Abstract
Aim
The present prospective randomized study compared the bone transport technique (BT) and Masquelet technique (MT) in the treatment of infected gap non-union of the tibia.
Patients and methods
Total 25 patients with infected gap non-union of the tibia with bone gap upto 6 cm were randomised into BT group (group I, 13 patients) and MT (group II, 12 patients). The mean age was 31.77 years in group I and 39.67 years in group II. The mean intra-operative bone gap was 3.92 cm in group I and 3.79 cm in group II. Monolateral fixator was applied in nine patients each in both groups, while four and three fractures were stabilized with ring fixators in group I and II, respectively. Mean follow-up was 31.62 months and 30.42 months in group I and II, respectively. Bone and functional results were compared using the association for the study and application of the method of Ilizarov (ASAMI) criteria.
Results
The average fixator period was 9.42 and 16.33 months in group I and II, respectively (p < 0.001). Union was achieved in 12 (92%) patients and 6 (50%) patients in group I and II, respectively. The functional results were excellent (eight and two), good (four and six), fair (zero and three) and poor (one and one) in group I and II respectively, (p 0.23). The Bone results were excellent, good and poor in nine, three and one patients in group I, and three, three and six patients in group II respectively, (p 0.109).
Conclusions
The functional and bone results were comparable but more reliable in bone transport than the Masquelet technique. The fixator duration and incidence of non-union were higher in MT group. Ilizarov bone transport technique should be preferred in infected non-union of the tibia with bone loss upto 6 cm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incidence of infections in high-velocity compound-complex bone injuries is more prevalent in recent era due to high contaminations at road side accidents (RSA) and severe musculoskeletal insult ranging from 4 to 64% [1, 2]. Further infected gap bone defects are resilient to long course of antibiotics and surgical treatment makes this entity cumbersome to treat efficiently [2]. There are a number of modalities described in literature at different time with their varied successful outcomes including Ilizarov bone transport technique, Masquelet (induced membrane) technique, bone grafting in form of vascularized autograft or allografting, different mesh techniques and more recently bone morphogenic proteins and tissue engineering products [2,3,4,5,6,7,8,9]. Ilizarov bone transport is one of the most successful and worldwide accepted method of treatment for infected non-union of the tibia. It usually involves adequate debridement of necrotic and infected bone followed by corticotomy for distraction osteogenesis [4, 8,9,10,11,12,13]. On the other end two staged Masquelet technique involving radical debridement followed by antibiotic cement spacer in first stage and cancellous bone grafting within induced biomembrane after removal of spacer at 6–8 weeks in second stage gained much popularity with high successful rate [4, 5]. There is scarcity of documented English literature comparing both modalities in the management of infected bone gap defects of tibia. We conducted a prospective randomized study to compare Ilizarov bone transport and Masquelet techniques in management of infected gap non-union of the tibia with respect to union, functional outcome and related complications.
Materials and methods
The present prospective randomized comparative study included 25 patients of infected non-union of tibia presenting to author’s tertiary level institute between Jun 2016 and Dec 2018. Patients with posttraumatic infected nonunion of tibia having fractures of tibia with fracture line visible on radiographs and bone gap of < 6 cm with adequate soft tissue cover of the bone were included in the study. Subjects were considered to have an infection, if they either had active discharging sinus at the fracture site or positive swab culture from wound/sinus [4, 9]. Intraoperative tissue samples, as well as hislopathological examination, was used to confirm the infection as well as pathology. Any wound more than 1.5 cm in any dimension over fracture site was considered as inadequate soft tissue cover. Patients with periarticular nonunion, bone gap > 6 cm, age > 65 years and < 18 years, pathological fractures and fractures associated with bone disorders, presence of any debilitating systemic disease and any underlying hormonal disorders were excluded from the study. The majority of patients were young with high-velocity trauma, so having no comorbid conditions. Comorbid conditions can adversely affect outcomes in other group, so to maintain comparable groups these were excluded from both groups in present study.
A detailed history and careful physical examination were done to extract relevant data. With standard anterio-posterior and lateral radiographs of fractured bones, these were classified according to Paley al classification [1, 3]. Patients were subjected to all relevant pre-operative investigations for pre-anaesthesia fitness. Baseline pre-op erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and pus cultures were sent for all the subjects for future treatment and diagnostic guidance.
Surgical methods of debridement and primary stabilization
All the procedures were done under regional or general anaesthesia in a supine position with all aseptic precautions. A longitudinal or appropriate incision over the previous scar or fresh one as per need of local soft-tissue status was given over the non-union site. Previously used hardware in situ, if any persist, were removed and radical resection of all necrotic tissue including bones upto appearance of vital tissue or fresh bleeding at the bone ends was done. Intra-operative tissues were sent for pus culture and sensitivity as well as histopathological examination to confirm the infection as well pathology [14].
Randomization was done by chit/lottery method during the operative procedure, if the patient had post debridement bone gap ≤ 6 cm. Thirteen patients were treated with bone transport technique (group I) and 12 patients by Masquelet’s technique (group II).
Group (Gp) I (bone transport technique)
Fracture ends of the bone were stabilized with either ring fixator or monolateral (Limb Reconstruction System LRS, Pitkar, India) external fixators. Ring fixators were applied in the standard manner with four rings and four rods around the affected limb by measuring the rings in reference to the greatest circumference of the limb with additional two finger breadth increments for ring skin clearance both anteriorly and posteriorly. Total 10 wires measuring 1.8 mm diameter were passed through the safe zone for bone fixation. Wires were passed slowly, intermittently while limb muscles were kept in maximal functional length at the time of wire insertion. Corticotomy was done at a single level in all patients either at proximal, distal or mid-diaphyseal level after application of fixator depending upon the fracture level and bone gap. Wound margins were approximated loosely as possible as and relaxing incisions were given, if needed. Similarly, for monolateral fixators, device was mounted on the anteromedial subcutaneous surface of the tibia by placing pins parallel to the axis of the knee joint and perpendicular to long axis of the tibia with three clamps aligned by eight or nine tapered threaded pins. Throughout the procedure, utmost attention was given to keep the fracture aligned in both planes. All the patients were given intravenous antibiotics for 2 weeks which were switched off over oral antibiotics for further 2 weeks according to culture sensitivity.
Group II (Masquelet technique)
The two staged surgery performed in a standard manner as described in the literature [6, 7]. At first mechanical stage, after thorough radical debridement as mentioned earlier, created bone gaps were filled with the antibiotic impregnated bone cement (PMMA), which also maintained the bone length. The limbs were fixed with external fixators (ring or LRS) for 6–8 weeks in normal alignment. Intravenous antibiotics were given for two weeks followed by oral antibiotics for two weeks depending on intraoperative culture sensitivity report. Patients had no signs of infection at end of the first stage confirmed by the absence of pus discharge, normal ESR and CRP. At the second biological stage, integrated PMMA spacer over the defects were removed meticulously without disturbing the surrounding soft tissues and induced membrane over the cement. Defect was filled with cancellous bone autograft from iliac crests followed by wound closure in layers by approximating skin ends in a delicate manner. The fixation used in the first stage was continued in the second stage also. Patients had intravenous antibiotics for one week followed by oral antibiotics till suture removal after the second stage.
Post-operative care and rehabilitation
The pin tracts were sealed with Povidone-iodine soaked gauze pieces dressed at regular intervals. Patients were encouraged to ambulate from the very first post-operative day with partial weight-bearing while the active and passive range of movement exercises started simultaneously to prevent contracture and stiffness. Distraction at corticotomy site in Gp I was started on the seventh day at the rate of 1 mm/day (0.25 mm four times a day) and sutures were removed on the 12–14th post-operative day. Patients were followed sequentially at monthly intervals for a minimum of 6 months or until union appeared clinically and radiologically. At each follow-up assessment and management of complications, if any, was done. Pin tract infections were classified as superficial (grade 1 and 2) and deep infections (grade 3), according to Paley’s classification [1, 4]. Healing in form of union is considered radiologically if three of four cortices showed bridging callus while clinically if there was absence of pain and motion at the fracture site.
Frames were dynamized before removal. Frames were removed after achieving union at fracture sites and consolidation at corticotomy sites. After removal of the fixator frames, PVC (polyvinyl chloride) below knee brace was given for the next 6 months and progressive weight-bearing was allowed. Final assessment for bone results and functional results was done using Association for the study and application of the methods of Ilizarov (ASAMI) criteria (Table 1) [4, 8]. The relevant data was analyzed statistically by appropriate tests including the Chi-square test with Yates correction, Fisher exact test and independent student’s t tests using IBM SPSS Statistics Version 20 software while p value ≤ 0.05 was considered statistically significant.
Results
Demographic profile and operative data of both the groups are described in Table 2. There was no statistically significant difference between the two groups on the basis of age, sex, mode of injury, site of injury, side of injury, duration of nonunion, intraoperative bone gap, and follow-up period. Monolateral fixator was applied in nine patients each in both groups, while four and three fractures were stabilized with ring fixators in Gp I and II, respectively, (p 0.89). Mean intraoperative bone gap was 3.92 ± 0.86 cm (range 3–6 cm) and 3.79 ± 1.19 cm (range 2–6 cm) in Gp I and II, respectively (p 0.754). Corticotomy in group I was performed in nine and four patients at proximal and distal tibia respectively, whereas no corticotomy was done in group II. Mean gain in length with distraction osteogenesis was 3.85 ± 0.898 cm (range 3–6 cm) in group I whereas in group II, the gap was maintained with the exact length of bone cement in stage I followed by bone graft in stage II with a mean value of 3.79 ± 1.19 cm (p 0.898).
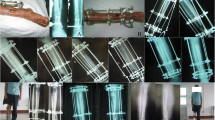
The average fixator period was 9.42 ± 2.37 months (range 6–12 months) and 16.33 ± 1.82 months (range 13–18 months), in group I and II respectively (p < 0.001, extremely significant). The average external fixator index (number of months the external fixator was attached to the bone per centimeter of length gained) was 2.486 ± 0.56 months/cm in Gp I and 4.71 + 1.71 months/cm in Gp II (p < 0.002, extremely significant). Fixator adjustment to correct axial deviation was required in two (15.4%) patients in Gp I and one (8.3%) patient in Gp II (p 0.94). Acute docking was done in one patient in Gp I only. In Gp I, the union was achieved primarily in 10 patients and after margin freshening and fixator adjustment in two more patients. So union was achieved in 12 (92%) patients and 6 (50%) patients in Gp I and II, respectively. Radiographic illustrations of treatment of infected non-union tibia with Ilizarov bone transport are described in Fig. 1. Non-union occurred in 50% (six) patients in Gp II as compared to one (8%) in Gp I, (p 0.056). Two patients among six failures in Gp II were managed with refreshening of non-union ends and refixation with bone transport technique while two limbs were managed with functional cast bracing with adequate functional outcomes. Two patients in Gp II were managed with below-knee amputation as insisted by patients.
a Preoperative radiograph (antero-posterior view) of right leg showing compound fracture of tibial mid-shaft and segmental fracture of the fibula. b Temporary stabilization of fractures of both bones with external fixator as damage control orthopedics resulting as infected non-union of the tibial diaphysis. c Immediate postoperative radiograph of right leg antero–posterior view, showing Ilizarov fixator stabilization after radical debridement of infected bone ends and proximal metaphyseal corticotomy of tibia. d Antero-posterior radiographic view of limb at final follow up showing consolidation of regenerate at proximal metaphyseal site and union at the fracture site with the adequate alignment of the limb. e Lateral radiographic view of limb at final follow up showing consolidation of regenerate at proximal metaphyseal site and union at fracture site with adequate alignment of limb
Radiographic illustrations of failed treatment of infected non-union tibia with Masquelet technique and revision surgery with Ilizarov bone transport is described in Fig. 2. No patient had a persistent infection at fracture site in any of the group. Cement spacer got exposed in four patients in Gp II at end of the first stage.
a Antero-posterior and lateral views of radiograph showing infected non-union of tibia managed with Masquelet technique and cement spacer in situ. b Radiographs showing failure of Masquelet technique and resorption of bone graft with sequestrum formation at grafting site. c Radiographs showing revision surgery with re-debridement and proximal metaphyseal corticotomy in failed Masquelet technique. d AP and lateral radiographs showing aligned limb with union at fracture site and regenerate formation at corticotomy site stabilized with Ilizarov bone transport technique. e AP and lateral radiographs showing complete union at the fracture site and consolidation of regenerate with the adequate alignment of the limb at corticotomy site at final follow-up
Limp was present in three patients (23.07%) in Gp I and nine patients (75%) in Gp II (p 0.028, statistically significant). Significant stiffness of knee, ankle, and both joints (loss of ≥ 15° knee extension and ankle dorsiflexion) were observed in zero, three, two and two, zero, two patients in Gp I and II respectively. Bone results were excellent in nine, good in three and poor in one patient in Gp I, whereas excellent, good and poor in three, three and six patients, respectively in Gp II. (p 0.109). Functional results were excellent (eight and two), good (four and six) and poor (one and one) in Gp I and II respectively, while three patients from Gp II had fair outcome (p 0.23).
Discussion
Management of infected non-union of the tibia to incorporating eradication of infection along with gaining pre-injury functional outcome is a cumbersome task. There are several modalities to overcome infection and associated problems in different forms, including traditional Ilizarov bone transport and newer one Masquelet technique [2,3,4,5,6,7,8,9,10,11,12,13]. The primary and utmost principle is to eradicate infection with meticulous debridement in all modalities followed by bong grafting or bone regeneration and aligned stable fixation of fracture ends [4]. Ilizarov bone transport methods can address both osseous and soft-tissue defects simultaneously using principles of distraction osteogenesis [4, 8, 9]. Masquelet technique has the additional advantage of use in small bones including hand and foot and periarticular defects [6, 7, 15,16,17,18].
Pseudo-synovial membrane around the cement spacer in MT while providing some vascular bed for graft incorporation with host bone, may act as a protective layer for bone graft against host immune system thus hampers graft resorption additional to the expression of various growth factors including bone morphogenic protein 2 (BMP-2), transforming growth factor-beta (TGF-B), Von Willebrand factor (VWF), interleukin6 (IL-6) and interlekin8 (IL-8) etc. [5, 7].
According to the literature there are comparable outcomes in view of treatment duration, complications, patient compliance, and satisfaction for both the methods of external fixation, Ilizarov as well as monolateral external fixators [4, 5, 9]. The mean duration of fixator was significantly higher in Gp II than I (16.33 vs 9.42), inspite of less mean bone gap (3.79 cm vs 3.92 cm), which was different in the study by Tong et al. [5] (10.15 months vs 17.21 months) for post-traumatic osteomyelitis bone defects in lower extremities. Average external fixation index of the present scenario was (2.48 months/cm in Gp I and 4.71 months/cm in Gp II) which was more than Yin et al. [19] (1.38 months/cm) and Chaddha et al. [8] (0.98 months/cm) and Ajmera et al. [20] (1.88 months/cm) while comparable to Hosny et al. [21] (2.30 months/cm) for Ilizarov BT group.
Our results, in terms of union (92%) in Gp I were comparable with various studies reported in the literature [19, 22, 23]. We are of the opinion that achievement of union is more reliable and predictable with bone transport technique than Masquelet technique in infected nonunion of the tibia with bone gap upto 6 cm.
Comparison of functional results and bone results by ASAMI criteria of the present study with document literature in past is tabulated in Table 3, 4, respectively. Functional and bony results were statistically non-significant between the groups while Gp I represented better results than Gp II [5, 8, 19,20,21], [24,25,26]. The excellent bone result was achieved in nine patients (69.2%) in Gp I as compared to only three (25%) in Gp II, (p 0.07). Similarly, excellent functional outcome was more common in Gp I (eight patients, 61.5%) than in Gp II (two patients, 16.6%), (p 0.06). This underlines the fact that more patients in Gp II had residual problems than Gp I. This further supports our opinion that achievement of good to excellent functional and bone results are more predictable with bone transport technique as compared to Masquelet technique in patients of infected nonunion of tibia with bone loss upto 6 cm. Bone transport technique also aids in the treatment of soft tissue defects as soft tissue also regenerates along with bone [4], [8,9,10,11,12,13], [19,20,21,22,23,24,25,26]. While the availability of adequate amount of autogenous cancellous Iliac bone grafts can be an issue for the reconstruction of major bone defect which can be addressed with use of femoral medullary grafts by RIA (Reamer irrigator aspirator) technique, allogenic bone or demineralized bone substitute [2, 3, 7]. There was an additional surgical insult at bone graft harvesting site, which further deranged mobility status of the patient at immediate post-operative period [5,6,7]. There were four cases of cement spacer exposure in Gp II, which might be related to soft tissue overlying non-viable bone cement or compromised soft tissue over the defects or overstuffing of the cement [7, 27,28,29]. These patients had no signs of reinfection at end of first stage confirmed by the absence of pus discharge, normal ESR and CRP values. Pin tract infection was the most common complication and were comparable in both groups. Similarly, joint stiffness was also comparable in both groups. Limping was observed more in Gp II and related to the stiffness of knee and ankle joints, shortening of limb, and more incidence of nonunions in Gp II. These all complications were also comparable to past literature [27,28,29,30,31,32,33]. The combined ortho-plastic approach has also some good results in the management of these complex injuries and has low complication rates documented in recent English literature [32]. There are some advantages of using bone transport technique over Masquelet technique [5] in terms of early allowance of weight-bearing, possibility of adjustments throughout the process, only single-stage treatment as compared to compulsory two stage treatment in Masquelet technique. When performing a bone transport the reconstructed bone is a hollow bone, similar to the original bone. The hollow bone is biomechanically better than the bone after using the Masquelet technique. In those cases, usually, a rodlike bone develops. The additional advantage of having no need of bone grafts and no added donor site morbidity gives bone transport an extra edge. However, there are some evidence on animal studies which support better bone healing with concentrated growth factors along with Masquelet technique on a critical bone defect model in rabbit radius but no consensus was observed in medical literature on infected bone defect of human limbs.
Results of the present study are relevant for comparison of bone transport and Masquelet technique in infected nonunion of tibia only upto 6 cm defects. However, Masquelet technique has shown its efficacy in treating large bone defects of all long bones including tibia, femur, humerus, and forearm [2, 5,6,7, 16]. Results of the Masquelet technique are independent of length of bone defect [7, 29]. Ten (77%) patients in Gp I had union with a single procedure only as compared to two staged Masquelet technique. The authors are of the opinion that bone transport technique should be preferred in patients with bone loss upto 6 cm. Bone loss of more than 6 cm may be managed with Masquelet technique, vascularized fibular grafting or Ilizarov bone transport technique.
This study had a small sample size and short follow-up as its limitations. We did not perform power analysis to calculate sample size as there is scarcity of literature comparing the two techniques and patients with stringent inclusion criteria of the present study are relatively rare. Longer follow-up with a larger sample size might better analyses the clinico-radiological outcomes of both methods. There was a scarcity of English medical literature which compared different techniques of treatment for infected non-union of tibia with described parameters so comparative evaluation was not extensive. However, the strength of study is its prospective and randomized nature. To the best of our knowledge, the present study is the first prospective randomized study in English literature comparing bone transport and Masquelet technique in infected nonunion of tibia.
Conclusions
Both Ilizarov bone transport and Masquelet technique achieved comparable radiological and functional outcomes in infected gap nonunion of the tibia with bone loss upto 6 cm but the results were more reliable and predictable in the bone transport group. We believe that Ilizarov bone transport technique should be preferred in infected nonunion of the tibia with bone loss upto 6 cm over the Masquelet technique.
Take home message
Ilizarov bone transport technique was found better than Masquelet technique in infected nonunion of the tibia with bone loss upto 6 cm. Bony and functional results were comparable in both the methods but more reliable in the Ilizarov bone transport group.
References
Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 250:81–104
Azi ML, Teixeira AAA, Cotias RB, Joeris A, Kfuri M (2019) Induced-membrane technique in the management of posttraumatic bone defects. JBJS Essent Surg Tech. https://doi.org/10.2106/JBJS.ST.18.00099
Giannoudis PV, Faour O, Goff T, Kanakaris N, Dimitriou R (2011) Masquelet technique for the treatment of bone defects: tips-tricks and future directions. Injury 42(6):591–598. https://doi.org/10.1016/j.injury.2011.03.036
Rohilla R, Wadhwani J, Devgan A, Singh R, Khanna M (2016) Prospective randomised comparison of ring versus rail fixator in infected gap nonunion of tibia treated with distraction osteogenesis. Bone Joint J 98(10):1399–1405
Kai T, Ziyi Z, Yulan P, Chuangxin L, Shenglu C, Yun Ping Y, Gang W (2017) Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury. https://doi.org/10.1016/j.injury.2017.03.042
Masquelet AC (2020) The induced membrane technique. Orthop Traumatol Surg Res 106(5):785–787. https://doi.org/10.1016/j.otsr.2020.06.001
Durand M, Barbier L, Mathieu L et al (2020) Towards understanding therapeutic failures in masquelet surgery: first evidence that defective induced membrane properties are associated with clinical failures. J Clin Med. https://doi.org/10.3390/jcm9020450
Chaddha M, Gulati D, Singh AP, Singh AP, Maini L (2010) Management of massive posttraumatic bone defects in the lower limb with the Ilizarov technique. Acta Orthop Belg 76:811–820
Rohilla R, Sharma PK, Wadhwani J, Rohilla S, Beniwal R (2019) Prospective randomized comparison of quality of regenerate in distraction osteogenesis of ring versus monolateral fixator in patients with infected non-union of tibia using digital radiographs and computed tomography. Bone Joint J 101(11):1416–1422
Sigmund IK et al (2020) Comparison of Ilizarov bifocal, acute shortening and relengthening, with bone transport in the treatment of infected, segmental defects of the tibia. J Clin Med 9:279. https://doi.org/10.3390/jcm9020279
Aktuglu K, Erol K, Vahabi A (2019) Ilizarov bone transport and treatment of critical-sized tibial bone defects: a narrative review. J Orthop Traumatol 20:22. https://doi.org/10.1186/s10195-019-0527-1
Tetsworth K et al (2017) Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury 48(10):2276–2284
Zhang Z et al (2018) Infection-free rates and sequelae predict factors in bone transportation for infected tibia: a systematic review and meta-analysis. BMC Musculoskelet Disord 19(1):442
Govaert GAM et al (2020) Diagnosing fracture-related Infections: current concepts and recommendations. J Orthop Trauma 34(1):8–17
Walker M, Sharareh B, Mitchell SA (2019) Masquelet reconstruction for posttraumatic segmental bone defects in the forearm. J Hand Surg Am 44:341–342. https://doi.org/10.1016/j.jhsa.2018.07.003
Masquelet AC, Begue T (2010) The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. https://doi.org/10.1016/j.ocl.2009.07.011
Bourgeois M, Loisel F, Bertrand D et al (2020) Management of forearm bone loss with induced membrane technique. Hand Surg Rehabil 39(3):171–177. https://doi.org/10.1016/j.hansur.2020.02.002
Chotel F, Nguiabanda L, Braillon P, Kohler R, Berard J, Abelin-Genevois K (2012) Induced membrane technique for reconstruction after bone tumor resection in children: a preliminary study. Orthop Traumatol Surg Res 98:301–308
Yin P, Zhang Q, Mao Z, Li T, Zhang L, Tang P (2014) The treatment of infected tibial nonunion by bone transport using the Ilizarov external fixator and a systematic review of infected tibial nonunion treated by Ilizarov methods. Acta Orthop Belg 80:426–435
Ajmera A, Verma A, Agrawal M, Jain S, Mukherjee A (2015) Outcome of limb reconstruction system in open tibial diaphyseal fractures. Indian J Orthop 49:429–435
Hosny G, Shawky MS (1998) The treatment of infected non-union of the tibia by compression-distraction techniques using the Ilizarov external fixator. Int Orthop 22(5):298–302
Maini L, Chaddha M, Vishwanath J, Kapoor S, Mehtani A, Dhaon BK (2000) The Ilizarov method in infected nonunions of fractures. Injury 31:509–517
Sen C, Eralp L, Gunes T, Erdem M, Ozden VE, Kocaoglu M (2006) An alternative method for the treatment of nonunion of the tibia with bone loss. J Bone Joint Surg Br 88:783–789
Patil S, Montgomery R (2006) Management of complex tibial and femoral nonunion using the Ilizarov technique, and its cost implications. J Bone Joint Surg [Br] 88(7):928–932
Harshwal RK, Sankhala SS, Jalan D (2014) Management of nonunion of lower extremity long bones using mono-lateral external fixator—report of 37 cases. Injury 45(3):560–567
Farmanullah KMS, Awais SM (2007) Evaluation of management of tibial non-union defect with Ilizarov fixator. J Ayub Med Coll Abbottabad 19(3):34–36
Masquelet AC, Kishi T, Benko PE (2019) Very long-term results of post-traumatic bone defect reconstruction by the induced membrane technique. Orthop Traumatol Surg Res 105(1):159–166
Siboni R, Joseph E, Blasco L, Barbe C, Bajolet O, Diallo S, Ohl X (2018) Management of septic non-union of the tibia by the induced membrane technique. What factors could improve results? Orthop Traumatol Surg Res 104(6):911–915
Morelli I, Drago L, George DA, Gallazzi E, Scarponi S, Romanò CL (2016) Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury 47(Suppl 6):S68–S76. https://doi.org/10.1016/S0020-1383(16)30842-7
Wang J, Yin Q, Gu S, Wu Y, Rui Y (2019) Induced membrane technique in the treatment of infectious bone defect: a clinical analysis. Orthop Traumatol Surg Res 10:1016
Testa G, Vescio A, Aloj DC, Costa D, Papotto G, Gurrieri L et al (2020) Treatment of infected tibial non-unions with Ilizarov technique: a case series. J Clin Med 9(5):1352. https://doi.org/10.3390/jcm9051352
Aljawadi A, Islam A, Jahangir N et al (2021) One-stage combined “fix and flap” approach for complex open Gustilo–Anderson IIIB lower limbs fractures: a prospective review of 102 cases. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03705-y
Iacobellis C, Berizzi A, Aldegheri R (2010) Bone transport using the Ilizarov method: a review of complications in 100 consecutive cases. Strat Trauma Limb Reconstr 5(1):17–22. https://doi.org/10.1007/s11751-010-0085-9
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Contributions
RR chief operating surgeon for most of the surgeries, wrote the manuscript, statistical analysis, conducted the data analysis. PKS assisted most of the surgeries, conducted the data analysis, wrote the manuscript, statistical analysis. JD assisted most of the surgeries, conducted the patient follow-up and record-keeping, edited the manuscript. JW data collection, data analysis, wrote the manuscript. RS conducted the data analysis, edited the manuscript. DB conducted the data analysis, edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Informed consent
Informed and written consent was taken from all the patients for surgical interventions as well as for the study participations. This study was approved by the Institutional Review Board (IRB ID: IEC/Th/18/Ortho/03).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rohilla, R., Sharma, P.K., Wadhwani, J. et al. Prospective randomized comparison of bone transport versus Masquelet technique in infected gap nonunion of tibia. Arch Orthop Trauma Surg 142, 1923–1932 (2022). https://doi.org/10.1007/s00402-021-03935-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03935-8