, alcohol consumption was not related to risk of any specific histologic subtype of melanoma (Supplemental Table in Online Resource 3).
Discussion
In this pooled analysis, we found an overall positive association between ever having consumed alcohol and incident melanoma in women. However, the association between the amount of alcohol consumed and incidence of melanoma was seen irrespective of the type of alcohol consumed. The magnitude of associations changed very little after adjustment for known confounding factors, and no significant dose–response associations were seen with increasing amounts of alcohol (including specific types) consumed. Further, our findings did not suggest that the association was specific to any particular anatomic site or histologic subtype nor was modified by the presence of nevi or age groups that reflected menopausal status.
These findings contrast results from a large cohort of US post-menopausal women in the Women’s Health Initiative Observational Study (WHI OS) that reported that the amount of alcohol consumption, and the preference of white wine and liquor (but not beer or red wine) were significantly positively associated with melanoma after adjustment for sun exposure and other risk factors for melanoma [23]. Variation in methods makes it difficult to compare the findings from WHI OS and ours. For example, in WHI OS, alcohol use at baseline was categorized as the number of drinks/week; and they measured alcohol preference rather than types of alcohol consumed. However, women in the WHI OS who were excluded from the analyses may have had higher melanoma risk compared with those who were included. The observed positive association may be biased because women who were non- and ex-alcohol consumers, older, obese, and obtained less education were also more likely to be excluded [23]; and people who have such characteristics often have increased risk of disease. The nature of the study design may also have influenced the conflicting findings as ours is retrospective whereas the WHI OS is a prospective study design.
A recently published systematic review and meta-analysis of alcohol consumption in relation to melanoma based on 14 case–control studies and two cohort studies (not including the WHI OS [23] ) reported findings that agreed with our results for ever vs. never alcohol exposure: men and women who consumed any alcohol had a 20 % increased risk of melanoma compared with non/occasional alcohol consumers [29]. Analyses restricted to women, based on three studies, also showed a significant 26 % increased risk with ever consuming alcohol. Unlike our overall results which did not change on adjustment of sun exposure, a positive but non-significant association was observed when the meta-analysis was limited to studies that adjusted for sun exposure. However, their adjusted result was similar to our detailed findings after adjustment (including interaction terms) for specific high-risk UV exposures from severe sunburns or use of tanning devices. Their findings also suggest dose–response relationship when men and women were combined; however, these significant risk estimates were based on studies not adjusted for sun exposure and there was significant heterogeneity in the included studies.
It is possible that our findings were influenced by socioeconomic factors, though when we included education in the analyses as an indicator of socioeconomic position, the pooled odds ratios changed negligibly. Education has been associated with alcohol intake patterns in women, especially in developed countries [28]. While women in higher socioeconomic groups are more likely to consume alcohol compared with their counterparts in lower socioeconomic groups [28, 31], women in lower socioeconomic groups are more likely to binge drink [8]. Further, the associations between socioeconomic position and melanoma vary from positive in Europe [18], to positive [14, 26] or negative in the US [13], to no association in Australia [1]. This complexity makes it difficult to assess the likely effect of socioeconomic differences if any on our final pooled results.
A major strength of our pooled study was only including studies with available data on sun exposure. Also, pooling the data from eight case–control studies increased the statistical power we had to examine the association between the amount and type of alcohol usually consumed. Pooled analyses also allowed us to undertake sub-group analyses to examine the associations by anatomic site of lesion, histologic subtype, age group, and number of moles.
A limitation of this study is that the data for alcohol consumption were collected by self-report. While alcohol consumption is generally under-reported among heavy drinkers [4], older or highly educated women also tend to under-estimate their past intake [25]. In addition, the accuracy of recalled intake may be influenced by current intake [25]. Moreover, in case–control studies, recall bias is a concern because exposure information (alcohol intake) is collected retrospectively. If the cases systematically under-estimated or over-estimated their intake across all exposure quartiles compared with controls, this could have distorted the reported effect estimates and dose–response associations [37] with attenuation of the latter if the bias operated more among heavy-drinkers. A previous study that investigated the effect of potential recall bias in alcohol intake and breast cancer found that cases had somewhat more biased reports than controls [11]. Even if misclassification of the alcohol drinking level was similar between cases and controls, distorted associations in any direction are possible with use of polychotomous exposure variables [5]. Further, we could not discriminate lifetime abstainers and former alcohol consumers and yet these groups often have very different characteristics regarding health consciousness and possibly other factors that influence their risk of melanoma [22]. Such measurement errors may also have contributed to our observed lack of dose–response despite a statistically significant overall association with ever- vs. never-consumption [36]. Finally, the studies included for this pooled analyses were made up from melanomas diagnosed between 1979 and 1993. Methods to collect information on alcohol intake and other potential confounding factors have not changed substantially, and we have that no grounds to believe findings are not valid.
In conclusion, our findings from eight case–control studies in women showed a weak positive association between ever consuming alcohol and melanoma occurrence, which was similar across types of alcohol. However, our results did not show increasing risk with increasing alcohol consumption in pre- or post-menopausal women and irrespective of anatomic site or histologic subtype of the lesion, or presence of nevi.
References
Australian Institute of Health and Welfare (AIHW), Australasian Association of Cancer Registries (AACR) (2012) Cancer in Australia: an overview, vol Cancer series no. 74. Cat. no. CAN 70. AIHW, Canberra
Bataille V, Bishop J, Sasieni P, Swerdlow A, Pinney E, Griffiths K, Cuzick J (1996) Risk of cutaneous melanoma in relation to the numbers, types and sites of naevi: a case-control study. Br J Cancer 73:1605–1611
Bliss JM, Ford D, Swerdlow AJ, Armstrong BK, Cristofolini M, Elwood JM, Green A, Holly EA, Mack T, MacKie RM (1995) Risk of cutaneous melanoma associated with pigmentation characteristics and freckling: systematic overview of 10 case-control studies. The International Melanoma Analysis Group (IMAGE). Int J Cancer 62:367–376
Boniface S, Shelton N (2013) How is alcohol consumption affected if we account for under-reporting? A hypothetical scenario. Eur J Public Health 23:1076–1081. doi:10.1093/eurpub/ckt016
Dosemeci M, Wacholder S, Lubin JH (1990) Does nondifferential misclassification of exposure always bias a true effect toward the null value? Am J Epidemiol 132:746–748
Elwood JM, Whitehead SM, Davison J, Stewart M, Galt M (1990) Malignant melanoma in England: risks associated with naevi, freckles, social class, hair colour, and sunburn. Int J Epidemiol 19:801–810. doi:10.1093/ije/19.4.801
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin D, Forman D, Bray F (2013) GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. International Agency for Research on Cancer. http://globocan.iarc.fr. Accessed 03 March 2015
Fone DL, Farewell DM, White J, Lyons RA, Dunstan FD (2013) Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ Open. doi:10.1136/bmjopen-2012-002337
Ford D, Bliss JM, Swerdlow AJ, Armstrong BK, Franceschi S, Green A, Holly EA, Mack T, Mackie RM, Østerlind A, Walter SD, Peto J, Easton DF (1995) Risk of cutaneous melanoma associated with a family history of the disease. Int J Cancer 62:377–381. doi:10.1002/ijc.2910620403
Gallagher R, Elwood J, Hill G, Coldman A, Threlfall W, Spinelli J (1985) Reproductive factors, oral contraceptives and risk of malignant melanoma: western Canada Melanoma Study. Br J Cancer 52:901–907
Giovannucci E, Stampfer MJ, Colditz GA, Manson JE, Rosner BA, Longnecker MP, Speizer FE, Willett WC (1993) Recall and selection bias in reporting past alcohol consumption among breast cancer cases. Cancer Causes Control 4:441–448
Green A, Bain C (1985) Hormonal factors and melanoma in women. Med J Aust 142:446–448
Harrison RA, Haque AU, Roseman JM, Soong S-J (1998) Socioeconomic characteristics and melanoma incidence. Ann Epidemiol 8:327–333. doi:10.1016/S1047-2797(97)00231-7
Hausauer AK, Swetter SM, Cockburn MG, Clarke CA (2011) Increases in melanoma among adolescent girls and young women in California: trends by socioeconomic status and UV radiation exposure. Arch Dermatol 147:783–789. doi:10.1001/archdermatol.2011.44
Holland B, Welch AA, Unwin ID, Buss DH, Paul AA, Southgate DAT (1991) McCance and Widdowson’s The Composition of Foods, 5th edn. Cambridge
Holly EA, Cress RD, Ahn DK (1995) Cutaneous melanoma in women. III. Reproductive factors and oral contraceptive use. Am J Epidemiol 141:943–950
Holman CD, Armstrong BK, Heenan PJ (1984) Cutaneous malignant melanoma in women: exogenous sex hormones and reproductive factors. Br J Cancer 50:673–680
Idorn LW, Wulf HC (2014) Socioeconomic status and cutaneous malignant melanoma in Northern Europe. Br J Dermatol 170:787–793. doi:10.1111/bjd.12800
International Agency for Research on Cancer (IARC) (2012) Radiation: a review of human carcinogens, vol. 100D. The International Agency for Research on Cancer, Lyon, France
Karagas MR, Stukel TA, Dykes J, Miglionico J, Greene MA, Carey M, Armstrong B, Elwood JM, Gallagher RP, Green A, Holly EA, Kirkpatrick CS, Mack T, Osterlind A, Rosso S, Swerdlow AJ (2002) A pooled analysis of 10 case-control studies of melanoma and oral contraceptive use. Br J Cancer 86:1085–1092
Kirkpatrick CS, White E, Lee JAH (1994) Case-control study of malignant melanoma in Washington State: II. diet, alcohol, and obesity. Am J Epidemiol 139:869–880
Klatsky AL (2008) Invited commentary: never, or hardly ever? It could make a difference. Am J Epidemiol 168:872–875. doi:10.1093/aje/kwn192
Kubo J, Henderson M, Desai M, Wactawski-Wende J, Stefanick M, Tang J (2014) Alcohol consumption and risk of melanoma and non-melanoma skin cancer in the Women’s Health Initiative. Cancer Causes Control 25:1–10. doi:10.1007/s10552-013-0280-3
Langholz B, Richardson J, Rappaport E, Waisman J, Cockburn M, Mack T (2000) Skin characteristics and risk of superficial spreading and nodular melanoma (United States). Cancer Causes Control 11:741–750. doi:10.1023/A:1008952219416
Liu S, Serdula MK, Byers T, Williamson DF, Mokdad AH, Flanders WD (1996) Reliability of alcohol intake as recalled from 10 years in the past. Am J Epidemiol 143:177–186
MacKie RM, Hole DJ (1996) Incidence and thickness of primary tumours and survival of patients with cutaneous malignant melanoma in relation to socioeconomic status. BMJ 312:1125–1128. doi:10.1136/bmj.312.7039.1125
Østerlind A, Tucker MA, Stone BJ, Jensen OM (1988) The Danish case-control study of cutaneous malignant melanoma. IV. No association with nutritional factors, alcohol, smoking or hair dyes. Int J Cancer 42:825–828. doi:10.1002/ijc.2910420604
Roerecke M, Greenfield TK, Kerr WC, Bondy S, Cohen J, Rehm J (2011) Heavy drinking occasions in relation to ischaemic heart disease mortality—an 11–22 year follow-up of the 1984 and 1995 US National Alcohol Surveys. Int J Epidemiol 40:1401–1410. doi:10.1093/ije/dyr129
Rota M, Pasquali E, Bellocco R, Bagnardi V, Scotti L, Islami F, Negri E, Boffetta P, Pelucchi C, Corrao G, La Vecchia C (2014) Alcohol drinking and cutaneous melanoma risk—a systematic review and dose-risk meta-analysis. Br J Dermatol 170:1021–1028. doi:10.1111/bjd.12856
Saladi RN, Nektalova T, Fox JL (2010) Induction of skin carcinogenicity by alcohol and ultraviolet light. Clin Exp Dermatol 35:7–11. doi:10.1111/j.1365-2230.2009.03465.x
Schmidt LA, Mäkelä P, Rehm J, Room R (2010) Alcohol: equity and social determinants. In: Blas E, Kurup AS (eds) Equity, social determinants and public health programmes. WHO Press, Switzerland, pp 11–30
Smith MA, Fine JA, Barnhill RL, Berwick M (1998) Hormonal and reproductive influences and risk of melanoma in women. Int J Epidemiol 27:751–757. doi:10.1093/ije/27.5.751
Stukel TA, Demidenko E, Dykes J, Karagas MR (2001) Two-stage methods for the analysis of pooled data. Stat Med 20:2115–2130. doi:10.1002/sim.852
Swerdlow AJ, English J, MacKie RM, O’Doherty CJ, Hunter JA, Clark J, Hole DJ (1986) Benign melanocytic naevi as a risk factor for malignant melanoma. Br Med J (Clin Res Ed) 292:1555–1559
U.S. Department of Agriculture. Agricultural Research Service (1998) USDA National Nutrient Database for Standard Reference. Nutrient Data Laboratory Home Page. http://www.ars.usda.gov/nuteintdata Release 12
van der Pols JC (2014) Alcoholic drinks and skin cancer–boozing on the beach and beyond. Br J Dermatol 171:1295–1296. doi:10.1111/bjd.13456
Wilkens LR, Hankin JH, Yoshizawa CN, Kolonel LN, Lee J (1992) Comparison of long-term dietary recall between cancer cases and noncases. Am J Epidemiol 136:825–835. doi:10.1093/aje/136.7.825
Willet W (1998) Nutritional Epidemiology, 2nd edn. Oxford University Press, New York
World Cancer Research Fund/American Institute of Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. American Institute of Cancer Research (AICR), Washington, DC
Zanetti R, Franceschi S, Rosso S, Bidoli E, Colonna S (1990) Cutaneous malignant melanoma in females: the role of hormonal and reproductive factors. Int J Epidemiol 19:522–526
Acknowledgments
The IMAGE group members are: Bruce Armstrong, Veronique Bataille, Marianne Berwick, J Mark Elwood, Richard P Gallagher, Adèle C Green, Elizabeth A Holly, Margaret R Karagas, Connie S Kirkpatrick, Thomas Mack, Anne Østerlind, Stephano Rosso, and Anthony J Swerdlow.
This study was supported by the National Institutes of Health, National Cancer Institute R01 CA62345. KM was supported by a National Health and Medical Research Council of Australia (NHMRC) Program Grant (No. 552429). EAH was supported by National Cancer Institute grant R01-CA34382. MRK was supported by the National Institutes of General Medicine grant P20 GM104416. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study formal consent is not required.
Additional information
On behalf of the International Melanoma Analysis Group (IMAGE) authors. Members of International Melanoma Analysis Group (IMAGE) are listed in “Acknowledgments”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Miura, K., Zens, M.S., Peart, T. et al. Alcohol consumption and risk of melanoma among women: pooled analysis of eight case–control studies. Arch Dermatol Res 307, 819–828 (2015). https://doi.org/10.1007/s00403-015-1591-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-015-1591-x