Abstract
Introduction
In total hip arthroplasty (THA), improper cup orientation can result in dislocation, early excessive polyethylene wear, and pain following THA. The supine position during THA provides a more reproducible functional pelvic position than the lateral decubitus position and may allow freehand cup placement as reliable as that obtained by computer navigation. The purpose of this study was to investigate the accuracy of freehand cup placement through a supine direct anterior approach (DAA) compared with computed tomography (CT)-based navigation.
Materials and methods
The same surgeon performed primary cementless THA through the DAA in 144 supine patients. Seventy-two patients underwent freehand cup placement with standard mechanical guidance-oriented radiographic target cup positioning, and 72 underwent placement with CT-based navigation guidance. Using three-dimensional templating software, the study group calculated cup inclination and anteversion on postoperative CT scans.
Results
The navigation method resulted in a significantly smaller deviation of inclination from the target (p < 0.05); the difference in anteversion was not significant. In addition, the navigation method resulted in significantly fewer cups placed ± 10° outside the target position (0% for inclination, 0% for anteversion) than did the freehand procedure (26% for inclination, 25% for anteversion) (p < 0.0001).
Conclusions
Freehand cup placement is less reliable even in the supine position. Use of a CT-based navigation system can significantly improve cup positioning in THA through the DAA by reducing the incidence of outliers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In total hip arthroplasty (THA), improper cup orientation can result in an increased risk of dislocation, early excessive polyethylene wear, and pain following THA [1,2,3]. Some authors have reported that supine patient positioning for THA allows more reliable freehand cup placement than does the lateral decubitus position [4,5,6]. With the popularisation of the direct anterior approach (DAA), THA is being increasingly performed with the patient in the supine position [4,5,6,7,8]. The supine procedure may logically allow a more reproducible, functional pelvic position at the time of cup placement. Conversely, other authors have reported that computer navigation systems for THA through a posterior, anterolateral, or lateral approach help control and minimise errors in cup positioning [9,10,11]. The study group hypothesised that the DAA in the supine position would allow reliable freehand cup placement and could be comparable to computer navigation. The purpose of this study was to investigate the accuracy of freehand versus computer-navigated insertion of the acetabular cup.
Patients and methods
Using the study group’s total joint registry, all consecutive primary THAs performed by the same surgeon from May 2016 to December 2019 were identified. A computed tomography (CT)-based navigation system (Stryker Nav3i; Stryker Leibinger, Freiburg, Germany) was introduced in January 2018. All primary THAs were performed without the navigation system from May 2016 to December 2017, and these patients constituted the freehand group. All THAs were performed using the navigation system from January 2018 to December 2019, and these patients constituted the navigation group. The surgeon routinely utilised the DAA for primary THA during the study period except in three patients: two with hip hardware that was removed at the time of THA and one whose prior posterior skin incision was used after previous Chiari pelvic osteotomy. A posterior approach was used for these three THAs. In total, 154 patients were identified during the study period. Of these 154 patients, the three above-mentioned patients were excluded; another seven patients (three from the freehand group, four from the navigation group) were also excluded because of missing or inadequate postoperative CT data. The remaining 144 patients were available for this retrospective case–control study. The freehand group comprised 72 patients, and the navigation group comprised 72 patients. The medical ethics committee of the study group’s institution approved the study protocol. All patients gave informed consent to undergo the postoperative CT scan, which was a standard postoperative follow-up procedure.
The mean age (± standard deviation) of the 144 patients (30 men, 114 women) was 69.2 ± 10.3 years (39–90). The mean body mass index (± standard deviation) was 24.5 ± 4.4 kg/m2 (15.4–42.8).
All surgeries were performed by the same surgeon, who had performed over 100 DAA cases before initiating the present study. All operations were performed through the DAA with the patient supine without a traction table. The patients in this study underwent THA using a cementless acetabular cup [Trident cup (Stryker, Mahwah, NJ, USA) (n = 76), G7 cup (Zimmer, Warsaw, IN, USA) (n = 39), or SQRUM cup (Kyocera, Kyoto, Japan) (n = 29)] and a cementless femoral stem [Profemur TL stem (MicroPort Orthopedics, Arlington, TN, USA) (n = 87), Hydra stem (Adler Ortho, Cormano, Italy) (n = 16), Initia stem (Kyocera) (n = 14), J-Taper stem (Kyocera) (n = 12), Mainstay stem (Kyocera) (n = 6), TaperLoc stem (Zimmer) (n = 6), Accolade II stem (Stryker) (n = 1), Acuta stem (Adler Ortho) (n = 1), or Profemur Z stem (Microport Orthopedics) (n = 1)] were used. An anterior skin incision, typically 8–10 cm long, was used in both groups.
In both groups, a pelvic CT scan was performed preoperatively. Preoperative planning was then performed with three-dimensional (3D) templating software (Zed Hip; Lexi, Tokyo, Japan) [12]. Three reference points (the bilateral anterior superior iliac spines and the pubic symphysis) were used to determine the orientation of the anterior pelvic plane. For planning, the pelvic reference system was based on the functional pelvic plane, where the pelvis in the supine position on the CT table was axially rotated until the bilateral anterior iliac spines touched the same horizontal plane [5, 13]. Next, a virtual 3D model of the cup was placed into the virtual 3D model of the natural acetabulum to determine the position and size of the cup on coronal, sagittal, and axial views. The study group attempted to place the cups to ensure a > 10° cup centre-edge angle by a combination of medial and superior shifts of the cup from the original acetabular position without perforation of the medial wall [14]. The study group’s general philosophy has been to prioritise bony coverage over anatomic placement. The cup size was determined to fit the anterior and posterior acetabular walls. The target cup position with respect to the functional pelvic plane differed depending on the group, as described below. In addition, the femoral stem size and position were selected to maximise the fit and fill of the femoral metaphysis. Stem anteversion was measured as the angle between the axis of the stem neck and the posterior condylar axis [15].
In the freehand group, the cup was placed using standard mechanical alignment guides with jigs intraoperatively. Although conventional mechanical guides with jigs are usually oriented to the operative cup inclination and anteversion [16], the standard mechanical guides in this study were specially designed to orient the cup in 40° of radiographic inclination and 20° of radiographic anteversion with the patient supine [16]. Therefore, the target cup position in the freehand group was 40° of radiographic inclination and 20° of radiographic anteversion with respect to the functional pelvic plane. If the pelvis is stable intraoperatively, these specially designed guides can achieve the target cup position.
In the navigation group, THA was performed with the CT-based navigation system. Before skin incision, a pelvic tracker was percutaneously fixed to the ipsilateral iliac crest with an external fixation device. The virtual 3D model of the pelvis was matched with the intraoperative position of the patient’s pelvis using surface registration. The reamer and the cup inserter were instrumented with a tracker. Reaming and cup impaction were performed under the constant guidance of the CT-based navigation system. The target radiographic inclination and anteversion with respect to the functional pelvic plane was determined in each patient from predetermined femoral stem anteversion, according to the combined anteversion theory [17].
All 144 patients underwent a pelvic CT scan 1 week after the operation. In both groups, a postoperative virtual 3D model of the pelvis was reconstructed with the same 3D templating software. All three reference points on the preoperative plan were manually copied onto the postoperative CT to standardise the preoperative and postoperative pelvic position. The virtual 3D model of the implanted cup on templates was superimposed on the virtual 3D model of the cup created with postoperative CT data to calculate the final postoperative radiographic inclination and anteversion of the implanted cup (Figs. 1, 2). The study group calculated the difference between the target cup position and the final postoperative value and defined deviations from the target cup position. The study group defined a cup position of ± 10° outside the target as an outlier. All measurements on preoperative or postoperative CT images in this investigation were completed by a single observer. The operative time (from incision to closure) was compared. The rate of dislocation within the first 6 months postoperatively was recorded.
Computer screen view in three-dimensional (3D) templating software demonstrates three postoperative views (coronal, sagittal, and axial). The virtual 3D model of the implanted cup on templates was superimposed on the virtual 3D model of the acetabular cup to calculate the final postoperative cup inclination and anteversion
Statistical analysis
An independent t test was used for normally distributed continuous data, and the Mann–Whitney U test was used for nonparametric data. Fisher’s exact test was used to compare categorical data. Odds ratios and 95% confidence intervals (CIs) were reported for cups placed ± 10° outside the target. An odds ratio of 0.55–1.82 was defined as equivalent between the groups [18].
Statistical analysis was performed with Prism 6 (GraphPad Software Inc., San Diego, CA, USA). Values of p < 0.05 were considered statistically significant.
Results
There were no significant differences in demographic data between the two groups (Table 1). The mean operative time was higher in the freehand group (119 ± 26 min) than in the navigation group (108 ± 15 min; p < 0.01).
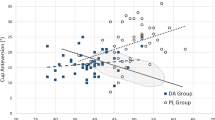
In the freehand group, the mean postoperative inclination was 35.1° ± 7.3° (18°–53°) and the mean postoperative anteversion was 23.0° ± 8.1° (− 1° to 41°). In the navigation group, the mean postoperative inclination was 37.7° ± 3.1° (32°–46°) and the mean postoperative anteversion was 17.1° ± 4.3° (6°–27°).
In the freehand group, the mean deviation of inclination from the target was − 4.4° ± 7.8° (− 21° to 15°), and the mean deviation of anteversion from the target was 4.0° ± 8.3° (− 18° to 26°). In the navigation group, the mean deviation of inclination from the target was − 2.1° ± 3.1° (− 8° to 6°), and the mean deviation of anteversion from the target was 2.6° ± 2.8° (− 3° to 9°).
The navigation method resulted in a significantly smaller mean deviation of inclination from the target than did freehand placement (p < 0.05). There was no significant difference between the two groups in anteversion (p = 0.173).
The computer-navigated method resulted in significantly fewer outliers in both inclination and anteversion than did the freehand method (p < 0.0001) (Table 2). The odds ratios for cups placed ± 10° outside the target were 0.02 (95% CI 0.00–0.32) for inclination and 0.02 (95% CI 0.00–0.34) for anteversion, failing to show equivalence between the groups. Using a post hoc power analysis, the study group found sufficient power (power = 0.996) to detect a difference in the percentage of outliers between the groups.
A single posterior dislocation occurred in the freehand group; none occurred in the navigation group. This difference was not significant (p = 1.000). The dislocation in the freehand group was treated with closed reduction and had no further sequelae.
Discussion
The 3D-CT reconstruction method for measuring cup position is superior to conventional radiographic analysis and remains the gold standard [19,20,21,22]. Tannast et al. [13] showed that measurements of cup anteversion on postoperative anteroposterior radiographs without accurate definition of the pelvic position are highly inaccurate because of pelvic tilt, rotation, and obliquity. Cup position can be accurately calculated with 3D templating software by using the anterior pelvic plane as a pelvic reference system. The importance of this study is that the study group compared the freehand technique with CT-based navigation by assessing postoperative cup position on 3D-CT reconstructions.
The DAA for THA has become increasingly popular in recent years, primarily because of claims of reduced surgical trauma, shorter recovery time, and a low rate of dislocation [4, 7, 8, 23]. A systematic review and meta-analysis showed that the DAA had a significantly lower dislocation rate relative to the posterior approach [23]. The lower risk of dislocation with the DAA could result from more desirable cup positioning [24]. A reason for the more desirable cup positioning with the DAA may be the stability of the pelvis in the supine position. The supine DAA appears to provide reliable freehand cup placement because supine patient positioning for THA maintains a stable pelvic position intraoperatively [4,5,6]. Three studies of DAA-THA with the freehand technique have reported the percentage of outliers (± 10° outside the target position) (Table 3) [5, 24, 25]. The percentage of outliers in this study was higher than that in some reports [5, 24] and lower than that in one report [25]. However, two of these studies measured cup position on conventional radiographs [24, 25], making these measurements not truly comparable. This study and that of Eilander et al. [5] measured cup position with 3D-CT, suggesting that the accurate percentage of outliers with freehand cup placement may be 16–26% for inclination and 5–25% for anteversion. These reports suggest that the freehand technique may be associated with both better and poorer cup placement and that the freehand technique cannot necessarily achieve the target cup position even with the patient supine.
Cup placement with the freehand technique in this study was not equivalent but instead inferior to that with navigation, although the study group used guides specially designed to orient the acetabular cup in 40° of radiographic inclination and 20° of radiographic anteversion with the patient supine. This raises the question: Is the pelvis stable during THA with the patient supine? Few reports have evaluated intraoperative changes in pelvic position during use of the supine DAA. Shah et al. [26] measured intraoperative changes in pelvic position in the transverse and sagittal planes during the DAA by using a smartphone mounted on the navigation tracker fixed on the iliac crest. They reported a change in pelvic position of ≥ 5° in both the sagittal and transverse planes in four of 22 patients (18.2%). They concluded that the pelvis is not fixed on the operating table during the supine DAA. In another study, Maeda et al. [27] placed a trial cup in the acetabulum using a mechanical guide to measure the true alignment of the trial cup with a CT-based navigation system during the supine DAA. They calculated the difference in cup position between the surgeon’s estimation and the true measurement and found that the pelvis rotated posteriorly by 9.3°, tilted caudally by 1.0°, and extended by 8.4° at the time of cup implantation. They concluded that the pelvis could not be stabilised with the DAA in the supine position and that extension and posterior rotation of the pelvis increased during cup procedures. Several authors have reported that the pelvic position is stable and highly reproducible when the patient is supine, provided that the hip joint is not dislocated [5, 13]. When the hip is dislocated intraoperatively, placement of acetabular retractors, acetabular reaming, and cup impaction can easily increase extension and posterior rotation of the pelvis [26, 27]. During CT-based navigation, the intraoperative motion of the pelvis can be tracked with a pelvic tracker. In fact, the accuracy of cup placement with the CT-based navigation technique in this study was higher and more reliable (Table 3).
To the study group’s best knowledge, no studies have focussed on actual clinical comparisons between the freehand technique and CT-based navigation technique through the DAA in the supine position. In a cadaver study, Nogler et al. [28] compared cup positioning through the DAA with an imageless navigation system versus conventional placement and found a significantly smaller range of deviation from the target with navigation. However, the study group cannot directly compare the present results with other clinical studies comparing the freehand technique and CT-based navigation through the DAA. In surgical approaches other than the DAA, some authors have compared freehand cup placement with computer-navigated cup placement in supine THA. Kalteis et al. [10] reported that CT-based navigation using the supine lateral approach resulted in significantly fewer cup placements ± 10° outside the target position (17%) than did the freehand procedure (53%). Parratte et al. [11] reported that the use of an imageless navigation system with the supine anterolateral approach resulted in significantly fewer cups placed ± 10° outside the target position (20%) than did the freehand technique (57%). These findings suggest that even in the supine position, the use of computer navigation significantly reduces outliers compared with the freehand technique, although these different surgical approaches prevent direct comparison with this study. Cup anteversion may vary among surgical approaches even in the same supine position [29, 30]. Chen et al. [29] reported significantly greater cup anteversion when using the supine DAA than when using a supine direct lateral approach. Kawarai et al. [30] also reported significantly greater cup anteversion with the supine DAA than with a supine anterolateral approach. These findings suggest that a different approach with the same supine position can result in different cup positions. Therefore, a clinical comparison of the freehand technique and CT-based navigation in the supine DAA is necessary. This study showed that CT-based navigation with the DAA resulted in significantly fewer cups placed ± 10° outside the target position (Table 3). In the present study, CT-based navigation resulted in significantly fewer outliers in cup positioning than the freehand technique during the DAA but did not significantly reduce the rate of dislocation within the first 6 months. The importance of a safe zone with respect to the incidence of dislocation remains controversial. Some studies have shown that cup positioning inside versus outside of a safe zone had no effect on the dislocation rate [31,32,33]; whereas, others have demonstrated that patients who sustained dislocation were less likely than other patients to have the cup positioned within a safe zone [2, 34]. Because dislocations are multifactorial, the cup position alone might not necessarily reduce the incidence of dislocation. The surgical approach also influences the risk of dislocation [23, 32, 33]. Although the DAA has the advantage of maintaining dynamic stability by sparing the posterior hip capsule and short external rotators [24], the optimal target for the DAA is unknown and an area of future investigation. The study group believe that most surgeons agree that the cup position is important and thus try to place the cup at the optimal target. This study has shown the extent of deviation from the target and could help to choose either the freehand technique or navigation to achieve the optimal target for the DAA in future.
Unexpectedly, the operative time was significantly shorter in the navigation group. This can be explained by the steep learning curve for the DAA or the surgeon’s high-volume experience with navigation (the surgeon had performed more than 400 posterior-approach THAs using the same CT-based navigation system at previous institutions). Garbarino et al. [35] performed the first 200 consecutive primary THA through the DAA and reported that the first 100 and second 100 cases had significant differences in operative times (118.1 vs 110.4 min, p = 0.009). A significant learning curve over the first 100 cases was consistent with the result of the present study.
There is a limitation to this study. This was not a randomised controlled study. However, there were no differences between the groups in age, sex, or BMI. Therefore, the study group believe this study offers valuable information about the comparison between the freehand technique and navigation.
Conclusion
The results of this study indicate that freehand cup placement is less reliable than navigation, even in the supine position. The pelvis does not seem to remain spatially stable intraoperatively. CT-based navigation can track the intraoperative motion of the pelvis with a pelvic tracker. Use of a CT-based navigation system improves cup positioning during THA through the DAA, as shown by a lower incidence of outliers in cup inclination and anteversion.
References
Patil S, Bergula A, Chen PC, Colwell CW Jr, D’Lima DD (2003) Polyethylene wear and acetabular component orientation. J Bone Jt Surg Am 85(Suppl 4):56–63
Sadhu A, Nam D, Coobs BR, Barrack TN, Nunley RM, Barrack RL (2017) Acetabular component position and the risk of dislocation following primary and revision total hip arthroplasty: a matched cohort analysis. J Arthroplasty 32(3):987–991
Chalmers BP, Sculco PK, Sierra RJ, Trousdale RT, Berry DJ (2017) Iliopsoas impingement after primary total hip arthroplasty: operative and nonoperative treatment outcomes. J Bone Jt Surg Am 99(7):557–564
Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H (2009) A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplasty 24(5):698–704
Eilander W, Harris SJ, Henkus HE, Cobb JP, Hogervorst T (2013) Functional acetabular component position with supine total hip replacement. Bone Jt J 95(10):1326–1331
Grammatopoulos G, Gofton W, Cochran M, Dobransky J, Carli A, Abdelbary H, Gill HS, Beaulé PE (2018) Pelvic positioning in the supine position leads to more consistent orientation of the acetabular component after total hip arthroplasty. Bone Jt J 100(10):1280–1288
Matta JM, Shahrdar C, Ferguson T (2005) Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res 441:115–124
Goebel S, Steinert AF, Schillinger J, Eulert J, Broscheit J, Rudert M, Nöth U (2012) Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop 36(3):491–498
Digioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS et al (2002) Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty 17(3):359–364
Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J (2006) Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Jt Surg Br 88(2):163–167
Parratte S, Argenson JN (2007) Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Jt Surg Am 89(3):494–499
Kase M, O’Loughlin PF, Aït-Si-Selmi T, Pagenstert G, Langlois J, Bothorel H, Bonnin MP (2020) Pre-operative templating in THA. Part I: a classification of architectural hip deformities. Arch Orthop Trauma Surg 140:129–137
Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F (2005) Anatomic referencing of cup orientation in total hip arthroplasty. Clin Orthop Relat Res 436(7):144–150
Sugano N, Nishii T, Nakata K, Masuhara K, Takaoka K (1995) Polyethylene sockets and alumina ceramic heads in cemented total hip arthroplasty. A ten-year study. J Bone Jt Surg Br 77(4):548–556
Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT (1987) Femoral anteversion. J Bone Jt Surg Am 69(8):1169–1176
Murray DW (1993) The definition and measurement of acetabular orientation. J Bone Jt Surg Br 75(2):228–232
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22(4):815–821
Silva GT, Logan BR, Klein JP (2009) Methods for equivalence and non-inferiority testing. Biol Blood Marrow Transplant 15(1 Suppl):120–127
Craiovan B, Renkawitz T, Weber M, Grifka J, Nolte L, Zheng G (2014) Is the acetabular cup orientation after total hip arthroplasty on a two dimension or three dimension model accurate? Int Orthop 38(10):2009–2015
Bayraktar V, Weber M, Kunow FV, Zeman F, Craiovan B, Renkawitz T, Grifka J, Woerner M (2017) Accuracy of measuring acetabular cup position after total hip arthroplasty: comparison between a radiographic planning software and three-dimensional computed tomography. Int Orthop 41(4):731–738
Holzer LA, Scholler G, Wagner S, Friesenbichler J, Maurer-Ertl W, Leithner A (2019) The accuracy of digital templating in uncemented total hip arthroplasty. Arch Orthop Trauma Surg 139:263–268
Savov P, Budde S, Tsamassiotis S, Windhagen H, Klintschar M, Ettinger M (2020) Three-dimensional templating in hip arthroplasty: the basis for template-directed instrumentation? Arch Orthop Trauma Surg 140:827–833
Higgins BT, Barlow DR, Heagerty NE, Lin TJ (2015) Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty 30(3):419–434
Soderquist MC, Scully R, Unger AS (2017) Acetabular placement accuracy with the direct anterior approach freehand technique. J Arthroplasty 32(9):2748–2754
Brun OCL, Sund HN, Nordsletten L, Röhrl SM, Mjaaland KE (2019) Component placement in direct lateral vs minimally invasive anterior approach in total hip arthroplasty: radiographic outcomes from a prospective randomized controlled trial. J Arthroplasty 34(8):1718–1722
Shah SM, Walter WL, Ngo J (2017) Is the pelvis stable during supine total hip arthroplasty? Acta Orthop Belg 83(1):81–86
Maeda Y, Sugano N, Nakamura N, Hamawaki M (2015) The accuracy of a mechanical cup alignment guide in total hip arthroplasty (THA) through direct anterior and posterior approaches measured with CT-based navigation. J Arthroplasty 30(9):1561–1564
Nogler M, Mayr E, Krismer M, Thaler M (2008) Reduced variability in cup positioning: the direct anterior surgical approach using navigation. Acta Orthop 79(6):789–793
Chen AF, Chen CL, Low S, Lin WM, Chinnakkannu K, Orozco FR, Ong AC, Post ZD (2016) Higher acetabular anteversion in direct anterior total hip arthroplasty: a retrospective case-control study. HSS J 12(3):240–244
Kawarai Y, Iida S, Nakamura J, Shinada Y, Suzuki C, Ohtori S (2017) Does the surgical approach influence the implant alignment in total hip arthroplasty? Comparative study between the direct anterior and the anterolateral approaches in the supine position. Int Orthop 41(12):2487–2493
Esposito CI, Gladnick BP, Lee YY, Lyman S, Wright TM, Mayman DJ, Padgett DE (2015) Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty 30(1):109–113
Grammatopoulos G, Thomas GER, Pandit H, Beard DJ, Gill HS, Murray DW (2015) The effect of orientation of the acetabular component on outcome following total hip arthroplasty with small diameter hard-on-soft bearings. Bone Jt J 97(2):164–172
Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW (2016) What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res 474(2):386–391
Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B (2005) Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Jt Surg Br 87(6):762–769
Garbarino L, Gold P, Sodhi N, Iturriaga C, Mont MA, Boraiah S (2021) Does structured postgraduate training affect the learning curve in direct anterior total hip arthroplasty? A single surgeon’s first 200 cases. Arthroplast Today 12(7):98–104
Funding
The authors did not receive support from any organisation for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
The medical ethics committee of our institution approved the study protocol.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nishihara, S., Hayashida, K. Comparison between freehand technique and computed tomography-based navigation in acetabular cup placement through direct anterior approach for total hip arthroplasty. Arch Orthop Trauma Surg 142, 323–329 (2022). https://doi.org/10.1007/s00402-021-03920-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03920-1