Abstract
Psoriasis is characterized by hyperproliferation and abnormal differentiation of keratinocytes, and inflammation. 1,25-Dihydroxyvitamin D3, which is used for the treatment of psoriasis, binds to vitamin D receptor (VDR) and modulates gene transcription. We analyzed VDR gene FokI, ApaI and TaqI polymorphisms in 51 Turkish familial psoriasis patients (psoriasis vulgaris and psoriatic arthritis) and 100 healthy subjects, and evaluated the correlation between VDR genotypes and calcipotriol response. We found that the TT genotype was significantly more frequent in the patients than in the controls (51 vs. 35%: P ≤ 0.05). The frequency of the T allele in patients was also significantly higher than that in the controls (73.5 vs. 59.5%: P ≤ 0.025). In psoriatic arthritis patients, T allele frequency was even higher (91.7%: P ≤ 0.05). With regard to response to calcipotriol treatment, in nonresponsive patients TT genotype and T allele frequencies were higher than they were in the controls (63.6 vs. 35%: P ≤ 0.025, 81.8 vs. 59.5%: P ≤ 0.01, respectively). In conclusion, we show that VDR gene TaqI polymorphism is associated with familial psoriasis in the Turkish population. We also demonstrate that VDR gene polymorphisms may play a role in partial resistance to calcipotriol therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psoriasis is a common chronic recurrent inflammatory skin condition characterized by hyperproliferation of the keratinocytes and affects about 2% of the world’s population. The etiology of psoriasis is affected by genetic, immunologic and environmental factors. It causes disruption in the normal events of cell maturation and proliferation [9].
The active metabolite of vitamin D (1,25-dihydroxyvitamin D3) analogs such as calcipotriol are known to be effective in the treatment of psoriasis [8]. It has been demonstrated that calcipotriol upregulates vitamin D receptor (VDR) in human keratinocytes in vivo [16]. In addition to the classical action on calcium homeostasis and bone metabolism, calcipotriol inhibits proliferation and induces terminal differentiation of keratinocytes [20]. It has been reported that cultured fibroblasts and keratinocytes from psoriatic patients exhibit partial resistance to calcipotriol mediated anti-proliferative activity, and response to calcipotriol treatment has been shown to vary among these patients [11]. VDR gene polymorphisms may explain this variable responsiveness [3, 7, 10, 12].
VDR, the receptor of 1,25-dihydroxyvitamin D3, is a member of the steroid/thyroid hormone receptor superfamily, which is a group of ligand-dependent transcription factors. The receptor-hormone complex binds to hormone response elements in regulatory regions of target genes and changes the gene transcription [2]. The VDR gene is localized to 12q12-14, consists of 11 exons, and spans 75 kb. Several polymorphisms in the VDR gene have been reported. FokI (F,f), which is a protein synthesis start codon polymorphism, is located in exon 2. In intron 8 BsmI (B,b) and ApaI (A,a) polymorphisms are described. The other polymorphic site in exon 9 is TaqI (T,t) [1].
In this study, we analyzed VDR gene FokI, ApaI and TaqI polymorphisms to determine whether they could be considered as one of the susceptibility genes for familial psoriasis in Turkish patients. We also investigated whether VDR genotypes were associated with calcipotriol responsiveness.
Materials and methods
Patients
A total of 51 unrelated Turkish psoriasis patients (22 males and 29 females, age range 14–78 years, mean age 38.5 years) recruited from different geographical regions of Turkey were referred to the Hacettepe University, Faculty of Medicine, Department of Dermatology. Among them, 45 had psoriasis vulgaris and 6 had psoriatic arthritis. All patients had a family history of psoriasis and 49 had an early onset not later than 40 years of age. The patients were clinically evaluated using the psoriasis area and severity index (PASI). The normal control population consisted of 100 unrelated Turkish healthy subjects (52 males and 48 females, age range 8–48 years, mean age 18 years) randomly recruited from different geographical regions to mirror the psoriasis patients in terms of geographic location. All control subjects and psoriasis patients originated from Anatolia.
Calcipotriol treatment
Among the 51 patients, 47 (42 psoriasis vulgaris and 5 psoriatic arthritis) agreed to receive topical calcipotriol treatment and their clinical responses were evaluated. None of the psoriatic arthritis patients received immunosuppressive treatment. Patients were instructed to apply calcipotriol (Psorcutan, Intendis, 50 μg/g) to the specific site twice a day. After 8 weeks of treatment, patients with point improvement less than 40% and more than 40% were classified as nonresponsive and responsive, respectively.
VDR gene polymorphism analysis
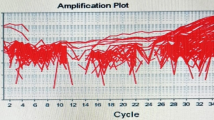
DNA was extracted from white blood cells by salting out [13]. VDR gene polymorphic FokI site (exon 2) and ApaI and TaqI polymorphic sites (intron 8-exon 9) were amplified by PCR. The primers 5′AGC TGG CCC TGG CAC TGA CTC TGC TCT3′ and 5′ATG GAA ACA CCT TGC TTC TTC TCC CTC3′ were used to amplify exon 2, and 5′CAG AGC ATG GAC AGG GAG CAA3′ and 5′GCA ACT CCT CAT GGC TGA GGT CTC3′ were used to amplify intron 8-exon 9. The PCR conditions were 35 cycles at 94°C for 30 s for denaturation, 30 s at 60°C for annealing and 30 s at 72°C for extension. Exon 2 PCR products were digested with FokI restriction endonuclease enzyme at 37°C for 1 h, and intron 8-exon 9 PCR products were digested with ApaI at 37°C for 2 h and with TaqI at 65°C for 1 h. The digested products were run on agarose gel containing EtBr and visualized under UV fluorescence [5, 17].
Statistical analysis
Differences between the controls and psoriasis patients were analyzed using the chi-square test. P values less than 0.05 were regarded as statistically significant. Allele frequencies were calculated from genotype frequencies on the basis of Hardy-Weinberg equilibrium with the chi-square test.
Results
The genotype and allele frequencies for FokI, ApaI and TaqI polymorphisms are shown in Tables 1 and 2. The presence of FokI, ApaI and TaqI restriction sites was defined as “f” (196, 69 bp), “a” (490, 210 bp), and “t” (290, 245, 205 bp), respectively, and the absence of the sites was defined as “F” (265 bp), “A” (700 bp) and “T” (490, 245 bp). Figure 1 shows the results of TaqI, ApaI and FokI restriction enzyme digestion.
Comparison of the VDR genotypes between the controls and psoriasis patients revealed significant difference in the TaqI site, but not in the ApaI and FokI sites. Frequencies for TT, Tt and tt genotypes were 51, 45.1 and 3.9% in the psoriasis group, and 35, 49 and 16% in the control group, respectively. We found a significantly higher proportion of patients with the TT genotype (P ≤ 0.05). Derived allele frequencies for T and t alleles were 73.5 and 26.5% in the psoriasis group and 59.5 and 40.5% in the control group. The observed and expected genotypic proportions of FokI, ApaI and TaqI polymorphisms were in the Hardy-Weinberg equilibrium in both groups. The frequency of the T allele in patients was significantly higher than that in the controls (P ≤ 0.025). In addition, this predisposition was even higher (91.7%) in psoriatic arthritis patients (P ≤ 0.05). No significant difference was found in ApaI and FokI allele frequencies (P ≤ 1).
Of the 51 patients recruited, 47 completed the 8-week calcipotriol treatment protocol. While 25 patients responded to treatment, 22 showed no response. Table 3 shows VDR genotype frequencies in responsive and nonresponsive patients. Compared with the control group, significant differences were observed only for the TaqI genotype and allele frequencies. In nonresponsive patients, the TT genotype and T allele were higher in frequency than they were in the controls (63.6 vs. 35%: P ≤ 0.025, 81.8 vs. 59.5%: P ≤ 0.01, respectively). The allele frequencies for FokI, ApaI and TaqI polymorphisms of responsive patients were also compared to those of nonresponsive patients, but no significant association was found (P > 0.05).
Discussion
There have been a number of studies to investigate whether VDR gene polymorphisms could be a risk factor for the development of psoriasis in different populations [4, 6, 14, 15, 18, 19]. We analyzed VDR gene ApaI, TaqI, and FokI polymorphisms, the relationship between these polymorphisms and response to calcipotriol treatment in familial Turkish psoriasis patients from Hacettepe University, Department of Dermatology, which is a referral center for patients all over Turkey.
Among the polymorphisms analyzed, we found that TaqI polymorphism was associated with psoriasis. The frequencies of the TT genotype and T allele were higher in the patients than they were in the control group. Previous studies on psoriasis and the VDR gene have demonstrated both non-significant [7, 10, 12, 14, 18] and significant associations, although involving different polymorphisms [3, 15, 19]. It is known that VDR genotype distribution varies dramatically due to the ethnic composition and genetic background of the populations. Similar to our results, as in the earlier studies in Japanese psoriasis patients, the frequency of the TT genotype was found to be higher in patients than in controls (87 vs. 74%, P < 0.05). They also showed that there was no significant difference in the frequency of ApaI genotypes between the two groups [19]. However, Park et al. [15] reported a higher frequency of AA and Aa genotypes in Korean psoriasis patients compared to controls (AA: 9.6 vs. 2.9%, Aa: 44.2 vs. 27.9%). They also observed that this tendency was more accentuated in psoriasis patients with early onset. Because of ethnic and geographical differences, the conflicting findings between these studies and ours are not unexpected.
Before our study, there was only one report, by Kaya et al., that investigated the association between VDR gene polymorphism and Turkish psoriasis patients. They demonstrated an association between aa/Aa genotypes and 53 psoriasis patients compared to 54 normal controls (AA: 26.4 vs. 50%, Aa: 58.5 vs. 38.9%, aa: 15.1 vs. 11%) [6]. However, our study showed that there was no significant difference in ApaI polymorphism between Turkish patients and controls (AA: 23.5 vs. 30%, Aa: 56.9 vs. 55%, aa: 19.6 vs. 15%, P ≤ 1). The apparent discrepancy between these earlier results and ours may be explained in two ways. First, the size of the control population is rather high in our study. Second, Turkey has distinct geographical regions with diverse climatic, cultural, social, economic and genetic differences, and this diversity in the country’s population makes genetic studies difficult [21]. Patients from different geographical regions of Turkey are concentrated mainly at the Hacettepe University, which is located in the capital, in central Turkey. Therefore, this coordinator university reflects the heterogeneous genetic composition of the whole country’s population.
To investigate whether there was a correlation between VDR genotypes and types of psoriasis, we compared the genotypes of 45 psoriasis vulgaris and 6 psoriatic arthritis patients with those of normal controls. In the psoriatic arthritis patients, the frequency of the T allele was 91.7% and in psoriasis vulgaris patients it was 71.1%. Although the number of psoriatic arthritis patients examined is small, our study is the first to report that in familial psoriatic arthritis patients, the frequency of the T allele was significantly higher than that in the controls. No significant differences were found in ApaI and FokI alleles.
The VDR belongs to the steroid/thyroid receptor superfamily and interacts with target-cell nucleus to produce a variety of biologic effects. It is found on the cells of many different tissues, including the thyroid, bone, kidney and T cells of the immune system [2]. T cells are known to play a role in psoriasis and it is thought that the binding of calcipotriol, the physiologically active form of vitamin D, to the VDR modulates the T cells gene transcription of cell differentiation and proliferation related genes. The mechanism of calcipotriol in remitting psoriasis is not well understood [20].
We suggested that the alleles of the polymorphic regions of the VDR gene may be related to responsiveness or nonresponsiveness to calcipotriol treatment. In the present study, we found that the TT genotype and T allele were significantly higher in the nonresponsive group compared to the controls. It is known that the clinical response of psoriasis patients to vitamin D3 is correlated with the level of expression of VDR mRNA, and some psoriatic patients have partial resistance to vitamin D3 mediated antiproliferative activity [11, 12]. Therefore, it could be suggested that Turkish psoriasis patients harboring the T allele show resistance to calcipotriol treatment. Among the six psoriatic arthritis patients, three were not responsive to treatment. Since psoriatic arthritis involves both joint and connective tissue inflammation, the nonresponsiveness of these patients to calcipotriol might be related to the heterogeneity and severity of this type of psoriasis. Besides topical treatment, these patients could receive systemic immunosuppressive agents that might improve clinical response. So far, the role of VDR polymorphism analysis in predicting clinical response to calcipotriol was demonstrated only in a few studies. It has previously been suggested by Halsall et al. [4] that F and T alleles were positively associated with calcipotriol response in psoriasis patients, but only the TT genotype was significant. On the other hand, Saeki et al. [19] stated that the FF genotype and F allele were lower in nonresponsive patients than in controls, with regard to the response to tacalcitol topical treatment. According to our results, the TT genotype and T allele were significantly more frequent in the nonresponsive group compared to the controls, which is in conflict with these previous findings. The discrepancy between the studies might be a result of the use of different therapeutic agents in different concentrations, the sizes of the population and the different genetic backgrounds of the populations studied.
In the present study, we found that VDR gene TaqI polymorphism is associated with a risk of developing psoriasis in the Turkish population. By demonstrating an association between TaqI polymorphism and psoriasis, we provide evidence on the genetic susceptibility in Turkish familial psoriasis patients. The association between the TT genotype and calcipotriol nonresponsiveness reported in this study may also support previous findings on partial resistance to calcipotriol treatment.
References
Audi L, Garcia-Ramirez M, Carrascosa A (1999) Genetic determinants of bone mass. Horm Res 51:105–123
DeLuca HF, Zierold C (1998) Mechanisms and functions of vitamin D. Nutr Rev 56:4–10
Giomi B, Ruggiero M, Fabbri P, Gulisano M, Peruzzi B, Caproni M, Pacini S (2005) Does the determination of the Bb vitamin D receptor genotype identify psoriasis vulgaris patients responsive to topical tacalcitol? J Dermatol Sci 37:180–181
Halsall JA, Osborne JE, Pringle JH, Hutchinson PE (2005) Vitamin D receptor gene polymorphisms, particularly the novel A-1012G promoter polymorphism, are associated with vitamin D3 responsiveness and non-familial susceptibility in psoriasis. Pharmacogenet Genomics 15:349–355
Harris SS, Eccleshall TR, Gross C, Dawson-Hughes B, Feldman D (1997) The vitamin D receptor start codon polymorphism (FokI) and bone mineral density in premenopausal American black and white women. J Bone Miner Res 12:1043–1048
Kaya TI, Erdal ME, Tursen U, Camdeviren H, Gunduz O, Soylemez F, Ikizoglu G (2002) Association between vitamin D receptor gene polymorphism and psoriasis among the Turkish population. Arch Dermatol Res 294:286–289
Kontula K, Valimaki S, Kainulainen K, Viitanen AM, Keski-Oja J (1997) Vitamin D receptor polymorphism and treatment of psoriasis with calcipotriol. Br J Dermatol 136:977–978
Kragballe K, Gjertsen BT, De Hoop D, Karlsmark T, van de Kerkhof PC, Larko O, Nieboer C, Roed-Petersen J, Strand A, Tikjob G (1991) Double-blind, right/left comparison of calcipotriol and betamethasone valerate in treatment of psoriasis vulgaris. Lancet 337:193–196
Krueger GG, Bergstresser PR, Lowe NJ, Voorhees JJ, Weinstein GD (1984) Psoriasis. J Am Acad Dermatol 11:937–947
Lee DY, Park BS, Choi KH, Jeon JH, Cho KH, Song KY, Kim IG, Youn JI (2002) Vitamin D receptor genotypes are not associated with clinical response to calcipotriol in Korean psoriasis patients. Arch Dermatol Res 294:1–5
MacLaughlin JA, Gange W, Taylor D, Smith E, Holick MF (1985) Cultured psoriatic fibroblasts from involved and uninvolved sites have a partial but not absolute resistance to the proliferation-inhibition activity of 1,25-dihydroxyvitamin D3. Proc Natl Acad Sci USA 82:5409–5412
Mee JB, Cork MJ (1998) Vitamin D receptor polymorphism and calcipotriol response in patients with psoriasis. J Invest Dermatol 110:301–302
Miller SA, Dykes DD, Polesky HF (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16:1215
Okita H, Ohtsuka T, Yamakage A, Yamazaki S (2002) Polymorphism of the vitamin D(3) receptor in patients with psoriasis. Arch Dermatol Res 294:159–162
Park BS, Park JS, Lee DY, Youn JI, Kim IG (1999) Vitamin D receptor polymorphism is associated with psoriasis. J Invest Dermatol 112:113–116
Reichrath J, Muller SM, Kerber A, Baum HP, Bahmer FA (1997) Biologic effects of topical calcipotriol (MC 903) treatment in psoriatic skin. J Am Acad Dermatol 36:19–28
Riggs BL, Nguyen TV, Melton LJ 3rd, Morrison NA, O’Fallon WM, Kelly PJ, Egan KS, Sambrook PN, Muhs JM, Eisman JA (1995) The contribution of vitamin D receptor gene alleles to the determination of bone mineral density in normal and osteoporotic women. J Bone Miner Res 10:991–996
Ruggiero M, Gulisano M, Peruzzi B, Giomi B, Caproni M, Fabbri P, Pacini S (2004) Vitamin D receptor gene polymorphism is not associated with psoriasis in the Italian Caucasian population. J Dermatol Sci 35:68–70
Saeki H, Asano N, Tsunemi Y, Takekoshi T, Kishimoto M, Mitsui H, Tada Y, Torii H, Komine M, Asahina A, Tamaki K (2002) Polymorphisms of vitamin D receptor gene in Japanese patients with psoriasis vulgaris. J Dermatol Sci 30:167–171
Smith EL, Walworth NC, Holick MF (1986) Effect of 1 alpha,25-dihydroxyvitamin D3 on the morphologic and biochemical differentiation of cultured human epidermal keratinocytes grown in serum-free conditions. J Invest Dermatol 86:709–714
Tunçbilek E (1997) Genetic services in Turkey. Eur J Hum Genet 5:178–182
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dayangac-Erden, D., Karaduman, A. & Erdem-Yurter, H. Polymorphisms of vitamin D receptor gene in Turkish familial psoriasis patients. Arch Dermatol Res 299, 487–491 (2007). https://doi.org/10.1007/s00403-007-0782-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-007-0782-5