Abstract
MAGE-3 or MAGE-A3 is one of the best-characterized tumor antigens. Due to its tumor-restricted expression pattern and its recognition by both cytotoxic and helper T cells it constitutes a promising tumor antigen for anticancer immunotherapy, notably of malignant melanoma. Surprisingly, however, only very limited information is available on the frequency and consistency of its expression in metastatic melanoma lesions. We have now investigated the presence of MAGE-A3 mRNA in 316 tumor samples from 147 melanoma patients by RT-PCR. MAGE-A3 mRNA was detectable in 62% of metastases, and expression did not depend on the site of the metastases (skin, lymph node, and internal organs), age, sex, or duration of disease. Southern blot hybridization of the PCR product enhanced sensitivity of detection, and 26% more samples (13/50 samples tested) scored positive, indicating an even higher MAGE-A3 mRNA frequency than determined by simple ethidium bromide gel analysis. In 62 patients, we were able to investigate MAGE-A3 expression in several metastases from the same patient, and unexpectedly, both MAGE-A3-positive and MAGE-A3-negative metastases were found in 32% of these patients (20 of 62). Immunohistochemistry (using mAb 57B) demonstrated that the expression pattern was usually also heterogeneous with positively and negatively stained tumor cells within one metastasis. However, most (90%) of the metastases (47/52) gave a partially positive signal. Taken together, MAGE-A3 is a common and frequent tumor antigen in metastasized melanoma, but its expression is often heterogeneous.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Therapy of stage IV melanoma is still frustrating. Over the past decades all chemotherapeutic approaches to curing metastasized melanoma have failed. Hence, tumor immunotherapy, especially in melanoma, has gained increasing attention and promising success has been obtained. In the search for promising targets suitable for an immunotherapeutic approach, many melanoma-associated tumor antigens have been identified in recent years, including cancer testis antigens (CTA), differentiation antigens, mutational antigens, overexpressed proteins and others. The ability of several of these antigens to induce T cell immune responses in melanoma patients and the development of immunogenic cancer vaccines targeting these antigens has brought them into the focus of many tumor immunologists. Out of the extensive group of tumor-associated antigens, CTA are one of the most attractive candidates for immunotherapy. Two main reasons account for this: (1) in adults CTA are almost exclusively expressed in neoplastic tissue and testis (an immune-privileged organ without MHC I expression), and (2) their expression has been repeatedly documented in metastatic melanoma [1–6].
After the isolation of the prototype CTA MAGE-1 (melanoma-associated gene-1) by CTL epitope cloning [7] (subsequently renamed MAGE-A1), various additional members of the MAGE gene family and many other CTAs have been isolated by other techniques such as serological expression cloning (SEREX), differential RNA analysis, and database mining [4, 8]. To date, more than 20 CTA or CTA families have been identified and their number is still growing. MAGE-A3 is a member of the MAGE-A family (MAGE-A1 to MAGE-A12) and is of particular interest to cancer immunologists since several T cell epitopes (HLA I and HLA II) have been characterized [1, 8, 9]. In addition, anti-MAGE-A3 immunotherapy has been shown to be beneficial in the treatment of metastasized melanoma [10–21]. The expression of the tumor antigen MAGE-A3 is not restricted to melanoma, but is well-documented for many malignant tumors including lung, bladder, breast, as well many other carcinomas and sarcomas [3, 4, 6].
Currently, only few data exist on the frequency of MAGE-A3 expression in melanoma metastases [2, 22]. In the current study, we analyzed its frequency in 316 metastases by MAGE-A3-specific RT-PCR with or without additional hybridization and by immunohistochemistry. For the analysis of protein expression, the monoclonal antibody (mAb) 57B was used which recognizes MAGE-A3 [23], but also MAGE-A1, -4, -6 and -12 [24, 25]. Our investigation included, in contrast to others, analysis of different metastases from the same patient and metastases from different organs.
Tumor samples, materials and methods
Unfixed, fresh tumor specimens (n=316) obtained from 147 patients (56% male, 44% female, median age 52.5 years) with stage IV melanoma (AJCC/UICC) were analyzed. Out of these metastases, 73% (230) were localized to the skin, 17% (54) to lymph nodes, and 10% (32) to other organs. All patients were informed and gave written consent (according to the local Ethics Committee protocols). Tumor specimens were immediately frozen in liquid nitrogen and stored at −80°C. Sections stained with hematoxylin-eosin (H&E) from these cryo-blocks were reviewed to verify the diagnosis, and assess the presence of representative tumor material. From 52 of the 316 metastases, a small portion of the tumor was formalin-fixed and paraffin-embedded following standard procedures for further immunohistochemical analyses.
RNA isolation, c-DNA synthesis, and polymerase chain reaction (RT-PCR)
Total RNA was isolated from frozen tumor samples using an RNeasy Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocol, and digested with RNAse free DNAse (Life Technologies, Karlsruhe, Germany). DNAse-treated RNA (2 μg) was reverse-transcribed into cDNA using Superscript (Life Technologies). The reaction was performed in the presence of 2 μM oligo(dT)15 and 0.5 mM dNTP in the supplied reaction buffer for 1 h at 42°C and stopped by boiling for 5 min. cDNA (3 μl) was used as a template for PCR. As a control for cDNA synthesis, GAPDH-PCR was performed with the following primers: GAPDH sense 5′-CAC CAC CAT GGA GAA GGC TGG-3′, GAPDH antisense 5′-GAA GTC AGA GGA GAC CAC CTG-3′ (398 bp). The MAGE-A3 PCR reaction included 0.4 μM MAGE-A3-specific sense (5′-TGG AGG ACC AGA GGC CCC C-3′) and antisense (5′-GGA CGA TTA TCA GGA GGC CTG C-3′) primers (725 bp), 200 μM dNTP, 2.5 U Taq polymerase (Amersham Pharmacia Biotech, Freiburg, Germany) in the supplied reaction buffer in a final volume of 50 μl. The PCR cycling conditions for MAGE-A3 were 1 min at 94°C and 4 min at 72°C, and for GAPDH 45 s at 94°C, 45 s at 60°C and 1.5 min at 72°C. MAGE-A3 PCR was carried out for 40 cycles; the GAPDH PCR for 30 cycles. PCR cycling included an initial 4-min denaturation step at 94°C and a final 15-min extension at 72°C. Aliquots of PCR reactions were loaded on 1.6% agarose gels and stained with ethidium bromide.
Southern blot hybridization of MAGE-A3 mRNA RT-PCR products
A subset of tumor samples (50/120) testing negative for MAGE-A3 mRNA on ethidium bromide gels were additionally investigated by hybridization with a MAGE-A3-specific probe. Only a subset could be analyzed since after performing the experiments with the ethidium bromide gel and the confirmation tests, in most cases no RNA or corresponding tumor tissue was left. Thus, this subset was selected purely by chance with the only limiting criterion being whether or not enough RNA was available. For Southern blot analysis, the PCR products were loaded on agarose gels and blotted onto nitrocellulose. Hybridization was performed according to standard protocols in 50% formamide at 42°C. The full-length MAGE-A3 cDNA was labeled with [32P]α-dATP using a Random Prime DNA labeling kit (Boehringer Mannheim, Mannheim, Germany) and used as probe. The filter was washed at 65°C three times with 2×SSC (standard sodium citrate), 0.1% sodium dodecyl sulfate (SDS) and twice with 1×SSC, 0.1% SDS. Bands were visualized by autoradiography.
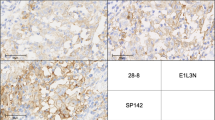
Immunohistochemistry
Immunohistochemistry was performed using paraffin-embedded tissue blocks (n=52). Sections of thickness 5 μm were deparaffinized and antigens retrieved by heating the sections in a microwave oven for 10 min in a buffer solution comprising 10 mM citric acid and 100 mM sodium citrate. The antibody mAb 57B (kindly provided by Dr. G. Spagnoli, Basel, Switzerland) was used to detect MAGE-A expression (MAGE-A1, -3, -4, -6 and -12, see above) at a working dilution of 1:25. Omission of the first antibody and isotype control stainings served as controls. Following antibody incubation for 60 min, the sections were incubated with a biotinylated secondary antibody and a streptavidin-horseraddish peroxidase using the ultraTech AP streptavidin-biotin system (Coulter-Immunotech Diagnostics, Germany). Finally, the signal was visualized by application of the AEC chromogen. Sections were counterstained with hematoxylin for 2 min, rinsed and coverslipped using Aquatex (Merck, Darmstadt, Germany). Two independent investigators (C.R. and P.D.) blinded to the antibodies reviewed each slide using a Leitz microscope to assess the percentage of positively stained cells. The results were categorized: negative, no staining; focal, single cells or small clusters of cells (fewer than 5%) stained positive; +, 5–25% of melanoma cells stained positive; ++, 25–50% of melanoma cells stained positive; +++, 50–75% of melanoma cells stained positive; ++++, >75% of melanoma cells positive.
Results
MAGE-A3 mRNA is frequently found in melanoma metastases
We investigated the presence of MAGE-A3 mRNA in 316 tumor samples from 147 patients with malignant melanoma by RT-PCR (Table 1). The overall frequency of MAGE-A3 mRNA in 316 metastases was 62% (196/316). No significant difference was found in the analysis of cutaneous/subcutaneous metastases (63%, 145/230), lymph node metastases (65%, 35/54), and internal organ metastases (mostly liver, samples were retrieved by fine needle puncture; 53%, 17/32). In 62 patients more than one metastasis was removed and tested. The vast majority of these patients had multiple skin melanoma metastases (n=51) due to their easy availability. Of these 62 patients, 7 had multiple lymph node metastases, and in 4 patients more than one internal organ metastasis was analyzed. MAGE-A3 RNA detection was unstable in 32% (20 of 62) of these patients with MAGE-A3-positive and MAGE-A3-negative metastases. Of these 20 patients, 17 had multiple skin metastases which were either positive or negative for MAGE-A3, 2 had multiple lymph node metastases, either positive or negative, and 1 had different internal organ metastases (lung and liver) which varied in their MAGE-A3 positivity. MAGE-A3 positivity of all tested metastases derived from the same patient was found in only 44% (27/62), and negativity in 24% (15/62). No significant influence of sex or age was noted. Furthermore, MAGE-A3 mRNA detection in the analyzed metastases was independent of the histological type of the primary melanoma (i.e., superficial spreading, nodular, acral lentiginous, or lentigo maligna; data not shown) and of the cytology of the tumor cells.
Frequency of MAGE-A3 expression is independent of the time between primary melanoma and metastases excision
We further investigated whether the time between the excision of the primary melanoma and the appearance of the analyzed metastasis had an influence on the frequency of MAGE-A3 mRNA detection by RT-PCR (Table 2). Data were available for 193 of our tumor samples. Of these 193 metastases, 118 occurred within 3 years after excision of the primary melanoma and MAGE-A3 mRNA was detected 60% (71/118). For metastases occurring after up to 5 years, MAGE-A3 was found in 68% (26/38), after up to 10 years in 56% (15/27), and after more than 10 years in 70% (7/10). Unfortunately, we could not analyze the corresponding primary melanomas. However, the time to metastasis occurrence seems to be without influence on the MAGE-A3 positivity.
Southern blot hybridization technique improves the detection of MAGE-A3 mRNA RT-PCR products
Fifty tumor samples (out of 120) which were negative for MAGE-A3 in the ethidium bromide gel analysis underwent further investigation by Southern blot hybridization using a MAGE-3-specific DNA probe. Interestingly, for 26% (13/50) of these metastases the presence of MAGE-A3 mRNA was demonstrated with this more sensitive detection method (Fig. 1). Thus, the frequency of MAGE-A3 mRNA expression in melanoma metastases appears to be even higher than determined by RT-PCR and ethidium bromide gel analysis (Tables 1 and 2). Unfortunately, we could not perform Southern blot analysis in all 120 samples. However, projecting the data from these 50 tumor samples tested by Southern blotting to all 120 negative samples, about 31 would be positive. Projecting the data to all 316 metastases, 227 (72%) would be positive. Thus, MAGE-A3 mRNA is frequently present in melanoma metastases and the prerequisite of a high expression frequency is fulfilled. One has to admit, however, that MAGE-A3 is expressed heterogeneously and that MAGE-A3-positive and MAGE-A3-negative metastases can be found in the same patient.
MAGE-A protein is frequently expressed in melanoma metastases
MAGE-A expression was investigated in 52 paraffin-embedded tumor samples simultaneously by immunohistochemistry using the mAb 57B. Of these 52 metastases, 17 were negative for MAGE-A3 (by RT-PCR) and 35 showed the presence of MAGE-A3 mRNA. In accordance to previous findings, a heterogeneous MAGE-A expression pattern was seen in the tumor cells (Fig. 2). Results of the immunohistochemical staining for MAGE-A were as follows (Table 3): of the 52 metastases, 5 were negative, 4 were focally positive, 9 were +, 10 were ++, 17 were +++, and 7 were ++++. Of the 52 tumor samples, only 5 failed to show at least in part MAGE-A expression at the protein level. All these five metastases were also negative in the PCR/ethidium bromide gel analysis. Three of these five metastases were also negative by Southern blot analysis. Interestingly, some metastases were negative for MAGE-A3 by PCR/ethidium bromide gel analysis and positive by immunohistochemistry (n=12). Since the mAb 57B was used for the stainings, this discrepancy is not surprising, as this mAb recognizes MAGE-A3, but detects MAGE-A1, -4, -6 and -12 more strongly, as delineated above. The primary peptide which is detected by this mAb seems to be MAGE-A4. Of these 12 metastases (negative by PCR, positive by immunohistochemistry), seven were subjected to Southern blot analysis and two were positive for MAGE-A3 by this more sensitive approach. Taken together, the frequency of MAGE-A detection by immunohistochemistry in these 52 melanoma metastases is surprisingly high.
Discussion
Recent efforts to find new and more successful treatment regimens for metastasized melanoma have focused on immunotherapeutic strategies. Several clinical findings, including spontaneous partial or complete regression of primary tumors and even distant metastases, development of vitiligo, and occurrence of metastases after more than 10 years, suggest that the patients’ immune system is actively involved in the course and outcome of melanoma. The clinically observed high immunogenicity of melanomas is further underlined by the detection of CD4/CD8 T-cell responses against defined tumor antigens in untreated melanoma patients [26, 27]. Given the fact that the immune system is capable of destroying whole organs (e.g., in graft-versus-host disease), the current challenges of cancer immunotherapy are to direct and employ the immune response in an effective way resulting in tumor cell lysis which overcomes tolerance and escape mechanisms [28, 29].
Several factors determine whether a tumor antigen is suitable and valuable for use as a target for an immunotherapy. Among these, frequency of its expression is a fundamental prerequisite. In this study, we investigated more than 300 melanoma metastases for their MAGE-A3 expression. We were especially interested in MAGE-A3 as it is a well-established and promising target in immunotherapy of melanoma [10–21]. We showed that MAGE-A3 mRNA is frequently found in melanoma metastases. By RT-PCR and Southern blot hybridization, the presence of MAGE-A3 mRNA in metastatic melanoma lesions was found in at least 70% of tumor specimens. Using the mAb 57B, which recognizes MAGE-A3 but is now also known to recognize some other MAGE-A antigens [23–25], the presence of MAGE-A at the protein level was almost 90%. No significant correlation with sex, age or duration of disease was found. It was also unimportant whether metastases were localized to the skin, lymph nodes, or internal organs. Furthermore, tumor cell cytology appeared to be irrelevant to the detection of MAGE-A3.
In 62 patients, we were also able to investigate MAGE-A3 expression in several metastases from the same patient. This is important as previously no information on a possible variation from one metastasis to another had been available in the literature. Remarkably, about one-third had MAGE-A3-positive and MAGE-A3-negative tumor samples. This is in accord with the reportedly typical heterogeneous immunohistochemical staining pattern for CTA [2, 4, 22, 23, 30] seen within a given metastasis. Even in the case of heterogeneous expression, targeting of MAGE-A3 may be useful, of course, notably if other antigens are targeted by vaccination as well. Effective partial tumor lysis mediated by MAGE-A3-specific T cells can in addition also lead to an epitope spreading with the creation of new effective antitumor T cell responses (T. Boon, personal communication).
Due to their easy accessibility, mainly skin metastases were analyzed in our study. In metastatic cells from lymph nodes, however, an equal frequency of MAGE-A3 expression was found. The frequency of MAGE-A3 expression in internal organs (mainly liver) was a little lower, yet this may also have been due to the sampling problem inherent in analyzing fine needle biopsy specimens. Amplification products that were negative in the ethidium bromide gel after RT-PCR were additionally subjected to Southern blotting using radioactively labeled MAGE-A3 cDNA. Due to the higher sensitivity of this technique, lower amounts of mRNA could be detected. It was nevertheless interesting that a significant 26% of the RT-PCR-negative tumor samples turned out to be positive by the additional hybridization.
Transcription does not necessarily mean that the corresponding protein is actually translated and presented on MHC molecules. The possibility of using specific antibodies would therefore be principally advantageous to the RT-PCR technique. To date, several anti-MAGE-A antibodies have been described including mAb 57B, mAb 6C1, and others. However, antibodies detecting single MAGE-A proteins only exist for MAGE-A1 (mAb MA454, mAb 77B) and MAGE-A4 (mAb R5) [31]. This is most probably due to the high homology of the MAGE-A genes. A MAGE-A3-specific antibody (mAb M3H67) has been suggested but has not yet been validated [32].
In summary, our study shows that the majority of melanoma metastases express MAGE-A3. Due to this high frequency, MAGE-A3 is, apart from its immunological suitability, clearly a practically relevant tumor rejection antigen which is worth pursuing in this respect. It is furthermore an interesting candidate for a cocktail of different target antigens which would ensure on a statistical basis that at least one antigen is expressed in any metastasis. Our findings that within the same patient some metastases can be MAGE-A3-negative while others are positive and that MAGE-A3 is expressed heterogeneously within one metastasis, however, strongly suggest that vaccinating solely against MAGE-A3 is likely to be incomplete in metastasized melanoma.
References
Boon T, van der Bruggen P (1996) Human tumor antigens recognized by T lymphocytes. J Exp Med 183:725–729
Brasseur F, Rimoldi D, Lienard D, Lethe B, Carrel S, Arienti F, Suter L, Vanwijck R, Bourlond A, Humblet Y (1995) Expression of MAGE genes in primary and metastatic cutaneous melanoma. Int J Cancer 63:375–380
Kirkin AF, Dzhandzhugazyan KN, Zeuthen J (2002) Cancer/testis antigens: structural and immunobiological properties. Cancer Invest 20:222–236
Scanlan MJ, Gure AO, Jungbluth AA, Old LJ, Chen YT (2002) Cancer/testis antigens: an expanding family of targets for cancer immunotherapy. Immunol Rev 188:22–32
Smith C, Cerundolo V (2001) Immunotherapy of melanoma. Immunology 104:1–7
Zendman AJ, Ruiter DJ, van Muijen GN (2003) Cancer/testis-associated genes: identification, expression profile, and putative function. J Cell Physiol 194:272–288
van der Bruggen P, Traversari C, Chomez P, Lurquin C, De Plaen E, van den Eynde B, Knuth A, Boon T (1991) A gene encoding an antigen recognized by cytolytic T lymphocytes on a human melanoma. Science 254:1643–1647
van den Eynde B, Peeters O, De Backer O, Gaugler B, Lucas S, Boon T (1995) A new family of genes coding for an antigen recognized by autologous cytolytic T lymphocytes on a human melanoma. J Exp Med 182:689–698
Gaugler B, van den Eynde B, van der Bruggen P, Romero P, Gaforio JJ, De Plaen E, Lethe B, Brasseur F, Boon T (1994) Human gene MAGE-3 codes for an antigen recognized on a melanoma by autologous cytolytic T lymphocytes. J Exp Med 179:921–930
Banchereau J, Palucka AK, Dhodapkar M, Burkeholder S, Taquet N, Rolland A, Taquet S, Coquery S, Wittkowski KM, Bhardwaj N, Pineiro L, Steinman R, Fay J (2001) Immune and clinical responses in patients with metastatic melanoma to CD34(+) progenitor-derived dendritic cell vaccine. Cancer Res 61:6451–6458
Coulie PG, Karanikas V, Lurquin C, Colau D, Connerotte T, Hanagiri T, Van Pel A, Lucas S, Godelaine D, Lonchay C, Marchand M, van Baren N, Boon T (2002) Cytolytic T-cell responses of cancer patients vaccinated with a MAGE antigen. Immunol Rev 188:33–42
Gajewski TF, Fallarino F, Ashikari A, Sherman M (2001) Immunization of HLA-A2+ melanoma patients with MAGE-3 or MelanA peptide-pulsed autologous peripheral blood mononuclear cells plus recombinant human interleukin 12. Clin Cancer Res 7:895s–901s
Hersey P, Menzies SW, Halliday GM, Nguyen T, Farrelly ML, DeSilva C, Lett M (2004) Phase I/II study of treatment with dendritic cell vaccines in patients with disseminated melanoma. Cancer Immunol Immunother 53:125–134
Mackensen A, Herbst B, Chen JL, Kohler G, Noppen C, Herr W, Spagnoli GC, Cerundolo V, Lindemann A (2000) Phase I study in melanoma patients of a vaccine with peptide-pulsed dendritic cells generated in vitro from CD34(+) hematopoietic progenitor cells. Int J Cancer 86:385–392
Marchand M, Punt CJ, Aamdal S, Escudier B, Kruit WH, Keilholz U, Hakansson L, van Baren N, Humblet Y, Mulders P, Avril MF, Eggermont AM, Scheibenbogen C, Uiters J, Wanders J, Delire M, Boon T, Stoter G (2003) Immunisation of metastatic cancer patients with MAGE-3 protein combined with adjuvant SBAS-2: a clinical report. Eur J Cancer 39:70–77
Marchand M, van Baren N, Weynants P, Brichard V, Dreno B, Tessier MH, Rankin E, Parmiani G, Arienti F, Humblet Y, Bourlond A, Vanwijck R, Lienard D, Beauduin M, Dietrich PY, Russo V, Kerger J, Masucci G, Jager E, De Greve J, Atzpodien J, Brasseur F, Coulie PG, van der Bruggen P, Boon T (1999) Tumor regressions observed in patients with metastatic melanoma treated with an antigenic peptide encoded by gene MAGE-3 and presented by HLA-A1. Int J Cancer 80:219–230
Marchand M, Weynants P, Rankin E, Arienti F, Belli F, Parmiani G, Cascinelli N, Bourlond A, Vanwijck R, Humblet Y (1995) Tumor regression responses in melanoma patients treated with a peptide encoded by gene MAGE-3. Int J Cancer 63:883–885
Palucka AK, Dhodapkar MV, Paczesny S, Burkeholder S, Wittkowski KM, Steinman RM, Fay J, Banchereau J (2003) Single injection of CD34+ progenitor-derived dendritic cell vaccine can lead to induction of T-cell immunity in patients with stage IV melanoma. J Immunother 26:432–439
Schuler-Thurner B, Schultz ES, Berger TG, Weinlich G, Ebner S, Woerl P, Bender A, Feuerstein B, Fritsch PO, Romani N, Schuler G (2002) Rapid induction of tumor-specific type 1 T helper cells in metastatic melanoma patients by vaccination with mature, cryopreserved, peptide-loaded monocyte-derived dendritic cells. J Exp Med 195:1279–1288
Thurner B, Haendle I, Roder C, Dieckmann D, Keikavoussi P, Jonuleit H, Bender A, Maczek C, Schreiner D, von den DP, Brocker EB, Steinman RM, Enk A, Kampgen E, Schuler G (1999) Vaccination with mage-3A1 peptide-pulsed mature, monocyte-derived dendritic cells expands specific cytotoxic T cells and induces regression of some metastases in advanced stage IV melanoma. J Exp Med 190:1669–1678
Weber JS, Hua FL, Spears L, Marty V, Kuniyoshi C, Celis E (1999) A phase I trial of an HLA-A1 restricted MAGE-3 epitope peptide with incomplete Freund’s adjuvant in patients with resected high-risk melanoma. J Immunother 22:431–440
Jungbluth AA, Busam KJ, Kolb D, Iversen K, Coplan K, Chen YT, Spagnoli GC, Old LJ (2000) Expression of MAGE-antigens in normal tissues and cancer. Int J Cancer 85:460–465
Hofbauer GF, Schaefer C, Noppen C, Boni R, Kamarashev J, Nestle FO, Spagnoli GC, Dummer R (1997) MAGE-3 immunoreactivity in formalin-fixed, paraffin-embedded primary and metastatic melanoma: frequency and distribution. Am J Pathol 151:1549–1553
Landry C, Brasseur F, Spagnoli GC, Marbaix E, Boon T, Coulie P, Godelaine D (2000) Monoclonal antibody 57B stains tumor tissues that express gene MAGE-A4. Int J Cancer 86:835–841
Rimoldi D, Salvi S, Schultz-Thater E, Spagnoli GC, Cerottini JC (2000) Anti-MAGE-3 antibody 57B and anti-MAGE-1 antibody 6C1 can be used to study different proteins of the MAGE-A family. Int J Cancer 86:749–751
Kawakami Y, Rosenberg SA (1997) Human tumor antigens recognized by T-cells. Immunol Res 16:313–339
Nagorsen D, Scheibenbogen C, Marincola FM, Letsch A, Keilholz U (2003) Natural T cell immunity against cancer. Clin Cancer Res 9:4296–4303
Rufer N, Zippelius A, Batard P, Pittet MJ, Kurth I, Corthesy P, Cerottini JC, Leyvraz S, Roosnek E, Nabholz M, Romero P (2003) Ex vivo characterization of human CD8+ T subsets with distinct replicative history and partial effector functions. Blood 102:1779–1787
Zippelius A, Batard P, Rubio-Godoy V, Bioley G, Lienard D, Lejeune F, Rimoldi D, Guillaume P, Meidenbauer N, Mackensen A, Rufer N, Lubenow N, Speiser D, Cerottini JC, Romero P, Pittet MJ (2004) Effector function of human tumor-specific CD8 T cells in melanoma lesions: a state of local functional tolerance. Cancer Res 64:2865–2873
Busam KJ, Iversen K, Berwick M, Spagnoli GC, Old LJ, Jungbluth AA (2000) Immunoreactivity with the anti-MAGE antibody 57B in malignant melanoma: frequency of expression and correlation with prognostic parameters. Mod Pathol 13:459–465
Juretic A, Spagnoli GC, Schultz-Thater E, Sarcevic B (2003) Cancer/testis tumour-associated antigens: immunohistochemical detection with monoclonal antibodies. Lancet Oncol 4:104–109
Dhodapkar MV, Osman K, Teruya-Feldstein J, Filippa D, Hedvat CV, Iversen K, Kolb D, Geller MD, Hassoun H, Kewalramani T, Coplan K, Comenzo RL, Chen YT, Jungbluth AA (2003) Expression of cancer/testis (CT) antigens MAGE-A1, MAGE-A3, MAGE-A4, CT-7, and NY-ESO-1 in malignant gammopathies is heterogeneous and correlates with site, stage and risk status of disease. Cancer Immun 3:9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roeder, C., Schuler-Thurner, B., Berchtold, S. et al. MAGE-A3 is a frequent tumor antigen of metastasized melanoma. Arch Dermatol Res 296, 314–319 (2005). https://doi.org/10.1007/s00403-004-0527-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-004-0527-7