Abstract
Introduction
Displaced femoral neck fractures (FNF) are complicated by high mortality rates and continue to represent an important cause of disability, having a negative impact on patient mobility and physical independence. The purpose of this study was to update and analyse current outcomes and evidence concerning hip hemiarthroplasty (HHA) versus total hip arthroplasty (THA) for displaced femoral neck fractures in the elderly. Thus, a meta-analysis of randomized clinical trials was conducted.
Materials and methods
This meta-analysis was conducted according to the PRISMA guidelines. In October 2019, the following databases were accessed: Embase, Google Scholar, Pubmed, Scopus. All randomized clinical trials (RCTs) comparing total hip arthroplasty versus hip hemiarthroplasty for displaced femoral neck fractures were included in the present study. For the statistical analysis and the methodological quality assessment, the Review Manager Software 5.3 (The Nordic Cochrane Collaboration, Copenhagen) and STATA/MP Software 14.1 (StataCorp, College Station, TX) were used.
Results
Data from 2325 (1171 HHA vs 1154 THA) patients were collected. The mean follow-up was 58.12 months. The HHA group reported lower values of the mean Harris hip score (EE 3.22; p = 0.2), surgical duration (EE 21.75; p < 0.0001), length of the hospitalization stay (EE 0.8; p = 0.4). The HHA group evidenced lower dislocations rate (OR 1.78; p = 0.01, Fig. 4), but higher rate of acetabular erosion (OR 0.08; p = 0.0006). At a mean of 58.12 ± 52.8 months follow-up, revisions rate scored reduced in the THA group (OR 0.76; p = 0.2). Subgroup analysis of RCTs < 5 years follow-up revealed reduced revision in favour of the HHA group (OR 2.19; p = 0.03), while subgroup analysis of RCTs > 5 years follow-up revealed reduced revision in favour of the THA group (OR 0.25; p = 0.0003). The Kaplan–Meier curve detected similarity of patients survivorship between the two groups (HR 1.06; p = 0.3).
Conclusion
For the elderly population, both HHA and THA are valid solutions to treat displaced femoral neck fractures, with comparable survivorship. HHA detected reduced dislocations, while for THA a lower risk of acetabular erosion and further revision surgeries were reported.
Level of evidence
Level I, meta-analysis of randomized clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of femoral neck fractures (FNF) is approximately 80 in 100,000 [1]. About 67% FNF are displaced, requiring open reduction [2]. The most important risk factors are posed by bone density, neck anatomy, injury mechanism, female gender, alcohol, and corticosteroid abuse [3]. Interestingly, an epidemiologic study estimated that the number of FNF will increase to over six million over the next 50 years [4]. FNF report a high mortality rate [5] and represents a pivotal cause of disability, having a negative impact on patient mobility and physical independence. Furthermore, FNF present a considerable healthcare expenditure [6]. Concerning the treatment, there exists no definite consensus and several different techniques have been described [7]. Total hip arthroplasty (THA) and hip hemiarthroplasty (HHA) represent the treatments of choice for displaced FNF [8]. The discussion regarding hemiarthroplasty versus total arthroplasty began approximately 50 years ago, and is still subject of contentious debates [9]. Two international surveys conducted by Bhandari et al. [8] and the American Association of Hip and Knee Surgeons [10] confirm that 80–85% of surgeons preferred HHA. From the patient’s point of view, a general preference for THA has been reported [11]. Since there still exists an ongoing discussion regarding the pros and cons of either treatment [12,13,14,15], it is essential to review current evidence to help in the decision-making process. Previous meta-analyses were published in 2012 [9, 16, 17] and in 2015 [18]. Recently, RCTs have been published that have not yet been included in any meta-analysis [19,20,21,22]. An update of the literature is necessary. Therefore, a meta-analysis comparing THA versus HHA for displaced femoral fractures in the elderly was conducted, to update and analyse current outcomes and evidence.
Materials and methods
The present study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [23]. A preliminary guideline protocol was compiled:
-
P (patient): displaced femoral neck fracture;
-
I (intervention): hip hemiarthroplasty (HHA);
-
C (comparison): total hip arthroplasty (THA);
-
O (outcomes): surgical duration, length of stay, clinical scores, complications.
Literature search and study selection
Two authors (FM, JE) independently performed the literature search. In October 2019, the same authors accessed the following databases: Pubmed, Embase, Google Scholar, Scopus. The following keywords were used in combination: displaced femur neck fracture, total hip arthroplasty, hip hemiarthroplasty, hip replacement, Harris hip score, revision, dislocation. The same authors independently screened the titles resulting from the database search for inclusion and accessed the full-text version of the articles of interest. The bibliographies of the full-text articles were checked as well.
Eligibility criteria
All RCTs comparing THA versus HHA for femoral neck fractures were included in the present study. According to the Oxford Centre of Evidence-Based Medicine [24], only articles classified as level of evidence I were included. Articles in English, Italian, Spanish, German, French, were taken into account. Every type of implant or surgical approach was considered for inclusion. Only studies treating patients with HHA or THA for displaced femoral neck fractures were considered, as were studies reporting quantitative data under the outcomes of interest. Only studies treating patients > 70 years old were considered. Articles published before 2000 were excluded, as were those treating animals, biomechanics, cadaveric, or in vitro studies. Studies treating revision surgeries were excluded. Studies evaluating these procedures through the addition of adjuvants, such as stem cells, PRP, or any other infiltrations, were excluded. Disagreements between the authors were debated and mutually solved.
Outcomes of interest
Two independent authors (FM, JE) exported data of interest from each clinical trial. The demographic data exported were the following: author, year of the publication, number of enrolled hips, and duration of the follow-up (months). Successively, the included articles were divided into two study groups: THA, HHA. The following data were extracted: number of enrolled hips, percentage of female patients, mean age of the samples, Harris hip score [25], surgical duration, duration of hospitalization. Further dislocation, acetabular erosion and revision surgeries were collected for each group, along with patient mortality.
Methodological quality assessment
For the methodological quality assessment, the Review Manager Software Version 5.3 (The Nordic Cochrane Centre, Copenhagen) was used. Two authors (FM, JE) independently performed the assessment. The aforementioned tool analyses the included articles with regard to five aspects: selection bias (random sequence generation and allocation concealment), performance bias, detection bias, attrition bias, and reporting bias.
Statistical analysis
The statistical analysis was performed by the senior author (FM). To assess the baseline comparability, the Student T test was performed. For the statistical analysis of quantitative variables, the Review Manager Software version 5.3 (The Nordic Cochrane Centre, Copenhagen) was used. Dichotomous data were analysed using the Mantel–Haenszel method with the odds ratio (OR) effect measure. Continuous data were analysed using the Inverse Variance method with the mean difference (MD). A fixed model method was used for the setup. To assess data heterogeneity, both chi-square (\(\chi\)2) and Higgins (I2) statistical tests were performed. Values of \(\chi\)2 > 0.5 indicate high heterogeneity. Values of I2 of 0–40%, 40–75%, 75–100% indicate low, moderate, and high data heterogeneity, respectively. In case of high heterogeneity, a random model effect was adopted. To analyse the publication bias, a funnel plot of the most commonly reported outcome was generated. For the analysis of the survivorship (mortality), the STATA/MP software version 14.1 (StataCorp, College Station, TX) was used. Survivorship was analysed through the Kaplan–Meier (KM) survivor function. The KM curve was performed according to the Cox-regression through the Breslow method with the hazard ratio (HR) effect measure. The confidence interval (CI) was set at 95% in all analysis. A p value < 0.05 was considered statistically significant.
Results
Search result
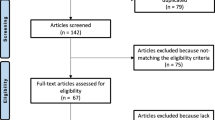
The databases searches resulted in 732 papers. First, a total of 305 articles were rejected due to duplication. Of those, only RCTs were considered, which left 77 studies for inclusion. Further 41 articles which did not match the topic were excluded, while other 19 because incompatibility with the eligibility criteria were in articles were excluded as they did not match the eligibility criteria. A further six papers were rejected as it did not report quantitative data under the outcomes of interest. This last operation left 11 RCTs for inclusion. The flow chart of literature search is shown in Fig. 1.
Methodological quality assessment
Correspondent to the above-mentioned assessment of each risk of bias, a low to moderate risk of selection bias can be reported. Attrition bias can be considered a low risk, and both performance and detection bias were moderate risks. Therefore, the methodological assessment of this work can be judged as very good quality. The review authors’ rating of each risk of bias item according to the Cochrane Collaboration is shown in Fig. 2.
Risk of publication bias
To detect possible publication bias, a funnel plot for the most commonly reported outcome (revisions) was performed. The plot evidenced an adequate symmetrical distribution of points close to the no-effect line. Moreover, none of the studies were located outside of the acceptability range, thus testifying satisfactory results. Concluding, the risk of publication bias for this study scored low. The funnel plot is shown in Fig. 3.
Patient demographic
Data from 2325 patients were collected. The mean follow-up was 58.12 ± 52.8 months. A total of 1171 samples were part of the HHA group, with a mean of 73.2% female patients and a mean age of 78.2 ± 4.6 years. The THA group accounted for 1154 patients in total with 70.7% of those being female, with a mean age of 79.4 ± 2.8 years. No differences were detected between the two groups regarding age or sex (p = 0.8 and p = 0.4, respectively). Table 1 summarizes the patient demographics.
Outcomes of interest
The overall results are shown in Table 2. Compared to THA, the HHA group reported lower values of the mean Harris hip score (MD: 3.22; 95% CI: −1.32 to 7.76; p = 0.2), surgical duration (MD: 21.75; 95% CI: 14.47 to –29.03; p < 0.0001), length of the hospitalization stay (MD: 0.8; 95% CI: − 0.90 to 2.49; p = 0.4). The HHA group evidenced lower dislocations rate (OR: 1.78; 95% CI: 1.15 to –2.77; p = 0.01, Fig. 4), but higher rate of acetabular erosion (OR: 0.08; 95% CI: 0.02 to –0.33; p = 0.0006).
At a mean of 58.12 ± 52.8 months follow-up, revisions rate scored reduced in the THA group (OR: 0.76; 95% CI: 0.48 to –1.19; p = 0.2; Fig. 5).
Subgroup analysis of RCTs < 5 years follow-up revealed reduced revision in favour of the HHA group (OR: 2.19; 95% CI: 10.9 to –4.40; p = 0.03), while subgroup analysis of RCTs > 5 years follow-up revealed reduced revision in favour of the THA group (OR: 0.25; 95% CI: 0.12 to –0.53; p = 0.0003).
The Kaplan–Meier curve detected similarity of patients survivorship between the two groups (HR: 1.06; 95% CI: 0.94 to –1.22; p = 0.3; Fig. 6).
Discussion
The main findings of the present meta-analysis were that for elderly patients with displaced femoral neck fractures, the HHA provide lower dislocations, shorter surgical duration, but higher rate of acetabular erosion compared to the THA. Revisions rate scored similar between HHA and THA. However, the subgroup analysis including only RCTs > 5 years follow-up revealed reduced revision in favour of the THA group. Hospitalization length and Harris hip score reported any statistically significant difference among the two cohorts. Concerning patients’ survivorship, the Kaplan–Meier curve found similarity among the two techniques.
In favour of HHA, decreased mean length of surgical duration was evidenced. This result was expected, since HHA requires less operative installation steps. Indeed, even if there is little variability within-technique operating time, the overall estimated effect was strongly in favour of the HHA group. These results are significantly reliable. Same observations were reported in other two RCTs not included in the comparison [20, 27].
To investigate hip function, the Harris hip score was evaluated. Yu et al. [16] in 2012 reported better Harris hip score in the THA cohort at 1, 3 and 4-year follow-up. Even the study of Burgers et al. [9] found statistically improved Harris hip score in the THA group over 300 patients. Want et al. [18] in 2015 analysed found any differences between HHA and THA within 1, 2, 4 and > 4-year follow-up. The present meta-analysis revealed a greater effect of the Harris hip score in favour of THA. This comparison suffered a high-level of heterogeneity and the final effect was not significant. We concluded, that the two groups were similar in terms of Harris hip score.
In the present meta-analysis, the comparison length of the hospitalization was affected by low grade of heterogeneity and variability, with good distribution of statistical weights. However, the final effect is not statistically significant, attesting similarity among the groups. Similar results were found by Wang et al. [18] in 2015 in a meta-analysis comparing bipolar HHA versus THA over 1014 patients. Woon et al. [32] analyzing 12,757 patients from the US National Hospital Discharge Survey found reduced hospitalisation length in the HHA cohort. Anyway, they evidenced high heterogeneity between region and hospital-size, maybe attributable to the differences in regional training and subspecialist availability. Moreover, in their analysis there was a larger proportion of THA patients was covered by private insurance to increase heterogeneity.
Concerning complications, a statistically significant reduction of the dislocation rate in the HHA group was observed. The forest plot showed variability of the weight distribution, with mostly overlapping CI. Data was in accordance with previous studies in the literature. The study by Burgers et al. [9] analysed dislocations over 800 patients with a reduced risk ratio in favour of HHA of 2.53. Similarly, Yu et al. [16] found a risk ratio of 1.99 in favour of the HHA group. Wang et al. [33] analysed dislocation at 1, 2, 4, and > 4 years follow-up. They found, only at 4 years, a statistically significant minimal reduction in favour of the HHA group (risk ratio 0.2). Zi-Sheng et al. [17] in 2012 analysed dislocations in 1122 patients, founding a statistically significant risk ratio of 0.49 in favour of the HHA group. Although HHA evidenced reduced dislocations rate, on the other hand, exposed the patients to higher risk of acetabular erosion. The analysis of acetabular erosion showed no heterogeneity among studies, attesting to this comparison high reliability and clinical relevance. The rate of erosion is far higher (OR 0.08) compared to the THA group. The higher acetabular erosion can partially explain the higher rate of revision in favour of the THA reported in the subgroup analysis (follow-up > 60 months). The comparison revision showed high concordance among the studies and results, with trustworthy results. Results in previous meta-analysis regarding implant revisions are controversial. Yu et al. [16] found a statistically significant halved risk ratio of revision in the HHA cohort, while Burgers et al. [9] found no difference at 1 year follow-up over 816 patients. Wang et al. [18] in their meta-analysis performed follow-up subgroup analyses. Similarly, they found that longer follow-up provided favourable results for the THA group (risk ratio 3.3 at > 4-year follow-up). Same observations were reported by Zi-Sheng et al. [17] in their follow-up subgroup analyses.
The Kaplan–Meier curve was performed to analyse patients’ survivorship. The result showed distinctly similarity among the two cohorts (HR 1.06, p = 0.3). This result is comparable with previous studies. Results from the US national register by Woon et al. [32] in 2017 found no difference in survivorship over 12,757 patients. Similarly, Hopley et al. [34] in their meta-analysis involving 1023 patients, found no differences between the HHA and THA (risk ratio 0.9, p = 0.8). Comparable results were found by other less recent meta-analyses [9, 16, 18, 35].
The quicker surgical duration and the sparing of healthy structures promoted by the HHA, can clarify the reduction of the total estimated blood loss, the faster recovery, the reduced post-operative attention, and the improved patients collaboration that have been reported in previous studies [5, 8, 12,13,14,15,16, 29, 32, 33, 36,37,38,39]. These features, commit that HHA should been recommend for patients with comorbidities, cognitive impairment, and reduced performance status. However, controversial concerning younger, active and healthier patients remains. Even if more at risk of dislocations, THA reported reduced acetabular erosion and longer survivorship, and may be recommended for healthy and more active patients [32, 40].
This study has several limitations. The most important limitation of the present study was given by the reduced number of included studies and related patients. In consequence of the limited evidence in the literature, no differentiation regarding surgical techniques, approaches, and implants were made. Most of the included studies differed in inclusion and exclusion criteria, thus representing another source of bias. Given these limitations, data from the present study must be interpreted with caution. The most important points of strength of this study were the extensive nature of the literature search, the rigorous methodological quality assessment of the studies, and the strictly eligibility criteria. Furthermore, the optimal baseline comparability of the samples promotes a reduction of heterogeneity and publication bias. Further clinical trials providing long-term follow-up are strongly recommended to establish the best evidence concerning both techniques.
Conclusion
For the elderly population, both HHA and THA are valid solutions to treat displaced femoral neck fractures, with comparable survivorship. HHA detected reduced dislocations, while for THA a lower risk of acetabular erosion and further revision surgeries were reported.
References
Zuckerman JD (1996) Hip fracture. N Engl J Med 334(23):1519–1525. https://doi.org/10.1056/NEJM199606063342307
Thorngren KG, Hommel A, Norrman PO, Thorngren J, Wingstrand H (2002) Epidemiology of femoral neck fractures. Injury 33(Suppl 3):C1–7
Benetos IS, Babis GC, Zoubos AB, Benetou V, Soucacos PN (2007) Factors affecting the risk of hip fractures. Injury 38(7):735–744. https://doi.org/10.1016/j.injury.2007.01.001
De Laet CE, Pols HA (2000) Fractures in the elderly: epidemiology and demography. Baillieres Best Pract Res Clin Endocrinol Metab 14(2):171–179. https://doi.org/10.1053/beem.2000.0067
Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD (2008) Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg 16(10):596–607
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6(2):99–105. https://doi.org/10.1038/nrrheum.2009.260
Parker MJ, Gurusamy K (2006) Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001706.pub3
Bhandari M, Devereaux PJ, Tornetta P 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, Schemitsch EH, Hanson BP, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt GH (2005) Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Jt Surg Am 87(9):2122–2130. https://doi.org/10.2106/JBJS.E.00535
Burgers PT, Van Geene AR, Van den Bekerom MP, Van Lieshout EM, Blom B, Aleem IS, Bhandari M, Poolman RW (2012) Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthop 36(8):1549–1560. https://doi.org/10.1007/s00264-012-1569-7
Iorio R, Schwartz B, Macaulay W, Teeney SM, Healy WL, York S (2006) Surgical treatment of displaced femoral neck fractures in the elderly: a survey of the American Association of Hip and Knee Surgeons. J Arthroplasty 21(8):1124–1133. https://doi.org/10.1016/j.arth.2005.12.008
Alolabi N, Alolabi B, Mundi R, Karanicolas PJ, Adachi JD, Bhandari M (2011) Surgical preferences of patients at risk of hip fractures: hemiarthroplasty versus total hip arthroplasty. BMC Musculoskelet Disord 12:289. https://doi.org/10.1186/1471-2474-12-289
Macaulay W, Pagnotto MR, Iorio R, Mont MA, Saleh KJ (2006) Displaced femoral neck fractures in the elderly: hemiarthroplasty versus total hip arthroplasty. J Am Acad Orthop Surg 14(5):287–293. https://doi.org/10.5435/00124635-200605000-00004
Macaulay W, Yoon RS, Parsley B, Nellans KW, Teeny SM, Consortium D (2007) Displaced femoral neck fractures: is there a standard of care? Orthopedics 30(9):748–749
Rodriguez-Merchan EC (2002) Displaced intracapsular hip fractures: hemiarthroplasty or total arthroplasty? Clin Orthop Relat Res 399:72–77
Schmidt AH, Leighton R, Parvizi J, Sems A, Berry DJ (2009) Optimal arthroplasty for femoral neck fractures: is total hip arthroplasty the answer? J Orthop Trauma 23(6):428–433. https://doi.org/10.1097/BOT.0b013e3181761490
Yu L, Wang Y, Chen J (2012) Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures: meta-analysis of randomized trials. Clin Orthop Relat Res 470(8):2235–2243. https://doi.org/10.1007/s11999-012-2293-8
Zi-Sheng A, You-Shui G, Zhi-Zhen J, Ting Y, Chang-Qing Z (2012) Hemiarthroplasty vs primary total hip arthroplasty for displaced fractures of the femoral neck in the elderly: a meta-analysis. J Arthroplasty 27(4):583–590. https://doi.org/10.1016/j.arth.2011.07.009
Wang F, Zhang H, Zhang Z, Ma C, Feng X (2015) Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis. BMC Musculoskelet Disord 16:229. https://doi.org/10.1186/s12891-015-0696-x
Cadossi M, Chiarello E, Savarino L, Tedesco G, Baldini N, Faldini C, Giannini S (2013) A comparison of hemiarthroplasty with a novel polycarbonate-urethane acetabular component for displaced intracapsular fractures of the femoral neck: a randomised controlled trial in elderly patients. Bone Jt J 95-B(5):609–615. https://doi.org/10.1302/0301-620X.95B5.31083
Rasi AMKS, Moghadam MET, Kazemian GH, Ebrahiminia MR (2014) Comparison of total hip arthroplasty (THA) and hemiarthroplasty (HA) in femoral neck fractures of elderly patients. Nova J Med Biol Sci 3(3):1–4
Tol MC, van den Bekerom MP, Sierevelt IN, Hilverdink EF, Raaymakers EL, Goslings JC (2017) Hemiarthroplasty or total hip arthroplasty for the treatment of a displaced intracapsular fracture in active elderly patients: 12-year follow-up of randomised trial. Bone Jt J 99-B(2):250–254. https://doi.org/10.1302/0301-620X.99B2.BJJ-2016-0479.R1
Investigators H, Bhandari M, Einhorn TA, Guyatt G, Schemitsch EH, Zura RD, Sprague S, Frihagen F, Guerra-Farfan E, Kleinlugtenbelt YV, Poolman RW, Rangan A, Bzovsky S, Heels-Ansdell D, Thabane L, Walter SD, Devereaux PJ (2019) Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med 381(23):2199–2208. https://doi.org/10.1056/NEJMoa1906190
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Howick J CI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford levels of evidence. Oxford Centre for Evidence-Based Medicine.https://www.cebm.net/indexaspx?o=5653. Accessed Oct 2019
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am 51(4):737–755
Avery PP, Baker RP, Walton MJ, Rooker JC, Squires B, Gargan MF, Bannister GC (2011) Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Jt Surg Br 93(8):1045–1048. https://doi.org/10.1302/0301-620X.93B8.27132
Blomfeldt R, Tornkvist H, Eriksson K, Soderqvist A, Ponzer S, Tidermark J (2007) A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Jt Surg Br 89(2):160–165. https://doi.org/10.1302/0301-620X.89B2.18576
Hedbeck CJ, Enocson A, Lapidus G, Blomfeldt R, Tornkvist H, Ponzer S, Tidermark J (2011) Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Jt Surg Am 93(5):445–450. https://doi.org/10.2106/JBJS.J.00474
Keating JF, Grant A, Masson M, Scott NW, Forbes JF (2006) Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Jt Surg Am 88(2):249–260. https://doi.org/10.2106/JBJS.E.00215
Mouzopoulos G, Stamatakos M, Arabatzi H, Vasiliadis G, Batanis G, Tsembeli A, Tzurbakis M, Safioleas M (2008) The four-year functional result after a displaced subcapital hip fracture treated with three different surgical options. Int Orthop 32(3):367–373. https://doi.org/10.1007/s00264-007-0321-1
Ravikumar KJ, Marsh G (2000) Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur—13 year results of a prospective randomised study. Injury 31(10):793–797
Woon CYL, Moretti VM, Schwartz BE, Goldberg BA (2017) Total hip arthroplasty and hemiarthroplasty: US national trends in the treatment of femoral neck fractures. Am J Orthop (Belle Mead NJ) 46(6):E474–E478
Grosso MG, Danoff JR, Padgett DE, Iorio R, Macaulay WB (2016) The cemented unipolar prosthesis for the management of displaced femoral neck fractures in the dependent osteopenic elderly. J Arthroplasty 31(5):1040–1046. https://doi.org/10.1016/j.arth.2015.11.029
Hopley C, Stengel D, Ekkernkamp A, Wich M (2010) Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ 340:c2332. https://doi.org/10.1136/bmj.c2332
Goh SK, Samuel M, Su DH, Chan ES, Yeo SJ (2009) Meta-analysis comparing total hip arthroplasty with hemiarthroplasty in the treatment of displaced neck of femur fracture. J Arthroplasty 24(3):400–406. https://doi.org/10.1016/j.arth.2007.12.009
Healy WL, Iorio R (2004) Total hip arthroplasty: optimal treatment for displaced femoral neck fractures in elderly patients. Clin Orthop Relat Res 429:43–48
Kyle RF (2009) Fractures of the femoral neck. Instr Course Lect 58:61–68
Grosso MJ, Danoff JR, Murtaugh TS, Trofa DP, Sawires AN, Macaulay WB (2017) Hemiarthroplasty for displaced femoral neck fractures in the elderly has a low conversion rate. J Arthroplasty 32(1):150–154. https://doi.org/10.1016/j.arth.2016.06.048
Rogmark C, Johnell O (2005) Orthopaedic treatment of displaced femoral neck fractures in elderly patients. Disabil Rehabil 27(18–19):1143–1149. https://doi.org/10.1080/09638280500055933
Chalmers BP, Perry KI, Hanssen AD, Pagnano MW, Abdel MP (2017) Conversion of hip hemiarthroplasty to total hip arthroplasty utilizing a dual-mobility construct compared with large femoral heads. J Arthroplasty 32(10):3071–3075. https://doi.org/10.1016/j.arth.2017.04.061
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Migliorini, F., Trivellas, A., Driessen, A. et al. Hemiarthroplasty versus total arthroplasty for displaced femoral neck fractures in the elderly: meta-analysis of randomized clinical trials. Arch Orthop Trauma Surg 140, 1695–1704 (2020). https://doi.org/10.1007/s00402-020-03409-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03409-3