Abstract
Purpose
Currently, accepted treatment for periprosthetic femoral fractures with loose femoral stem indicates its revision; however, recent studies have proposed treating Vancouver type B2 fractures via internal fixation without stem revision, particularly in the elderly or multi-morbid patients. Despite indications for stem revision, some surgeons tend to perform internal fixation. The main goal of this study was therefore to identify the parameters that were significantly different comparing internal fixation to stem revision for Vancouver type B2 fractures.
Methods
Eighty-one Vancouver B2 periprosthetic femoral fractures, treated between 2010 and 2019, were analysed. The internal fixation (ORIF) and the revision groups were compared. Patients’ age, BMI, American Society of Anaesthesiologists (ASA) score, anaesthesia type, operating time, blood loss, surgeons’ experience, post-operative weight-bearing, length of hospital stay, and radiological outcome using AGORA roentgenographic assessment were analysed.
Results
Patients chosen for ORIF were significantly older than those treated by stem revision (85.4 vs 75.1 years; p = 0.002). Blood loss was 390.7 and 1141.6 ml in the ORIF and revision groups, respectively (p < 0.0001). The surgical times were 134.5 and 225 min in the ORIF and revision groups, respectively (p < 0.0001). Our analysis of BMI, ASA score, anaesthesia type, length of hospital stay, surgeons’ experience and radiological outcome, were not significantly different between the two groups.
Conclusion
Revision did not exhibit better radiological results; moreover, internal fixation resulted in significantly less perioperative blood loss and a shorter operating time, concluding that ORIF is a viable alternative to revision arthroplasty, particularly in older patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip replacement is one of the most performed elective orthopaedic surgical procedures. Western civilisation is continuously aging, with the elderly population of Europe (> 65 years old) expected to double within the next 10–20 years [1]. Annually, over 800,000 new hip replacements are performed worldwide. In 2014, about 3.2% of the population aged > 55 years had an artificial joint, while another 2% required one [2]. The increasing life expectancy and number of hip arthroplasties performed—especially in younger, more active patients—elevate the statistical chance of falls, and occurrence of periprosthetic fractures [3]. Periprosthetic femoral fractures (PFFs) are becoming increasingly common and challenging, usually concerning individuals older than 78 years; naturally, their number of comorbidities is higher than in the younger population [4].
The incidence of PFFs after total hip replacement is reportedly 0.1–18% [5]; the Mayo Clinique Joint Replacement Database reports periprosthetic fractures in 1% of 23,980 primary hip replacements. Lindahl et al. previously reported a PFF rate of up to 9.5%, taken from the Swedish Hip Registry [3]. Analysing 1751 patients from the same registry, Chatziagorou et al. reported that the incidence of fractures around the femoral stem had increased from 1/1000 patients in 2001, to 1.4/1000 patients in 2011; the rate of fracture in patients aged > 80 years increased from 1.3 to 2.3 per 1000 primary total hip arthroplasties (THA) between 2001 and 2011 [6].
The Vancouver classification, described in 1995, is the most widely accepted classification for periprosthetic fractures around the femoral stem [7]. It has demonstrated high reliability and inter- and intra-observer agreement, and has been validated in numerous studies, with several advantages over other classifications; the most important being its value in establishing a surgical strategy [8,9,10,11]. Fractures with loose stems are most common; B2 and B3 type fractures are reported in 75–85% of all periprosthetic hip fractures [2, 7]. If the femoral stem is loose, classic treatment involves revision arthroplasty using cerclage, plates, strut allografts, or a combination of thereof [12].
Recent literature reports open reduction and internal fixation (ORIF) without stem revision for the treatment of type B2 PFFs, particularly in the aged population, or in patients with multiple comorbidities [13, 14]. Some advocate ORIF use due to its lesser surgical complexity, others suggest that properly re-fixed stems can osseointegrate with good results; most importantly, fewer surgery-related risks are involved in ORIF, compared with stem revision surgery [13,14,15].
We observed that surgeons within our institution tended to prefer ORIF over femoral stem revision for Vancouver B2 fractures, even though the classic approach indicates otherwise. It is unclear whether their decision to choose ORIF was intuitive, or related to a lack of experience, particularly regarding younger specialists; alternatively, it may be based on recently emerging literature supporting this treatment modality for B2 fractures.
All patients treated for Vancouver B2 PFFs were divided into two groups: those treated via stem revision, and those treated via ORIF. Our primary objective was to retrospectively analyse the parameters that were significantly different between ORIF and stem revision groups. We then examined the pre-operative parameters, including patient age, BMI, and ASA score. The intra-operative parameters—anaesthesia type, blood loss, operating time, and surgeon’s experience—were compared between the two groups. Finally, post-operative parameters including weight-bearing, length of hospital stay and radiological outcome were analysed. Our null hypothesis was that there was no difference in these parameters between the two groups.
Materials and methods
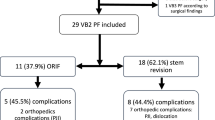
After obtaining institutional review board approval, a retrospective medical chart and radiograph review was performed on 2476 patients who underwent hemi- or total hip arthroplasty, followed up at two university hospitals. All revisions that occurred between 1st January 2010, and 15th November 2019, were studied. After excluding all other reasons for hip replacement failure, we outlined 105 periprosthetic hip fractures. All femoral fractures, except for Vancouver B2, were excluded; a total of 76 patients with 81 periprosthetic Vancouver B2 fractures around the cementless stem were included in this study. The average age of patients at the index operation was 70.7 (18–94) years, the average age at the time of PFF surgery was 76.6 (29–98) years, and the median follow-up times from the index and revision procedures were 134 (12–312) and 60 (6–111) months, respectively. Patients were divided into two groups: the revision (n = 27) and ORIF (n = 54) groups.
The revision group included patients whose primary implant was removed; a revision stem, bypassing the fracture by at least two diaphyseal diameters, was implanted. Additional hardware, such as cerclage wires or plates, was used at the surgeon’s discretion. In ORIF group, the fractures were treated by cerclage alone (n = 10), plate with screws and cerclage (n = 14), hook plate with screws and cerclage (n = 26) or by a combination of plate, strut allograft, screws and cerclage wires (n = 4). In all ORIF cases, the original stem was preserved.
Medical records
The dates of index arthroplasty and reoperation (ORIF or stem revision), and blood loss during the revision procedure, both from the surgical protocol and from the anaesthetist reports, were carefully recorded. Patients’ BMI, ASA score, and type of anaesthesia during revision surgery were analysed. The duration of the procedure, from skin incision until wound closure, was precisely calculated, and the length of hospital stay before discharge or referral to the rehabilitation centre was calculated. Furthermore, the level of experience (years) of the surgeon who performed the second intervention was analysed; all surgeons included perform at least 21 hip replacements per year.
The correlation between the surgeon’s level of experience and their tendency to choose ORIF or revision was analysed, hypothesizing that younger surgeons would favour an ORIF procedure. Following the operation, the weight-bearing protocol was reviewed. Patients were divided into seven groups: immediate full weight-bearing; 50% weight-bearing; and 2, 4, 6, 8, 12 weeks of no weight-bearing on the operated side.
Radiographic analysis
The pre- and post-operative images of the index arthroplasties were evaluated as a reference. The post-traumatic radiographs were analysed to define the extension of the fracture, level of bone comminution, subsidence, rotational displacement, and angular migration of the stem. After operation, anteroposterior, lateral, and oblique radiographs were evaluated; the AGORA Roentgenographic Assessment (ARA) score was used to evaluate fractures around the stems [16]. Published in 1995, this is a numeric score with an initial value of six, that subtracts points for each parameter that reduces the stability of the stem; results may be interpreted as excellent (5–6), good (4), fair (3), and poor (≤ 2). The ARA score correlates with the more familiar Engh score; however, the former is presumably better adapted to modern-type stems, with better discriminative capacity in the upper spectrum of the radiographic images [17].
Statistical analysis
A t test was used for independent variables, whereas categorical variables were compared using the Chi-squared test through cross-tabulation; McNemar’s test was used for the surgeon’s experience. The Mann–Whitney test was used for non-normally distributed variables; a p value < 0.05 was considered statistically significant.
Results
Medical record
Of the 2476 hip replacements followed up in our clinic, 297 (12%) arthroplasty failures were surgically treated between 1st January 2010 and 15th November 2019; 37% of failures were due to aseptic loosening, 9% due to infections, 18% due to dislocations, and ~ 1% due to technical or other reasons. A total of 105 patients were admitted to the emergency department for periprosthetic hip fracture, representing 35% of all revised failures, and 4.2% of overall hip replacements.
Of the 105 periprosthetic hip fractures, one was around the acetabulum without femoral fracture, two were Vancouver type AG, eight were type B1, 81 were type B2, nine were type B3, and 4 were type C.
Seventy-six patients were treated for 81 Vancouver B2 PFFs (male: n = 22, female: n = 59). The ORIF and revision groups included 54 and 27 fractures, respectively. The average age of patients at the index procedure was 70.7 (SD = 14.4, range: 24–88) years for both groups, and 74.3 (SD = 11.2) and 62.6 (SD = 17.2) years for the ORIF and revision groups, respectively; the average age at the second surgery was 76.6 (SD = 13.4; range: 29–98) years for both groups, and 85.4 (SD = 12.1) and 75.1 (SD = 16.6) years for the ORIF and revision groups, respectively. The ratio between the left and right hips was 44:37.
Comparing the mean age at the second surgery in the ORIF (85.4 years) and revision (75.1 years) groups, we found that the ORIF group was significantly older (p = 0.002). Patients’ BMI (p = 0.89) and ASA score (p = 0.19) did not differ significantly between the two groups, and were therefore not considered determining criteria for either ORIF (23.9) or revision (26.1). The mean lengths of hospital stay were 19.4 and 21.7 days in the ORIF and revision groups, respectively; no significant difference in hospitalization time was found between the two groups (p = 0.28).
Regarding types of anaesthesia, four possibilities were observed: epidural, epidural with femoral bloc, general, and general with femoral bloc. Although the revision group tended toward general anaesthesia, this difference was not significant (p = 0.23). The average blood loss in the ORIF group was significantly less than in the revision group, 390.7 and 1141.6 ml, respectively, p < 0.0001; (Fig. 1). The mean operating times were 225 and 134.5 min in the revision and ORIF groups, respectively (Fig. 2), which was significant (p < 0.0001).
Surgeons’ experience was calculated based on the number of years performing hip replacement surgeries. Sixteen surgeons were divided in four clusters: 1–5, 5–10, 15–20, and 25–30 years of hip arthroplasty experience; each cluster included four surgeons. These four clusters were compared to examine the correlation between level of experience and the choice between ORIF and revision surgery; no significant correlation was determined (p = 0.79).
Cross-tabulating the two groups with seven post-operative weight-bearing categories indicated significantly earlier weight-bearing in the revision group (p = 0.002).
Radiographic analysis
The pre-fracture and follow-up images, for at least 12 (mean: 91.3; range: 12–262.3) months after the index arthroplasty, were scored using ARA assessment. The ARA score following the second procedure, either ORIF or revision, was calculated based on X-rays performed 12 (mean: 36.3; range: 6–58.9) months after the procedure. Exceptions were made for three patients who died before their 12-month follow-up (images analysed six months after the procedure).
In the ORIF group, the mean ARA scores before periprosthetic fracture and after PFF fixation with ORIF were 5.25 (SD = 0.73) and 5.08 (SD = 0.92), respectively. In the revision group, the mean scores were 4.87 (SD = 1.01) after the index procedure and 4.96 (SD = 1.1) after revision.
The most frequently seen negative radiographic ARA score parameters, before periprosthetic fractures, were calcar remodelling and hypertrophy (− 2 points), initial osteolysis (− 2 points), and to a lesser extent, lucent lines in the smooth zones (− 2 points) and reactive lines in < 50% of the porous zones (− 2 points). Pedestal formation, cortical hypertrophy, migration, and interface deterioration were seen much less frequently.
After ORIF or revision procedures, the most commonly seen ARA score parameters were calcar remodelling (− 2 points), lucent lines in smooth and/or porous zones (− 2 and − 3 points, respectively), initial or progressive osteolysis (− 2 and − 4 points, respectively), and moderate migration or varus (− 2 points). Less often, severe migration (− 4 points) was observed; pedestal formation and cortical hypertrophy were rarely observed. All those parameters were present almost equally in ORIF and revision groups. The 10 cases in ORIF group treated by cerclage wires only, showed a slightly worse ARA score compared to other modalities (p = 0.35).
Case examples
Case 1
A 70-year-old male patient with periprosthetic Vancouver type B2 fracture around cementless stem. (Fig. 3). The index procedure was done 8 years prior to the fracture. At the time of fracture his BMI was 32 and ASA score 3. The patient had general anaesthesia. The blood loss was 600 ml and the operating time was 150 min. He was operated by a surgeon with 15 years of experience. The patient spent 4 days in the orthopaedic ward and 16 days in the rehabilitation centre. The patient had 8 weeks of partial weight-bearing. After the index procedure his ARA score was 6 and it remained the same at the follow-up of one and 4.5 years. The patient reported Forgotten Joint score (FJS) of 92 and Oxford Hip score (OHS) of 42 at the last visit.
Case 2
A female patient of 94 years was hospitalised with Vancouver B2 fracture around a cementless stem after a fall (Fig. 4). The index procedure was done when she was 84 years old. At the time of ORIF procedure, the patient had a BMI 22 and ASA score 3. She was operated under spinal anaesthesia. The blood loss was 450 cc and the operating time was 140 min. She was operated by a surgeon with more than 25 years of experience. The patient spent 7 days in the orthopaedic ward, then 24 days in a specialized centre for convalescence. The patient was asked to walk with toe-touch on the right side for 6 weeks. Her ARA score was a constant 6 after the index arthroplasty and at 1 and 5 years after the ORIF surgery. At 5 years’ follow-up, the FJS was 82 and the OHS was 34, she walked into the office by herself without a walking aid.
Case 3
A female patient whose hip had been replaced at the age of 82, suffered a B2 type periprosthetic fracture 19 months later (Fig. 5). The BMI was 19, ASA score 2. The patient lost 550 ml of blood during a 140-min-long surgery under general anaesthesia. She was operated by a surgeon who had finished his residency two years earlier. The patient stayed 6 days in the surgical ward and 17 days in the rehabilitation. The weight-bearing was not allowed for 12 weeks after surgery. The ARA score was 6 after the index THA. After the ORIF procedure, it decreased to 4 due to subsidence and varus migration at 1 and 3 years’ follow-up. At her latest visit, she presented FJS of 72 and OHS of 32.
Discussion
The 4.2% of PFFs in our study was within the 0.1–18% range reported in the literature [5, 6]. The percentage of revision due to aseptic loosening, dislocation, or infection was also comparable to the rates reported; however, the rate of periprosthetic fractures was 35% of all revised failures, which was somewhat higher than reported by other researchers [18]. (Table 1)
We observed a proportion of Vancouver B2 fractures comparable to those reported in the literature, representing 78% of all PFFs in our study [19]. Remarkably, all surgeons between the two university hospitals tended to prefer ORIF to revision when patients were older. Even in the relatively small cohort included in this study, we showed that the average age in the ORIF group was over 10 years higher than in the revision group (85.4 vs 75.1 years). We speculated that ORIF was chosen as the older population with PFF presents a higher number of comorbidities, often precluding more complex procedures, such as stem revision. However, the ASA score, designed to serve as an indicator for a patient’s general state, was not significantly different between the ORIF and revision groups, which does not support our speculation.
Along with the difference in age in the ORIF and revision groups, we found a significant difference in blood loss and operating time. As demonstrated by Manara et al., these two parameters are inter-related; the probability of massive blood loss increases by 3% for every minute surgery is prolonged [20]. A three times lesser blood loss and twice shorter operating time in the ORIF group cannot be overlooked; these are crucial factors in a patient’s ability to tolerate the surgery and allow for better post-operative recovery. We observed that weight-bearing was allowed earlier in the revision group, which may favour stem revision surgery. However, the weight-bearing protocol after PFF varies significantly between institutions [21].
Regarding surgical experience, the hypothesis that younger surgeons prefer ORIF due to its lesser complexity was rejected; no correlations were found between years of experience and the choice of treatment modality for type B2 PFFs. We intentionally presented the third case (Fig. 5) which showed a migration of the stem, rarely seen in our ORIF cohort. Despite the stem subsidence, the patient was satisfied with the outcome. Possibly the ORIF was a poor choice for this stem design or in this particular case, surgeon’s experience was a disadvantageous factor.
Regarding radiographic evaluation, the ARA score was a convenient, efficient, and precise tool to evaluate the radiographs of the cementless stems after ORIF or revision surgery.
We found no studies using ARA score for periprosthetic fractures in the literature. Comparing results between the index arthroplasty and second procedure, we observed a slight decline in ARA score in the ORIF group, and a small improvement in the revision group; no significant difference was observed between the two groups, probably due to the small sample size. An important observation is that patients who underwent ORIF in our study showed neither major hardware failure, nor stem migration or displacement; these potential complications are often used as an argument for stem revision. Recent data suggest that ORIF can offer results equivalent to stem revision [15]; our radiological results propose the same. Moreover, less blood loss and a shorter operating time suggest that ORIF is a viable treatment option for Vancouver B2 PFFs [2, 14].
Some points may strengthen this study; first, it would be beneficial to perform an in-depth analysis of implant type and model, and exact modality of internal fixation used, rather than simply dividing patients into ORIF and revision groups. Second, a mortality analysis would be useful. Third, comorbidities could be further explored, using a Charlson score, for example. Despite these weaknesses, we encourage further, prospective, larger sample size investigations regarding the role of ORIF in Vancouver B2 fracture treatment. Considering that the radiographic results are comparable between the two groups, the null hypothesis is rejected, indicating that ORIF could be beneficial in patients older than 75 years, particularly from the operation duration and blood loss standpoint.
Data availability
Data available on request from the author.
References
Learmonth ID (2004) The management of periprosthetic fractures around the femoral stem. J Bone Jt Surg Br 86:13–19
Antoci V, Appleton P, Rodriguez EK (2014) Fixation of fractures around unstable hip implants. Tech Orthop 29:200–209. https://doi.org/10.1097/BTO.0000000000000102
Lindahl H (2007) Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury 38:651–654. https://doi.org/10.1016/j.injury.2007.02.048
Delgado A, Cordero G-GE, Marcos S, Cordero-Ampuero J (2020) Influence of cognitive impairment on mortality, complications and functional outcome after hip fracture: dementia as a risk factor for sepsis and urinary infection. Injury 51(Suppl1):S19–S24. https://doi.org/10.1016/j.injury.2020.02.009
Pike J, Davidson D, Garbuz D, Duncan CP, O’Brien PJ, Masri BA (2009) Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg 17:677–688. https://doi.org/10.5435/00124635-200911000-00002
Chatziagorou G, Lindahl H, Garellick G, Kärrholm J (2019) Incidence and demographics of 1751 surgically treated periprosthetic femoral fractures around a primary hip prosthesis. Hip Int 29:282–288. https://doi.org/10.1177/1120700018779558
Duncan CP, Masri BA (1995) Fractures of the femur after hip replacement. Instr Course Lect 44:293–304
Gaski GE, Scully SP (2011) In brief: classifications in brief: Vancouver classification of postoperative periprosthetic femur fractures. Clin Orthop Relat Res 469:1507–1510. https://doi.org/10.1007/s11999-010-1532-0
Naqvi GA, Baig SA, Awan N (2012) Interobserver and intraobserver reliability and validity of the Vancouver classification system of periprosthetic femoral fractures after hip arthroplasty. J Arthroplasty 27:1047–1050. https://doi.org/10.1016/j.arth.2011.11.021
Rayan F, Haddad F (2010) Periprosthetic femoral fractures in total hip arthroplasty—a review. Hip Int 20:418–426. https://doi.org/10.1177/112070001002000402
Schwarzkopf R, Oni JK (2013) Marwin SE (2013) Total hip arthroplasty periprosthetic femoral fractures: a review of classification and current treatment. Bull Hosp Jt Dis 71:68–78
Sledge JB 3rd, Abiri A (2002) An algorithm for the treatment of Vancouver type B2 periprosthetic proximal femoral fractures. J Arthroplasty 17:887–892. https://doi.org/10.1054/arth.2002.34810
Niikura T, Lee SY, Sakai Y, Nishida K, Kuroda R, Kurosaka M (2014) Treatment results of a periprosthetic femoral fracture case series: treatment method for Vancouver type b2 fractures can be customized. Clin Orthop Surg 6:138–145. https://doi.org/10.4055/cios.2014.6.2.138
Solomon LB, Hussenbocus SM, Carbone TA, Callary SA, Howie DW (2015) Is internal fixation alone advantageous in selected B2 periprosthetic fractures? ANZ J Surg 85:169–173. https://doi.org/10.1111/ans.12884
Stoffel K, Blauth M, Joeris A, Blumenthal A, Rometsch E (2020) Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: a systematic review. Arch Orthop Trauma Surg 140:1381–1394. https://doi.org/10.1007/s00402-020-03332-7
Epinette JA, Geesink RGT (1995) Radiographic assessment of cementless hip prostheses: ARA, a proposed new scoring system. Exp Sci Fr (English Volume)
Epinette JA (1999) Radiographic assessment of cementless hip prostheses: the “ARA” scoring system. Eur J Orthop Surg Traumatol 9:91–94. https://doi.org/10.1007/BF01695736
The SoFCOT Group, Delaunay C, Hamadouche M, Girard J, Duhamel A (2013) What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res 471:3863–3869. https://doi.org/10.1007/s11999-013-2935-5
Joestl J, Hofbauer M, Lang N, Tiefenboeck T, Hajdu S (2016) Locking compression plate versus revision-prosthesis for Vancouver type B2 periprosthetic femoral fractures after total hip arthroplasty. Injury 47:939–943. https://doi.org/10.1016/j.injury.2016.01.036
Manara J, Sandhu H, Wee M et al (2020) Prolonged operative time increases risk of blood loss and transfusion requirements in revision hip surgery. Eur J Orthop Surg Traumatol 30:1181–1186. https://doi.org/10.1007/s00590-020-02677-4
Ricci WM (2015) Periprosthetic femur fractures. J Orthop Trauma 29:130–137. https://doi.org/10.1097/BOT.0000000000000282
Acknowledgements
Special thanks to Ms. Agnes Stoka for substantial help in creation of this article. We also would like to thank Editage.com for English language editing.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare relevant to the content of this article.
Ethical approval
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethics Committee of Free University of Brussels approved this study.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martinov, S., D’ulisse, S., Haumont, E. et al. Comparative study of Vancouver type B2 periprosthetic fractures treated by internal fixation versus stem revision. Arch Orthop Trauma Surg 142, 3589–3597 (2022). https://doi.org/10.1007/s00402-021-03953-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03953-6