Abstract
Sleep disordered breathing [snoring and obstructive sleep apnea–hypopnea syndrome (OSAHS)] is common in the US and has been associated with negative health outcomes. There has been no long-term prospective study on the association between sleep disordered breathing and psoriasis risk. We prospectively evaluated the association between OSAHS and snoring and incident psoriasis and psoriatic arthritis (PsA) in 71,598 women over an 11-year period (1997–2008) in the Nurses’ Health Study. Participants received follow-up questionnaires every 2 years and were asked about snoring, diagnosis of OSAHS, and diagnosis of psoriasis and PsA. We studied individuals who reported data on snoring and OSAHS prior to the diagnosis of psoriasis or PsA. We used Cox proportional hazards to calculate age-adjusted and multivariate risk ratios. Over the follow-up period, there were 524 cases of psoriasis. Women with OSAHS were more likely to have a higher BMI, be hypertensive, have cardiovascular disease, and have type 2 diabetes (p < 0.001 for all). The age-adjusted relative risk (RR) of psoriasis among women with OSAHS was 2.19 (95 % CI 1.39–3.45), the multivariate RR was 1.93 (95 % CI 1.21–3.08). Further adjusting for night shift work, hypertension, cardiovascular disease, and type 2 diabetes, the multivariate RR was 1.91 (95 % CI 1.20–3.05). There was no effect modification by BMI (p = 0.52), hypertension (p = 0.34), or snoring (p = 0.91). OSAHS was not associated with an increased risk of PsA. Although women with OSAHS were more likely to be snorers, we did not find a statistically significant relationship between snoring and the risk of confirmed psoriasis. In this study, we found that women with OSAHS had a significantly increased risk of psoriasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disordered breathing (SDB) is a spectrum of disease comprised of snoring and the obstructive sleep apnea–hypopnea syndrome (OSAHS) [19]. SDB is a relatively common problem in the United States; about 50 % of adults in the United States snore regularly, 20 % have mild-moderate OSAHS, and 6–7 % have severe OSAHS [4, 5, 10, 23]. OSAHS is thought to be on the more severe end of the SDB continuum. The burden of SDB in the United States has significant health and quality of life consequences [4, 5].
OSAHS is characterized by episodic reduction or cessation of air flow during sleep [5, 23]. OSAHS can lead to adverse health outcomes, daytime sleepiness, psychosocial problems, decreased cognitive function, and decreased quality of life [5]. OSAHS has also been found to increase the risk of cardiovascular and cerebrovascular disease as well as diabetes and metabolic syndrome [4, 24]. Risk factors for OSAHS include large body habitus, craniofacial and upper airway anatomic abnormalities, and cigarette smoking [23].
SDB is considered a systemic inflammatory disorder [4, 5, 19, 24]. Evidence suggests that systemic levels of TNF-α, IL-6, VEGF, C-reactive protein, and pro-inflammatory reactive oxygen species are increased in individuals with SDB [4, 5, 19, 24]. The etiology of the elevations in pro-inflammatory cytokines is thought to be greater expression of transcription factors such as NF-κB and HIF-1α [4, 5, 24]. The systemic inflammatory milieu created by SDB is thought to play a role in the adverse health effects associated with the condition [4, 5, 19, 24].
Psoriasis is a systemic inflammatory disorder, and it has been posited that systemic inflammation can play a role in the development of the condition [13]. Moreover, the severity of psoriatic disease has been correlated with the level of inflammatory cytokines, such as TNF-α [1]. Therefore, the elevation of inflammatory cytokines and VEGF in OSAHS may predispose individuals to develop psoriasis by acting at various points in the cycle of interaction between the innate and adaptive immune responses and keratinocytes [13]. Specifically, cytokines such as TNF-α and IL-6 activate myeloid dendritic cells. Activated myeloid dendritic cells produce IL-12 and IL-23, which activate Th1 and Th17 cells. This causes activation of keratinocytes, which leads to keratinocyte proliferation and the production of more inflammatory cytokines. These cytokines perpetuate an inflammatory cycle by activating macrophages, plasmacytoid dendritic cells, and NKT cells, which are all important parts of the innate immune response. Additionally, VEGF is thought to play an important role in the vascular changes associated with psoriasis. These changes include tortuous and leaky blood vessels, which promote the extravasation of inflammatory cells. Ultimately, the inflammatory activation and the changes to the microvasculature caused by OSAHS may promote the pathogenesis of psoriasis [13].
There has been some research into the impact of sleep on dermatologic disease and the impact of psoriasis on sleep, and one study investigating the relationship between OSAHS and psoriasis [8, 9, 14, 17, 18, 21]. This study followed individuals for a 3-year period and found that individuals with OSAHS were more likely than those without OSAHS to be diagnosed with psoriasis [21]. However, this study was a relatively small study with a relatively small sample size, did not control for important covariates, and was conducted in a Taiwanese population. Given the current burden of SDB in the United States and its associated negative health effects, a better understanding of the association between SDB and psoriasis is important from a public health perspective as well as for optimal management of both conditions. Therefore, we sought to determine the relationship between sleep disordered breathing and risk of psoriasis in a population of US women. We hypothesized that sleep apnea would be associated with an increased risk of psoriasis.
Materials and methods
Study population
The Nurses’ Health Study (NHS) is a prospective cohort study that began in 1976 with 121,700 female registered nurses from 11 states in the United States aged 30–55 years. Participants completed baseline questionnaires in 1976 and have subsequently completed questionnaires every 2 years. The information collected includes lifestyle factors, medical history, and diet. The follow-up rate is approximately 90 % for each 2-year period. This study has been approved by the Partners HealthCare Human Research Committee and informed consent was previously obtained from all study participants when they agreed to participate. We began follow-up in 1986 for snoring, 1997 for sleep apnea, and 1986 for average sleep duration, the first years in which corresponding information on each of these variables was available.
Identification of psoriasis cases
Participants in the NHS were asked if they had ever been diagnosed with psoriasis in 2008. They were also asked when their diagnosis had been made and were given the following answer choices: 1997 and before, 1998–2001, 2002–2005, 2006–2007, 2008 and later. Follow-up for psoriasis began in 1996. Self-reported psoriasis diagnosis was validated using a mailed, previously validated questionnaire [6, 7]. Psoriatic arthritis was asked in the same fashion as psoriasis, and the risk of self-reported psoriatic arthritis was also analyzed [6, 7].
Assessment of sleep apnea, snoring, and sleep duration
NHS participants were asked if they had ever been diagnosed by a physician with sleep apnea in 2008. They were also asked when their diagnosis had been made if they indicated a diagnosis of sleep apnea (1997 and before, 1998–2001, 2002–2005, 2006–2007, 2008 and later).
Participants in the NHS were asked if they snored in 1986, 2000, 2002, and 2008. The answer choices provided were: every night, most nights, a few nights a week, occasionally, almost never, and don’t know.
Participants in NHS were asked “On average, over a 24 hour period, do you sleep” or “How many total hours of actual sleep do you get in a 24-hr period?” The answer choices were ≥5, 6, 7, 8, 9, and 10+ h, and some years 11+ h was included. This question was asked in 1986, 2000, 2002, and 2008. A previous study has validated this question using a sleep diary and showed that the reported sleep data closely matched that in a 1-week sleep diary [15]. The reference group was 7 h because previous studies have found that all-cause and disease-specific morbidity and mortality is lowest in the range of 6–7 h of sleep per night [2, 3, 15, 16, 20, 22, 25].
Multivariate models simultaneously adjusted for age (continuous by year), BMI (continuous), current smoking status (yes or no), hypertension (yes or no), cardiovascular disease (defined as history of myocardial infarction, angina pectoris, congestive heart failure, and peripheral artery disease), type 2 diabetes (yes or no), and history of night shift work (yes or no).
Individuals who responded to the sleep apnea or snoring questions and had not reported a pre-existing diagnosis of psoriasis or PsA were included in this study. We excluded individuals who had a diagnosis of psoriasis prior to their diagnosis of sleep apnea or report of snoring. Individuals who were diagnosed with psoriasis within 2 years of their onset of snoring or sleep apnea diagnosis were also excluded to ensure that we only studied individuals who had a diagnosis of OSAHS before a diagnosis of psoriasis. Finally, we excluded individuals with missing data on snoring, psoriasis, weight, and height.
Statistical analyses
The primary exposure was diagnosis of sleep apnea and the secondary exposures were snoring and average sleep duration. The participants contributed person-time from the point of return of their follow-up questionnaires indicating a diagnosis of sleep apnea, snoring, or average sleep duration. Accumulation of time stopped at report of diagnosis with psoriasis or the end of study follow-up (whichever came first). Cox proportional hazards models were used to calculate risk ratios (RRs) and 95 % confidence intervals (CIs) for developing psoriasis using sleep apnea, snoring, and sleep duration status. In the multivariate analysis, we controlled for age, body mass index (BMI), smoking status, and physical activity. We also performed multivariate analysis that controlled for the aforementioned covariates and history of hypertension, cardiovascular disease, type 2 diabetes, and night shift work. We conducted pre-specified analyses of interaction by BMI, hypertension, and snoring (when not the main exposure). We also analyzed the risk of self-reported psoriatic arthritis in the same manner. Self-reported cases were used because of the low number of confirmed cases of psoriatic arthritis in the cohort. Proportionality testing was done to ensure that the proportional hazards assumption was not violated.
Results
Study population characteristics
In this study, a total of 71,598 women were included. For sleep apnea, there was a combined 844,733 person-years of follow-up, for snoring there was a combined 515,883 person-years of follow-up, and for sleep duration there was a combined 771,028 person-years of follow-up. The median follow-up time was 10 years. Individuals with sleep apnea were more likely to be snorers (p < 0.001), have a higher BMI (p < 0.001), be hypertensive (p < 0.001), have cardiovascular disease (p < 0.001), and have type 2 diabetes mellitus (p < 0.001) (Table 1).
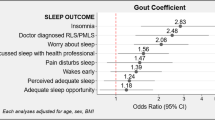
Obstructive sleep apnea–hypopnea syndrome and psoriasis risk
Compared to individuals without sleep apnea, those with sleep apnea had a higher age-adjusted and multivariate risk of developing psoriasis (Table 2). Of the 524 women who responded to the sleep apnea question and developed psoriasis, 504 indicated that they did not have sleep apnea and 20 of the women indicated that they had been diagnosed with sleep apnea. The age-adjusted RR for developing psoriasis in women with sleep apnea was 2.19 (95 % CI 1.39–3.45), the multivariate RR was 1.93 (95 % CI 1.21–3.08), and the multivariate RR that further adjusted for night shift work and hypertension, cardiovascular disease, and type 2 diabetes mellitus was 1.91 (95 % CI 1.20–3.05). Interaction analysis revealed no effect modification by BMI (p = 0.52), hypertension (p = 0.34), or snoring (p = 0.91) on the relationship between obstructive sleep apnea and psoriasis risk.
Snoring and psoriasis risk
In total, 353 women assessed for snoring developed psoriasis during the study period. Compared to non-snorers, individuals snoring a few nights per week, most nights, and every night had an increased age-adjusted risk of developing psoriasis, but no relationship between snoring and psoriasis was seen with multivariate analysis (Table 2). There was no material difference between the two multivariate models. For occasional snorers, the age-adjusted RR for developing psoriasis was 1.11 (95 % CI 0.85–1.43) and the multivariate RR that took night shift work and selected comorbid diseases into account was 1.04 (95 % CI 0.80–1.35). For those who snored a few nights per week, the age-adjusted RR for developing psoriasis was 1.37 (95 % CI 0.91–2.06) and multivariate RR (simultaneously adjusting for night shift work and selected comorbid diseases) was 1.25 (95 % CI 0.83–1.88). For individuals snoring most nights, the age-adjusted RR for developing psoriasis was 1.43 (95 % CI 1.02–2.01) and the multivariate RR that took night shift work and selected comorbid diseases into account was 1.24 (95 % CI 0.88–1.75). For every night snorers, the age-adjusted RR for developing psoriasis was 1.32 (95 % CI 0.86–2.05) and the multivariate RR was 1.10 (95 % CI 0.71–1.73). Interaction analysis revealed no effect modification by BMI (p = 0.92) or hypertension (p = 0.99) on the association between snoring and psoriasis.
Sleep duration and psoriasis risk
We found no association between incident psoriasis and average sleep duration in age-adjusted or multivariate models (Table 3).
Obstructive sleep apnea and psoriatic arthritis risk
We found an increased age-adjusted risk of developing psoriatic arthritis among individuals with OSAHS, but there was no significant difference after adjusting for age, BMI, smoking status, exercise, hypertension, cardiovascular disease, type 2 diabetes, and history of night shift work (Online Resource 1). Twenty-three women who were assessed for snoring developed psoriatic arthritis. We found that snoring was not associated with risk of psoriatic arthritis (Online Resource 1).
Discussion
In this study, we sought to prospectively evaluate the relationship between SDB and psoriasis. We found an association between OSAHS and incident psoriasis. This relationship persisted in two multivariate models that considered other known risk factors for psoriasis and SDB, demonstrating an association between these two entities. Although women with sleep apnea were more likely to be snorers, we found no association between snoring and psoriasis.
A recent study suggested a relationship between OSAHS and psoriasis [21]. The study included a group of 2,250 Japanese individuals with OSAHS, but without psoriasis, and 11,255 matched controls with neither OSAHS nor psoriasis. The individuals were followed for 3 years for a diagnosis of psoriasis. After adjusting for monthly income, urbanization level, geographic location, and obesity, the study authors found a hazard ratio of developing psoriasis of 2.30 (95 % CI 1.13–4.69; p = 0.022) times greater if individuals had OSAHS [21]. This study had a relatively short duration given the fact that both OSAHS and psoriasis are chronic conditions that are thought to develop over years. Additionally, the authors of this study did not address other potential confounders such as cigarette smoking. Our study follows individuals for a longer period of time and uses two multivariate models that both simultaneously adjust for risk factors for OSAHS and psoriasis. Although we cannot account for all unmeasured confounding, we included all known risk factors for both conditions into our models.
SDB has been associated with multiple comorbidities—including diabetes and cardiovascular disease—through a proposed mechanism of systemic inflammation [4, 11, 12, 19, 24]. Individuals with OSAHS have been found to have higher levels of inflammatory cytokines such as TNF-α, IL-1, and IL-6 [4, 5, 19, 24]. These cytokines are also elevated in individuals with psoriasis [1, 13]. We propose that the elevation in inflammatory cytokines may contribute to the manifestation of a psoriasis phenotype in an individual who is predisposed to developing psoriasis.
Together, snoring and OSAHS comprise a spectrum of SDB [19]. Since OSAHS is on the more severe end of the continuum of SDB, individuals with this condition may have the greatest elevations in cytokines [19]. This may help to explain why we observed an increased risk of psoriasis in women with OSAHS, but did not see the same relationship in women who snored.
There are several strengths and limitations to our study. To our knowledge, this is the largest prospective assessment of SDB and psoriasis. The diagnosis of OSAHS and psoriasis was self-reported, however, psoriasis diagnoses have been validated and their accuracy has been demonstrated, making the likelihood of misclassification low [6, 7]. The fact that our study is restricted to female registered nurses represents both a strength and a weakness. Since these participants are well-educated women, there is less socioeconomic variability in our cohort and there is a high rate of response. Our results do not necessarily represent the female population in the United States. Our study is limited by the relatively small PsA case number, which hampers our statistical power to assess the association between SDB and PsA. Furthermore, we are not able to infer a relationship between SDB and psoriasis in men based on this study. However, while the prevalence of SDB and psoriasis in our study may not reflect that of all individuals in the United States, we expect the biological relationship between SDB and psoriasis to be similar among women and men. Finally, the age of individuals in our cohort more closely reflects the second peak of the bimodal pattern of psoriasis incidence, so these results may be most applicable to psoriasis that onsets later in life.
This prospective study has demonstrated that women with OSAHS are at an approximately twofold increased risk of developing psoriasis. Physicians should be aware of the association between OSAHS and psoriasis. Our results suggest that managing SDB, and in particular OSAHS, may be a potential target for preventing and managing psoriasis, although our study did not examine this question directly.
References
Arican O, Aral M, Sasmaz S, Ciragil P (2005) Serum levels of TNF-alpha, IFN-gamma, IL-6, IL-8, IL-12, IL-17, and IL-18 in patients with active psoriasis and correlation with disease severity. Mediat Inflamm 2005:273–279
Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, Patel S, Hu FB (2003) A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 26:380–384
Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, Hu FB (2003) A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med 163:205–209
Calvin AD, Albuquerque FN, Lopez-Jimenez F, Somers VK (2009) Obstructive sleep apnea, inflammation, and the metabolic syndrome. Metab Syndr Relat Disord 7:271–278
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP (2010) Pathophysiology of sleep apnea. Physiol Rev 90:47–112
Dominguez PL, Assarpour A, Kuo H, Holt EW, Tyler S, Qureshi AA (2009) Development and pilot-testing of a psoriasis screening tool. Br J Dermatol 161:778–784
Dominguez PL, Husni ME, Holt EW, Tyler S, Qureshi AA (2009) Validity, reliability, and sensitivity-to-change properties of the psoriatic arthritis screening and evaluation questionnaire. Arch Dermatol Res 301:573–579
Gezer O, Batmaz I, Sariyildiz MA, Sula B, Ucmak D, Bozkurt M, Nas K (2014) Sleep quality in patients with psoriatic arthritis. Int J Rheum Dis. doi:10.1111/1756-185X.12505
Gowda S, Goldblum OM, McCall WV, Feldman SR (2010) Factors affecting sleep quality in patients with psoriasis. J Am Acad Dermatol 63:114–123
Hiestand DM, Britz P, Goldman M, Phillips B (2006) Prevalence of symptoms and risk of sleep apnea in the US population: results from the national sleep foundation sleep in America 2005 poll. Chest 130:780–786
Hu FB, Willett WC, Colditz GA, Ascherio A, Speizer FE, Rosner B, Hennekens CH, Stampfer MJ (1999) Prospective study of snoring and risk of hypertension in women. Am J Epidemiol 150:806–816
Hu FB, Willett WC, Manson JE, Colditz GA, Rimm EB, Speizer FE, Hennekens CH, Stampfer MJ (2000) Snoring and risk of cardiovascular disease in women. J Am Coll Cardiol 35:308–313
Nestle FO, Kaplan DH, Barker J (2009) Psoriasis. N Engl J Med 361:496–509
Papadavid E, Vlami K, Dalamaga M, Giatrakou S, Theodoropoulos K, Gyftopoulos S, Stavrianeas N, Papiris S, Rigopoulos D (2013) Sleep apnea as a comorbidity in obese psoriasis patients: a cross-sectional study. Do psoriasis characteristics and metabolic parameters play a role? J Eur Acad Dermatol Venereol 27:820–826
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB (2004) A prospective study of sleep duration and mortality risk in women. Sleep 27:440–444
Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB (2006) Correlates of long sleep duration. Sleep 29:881–889
Shutty BG, West C, Huang KE, Landis E, Dabade T, Browder B, O’Neill J, Kinney MA, Feneran AN, Taylor S, Yentzer B, McCall WV, Fleischer AB Jr, Feldman SR (2013) Sleep disturbances in psoriasis. Dermatol Online J 19:1
Stinco G, Trevisan G, Piccirillo F, Di Meo N, Nan K, Deroma L, Bergamo S, Patrone P (2013) Psoriasis vulgaris does not adversely influence the quality of sleep. G Ital Dermatol Venereol 148:655–659
Svensson M, Venge P, Janson C, Lindberg E (2012) Relationship between sleep-disordered breathing and markers of systemic inflammation in women from the general population. J Sleep Res 21:147–154
von Ruesten A, Weikert C, Fietze I, Boeing H (2012) Association of sleep duration with chronic diseases in the European prospective Investigation into cancer and nutrition (EPIC)-Potsdam study. PLoS One 7:e30972
Yang YW, Kang JH, Lin HC (2012) Increased risk of psoriasis following obstructive sleep apnea: a longitudinal population-based study. Sleep Med 13:285–289
Yeo Y, Ma SH, Park SK, Chang SH, Shin HR, Kang D, Yoo KY (2013) A prospective cohort study on the relationship of sleep duration with all-cause and disease-specific mortality in the Korean multi-center cancer cohort study. J Prev Med Public Health 46:271–281
Young T, Skatrud J, Peppard PE (2004) Risk factors for obstructive sleep apnea in adults. JAMA 291:2013–2016
Zamarron C, Garcia Paz V, Riveiro A (2008) Obstructive sleep apnea syndrome is a systemic disease. Current evidence. Eur J Intern Med 19:390–398
Zhang X, Giovannucci EL, Wu K, Gao X, Hu F, Ogino S, Schernhammer ES, Fuchs CS, Redline S, Willett WC, Ma J (2013) Associations of self-reported sleep duration and snoring with colorectal cancer risk in men and women. Sleep 36:681–688
Acknowledgments
We are deeply indebted to the participants and staff of the Nurses’ Health Study for their valuable contributions. This work was funded by the National Psoriasis Foundation Medical Dermatology Research Fellowship (JMC), the Department of Dermatology, Brigham and Women’s Hospital, Boston, Massachusetts and National Institutes of Health (NIH) grant R01 CA50385.
Conflict of interest
Dr. Qureshi serves as a consultant for Abbvie, Amgen, the Centers for Disease Control, Janssen, Merck, Novartis, and Pfizer and is an investigator for Amgen. Mr. Cohen, Dr. Jackson, and Ms. Li have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cohen, J.M., Jackson, C.L., Li, T.Y. et al. Sleep disordered breathing and the risk of psoriasis among US women. Arch Dermatol Res 307, 433–438 (2015). https://doi.org/10.1007/s00403-015-1536-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-015-1536-4