Abstract
Distal radioulnar joint (DRUJ) instability is often an underestimated or missed lesion which may entail fatal consequences. The triangular fibrocartilage complex is a biomechanically very important stabilizer of the DRUJ and guarantees unrestricted range of motion of the forearm. To detect DRUJ instability a systematic examination is of uppermost importance. The contralateral healthy arm will be used for comparison during clinical examination. X-rays are required to exclude osseous lesions or deformities. Computed tomography of both wrists in neutral forearm rotation, supination, and pronation may be necessary to verify DRUJ instability in ambiguous situations. Following a systematic clinical examination wrist and DRUJ arthroscopy detects lesions definitely. Tears of the distal radioulnar ligaments which entail DRUJ instability should be repaired preferably anatomically. Ulnar-sided ligament ruptures which cause instability are detected more often than radial-sided ones. Osseous ligament avulsions are mostly refixated osteosynthetically. Ligamentous tears of the distal radioulnar ligaments may be reconstructed using anchor suture or transosseous refixation. Secondary procedures such as tendon transplants are necessary for anatomical reconstruction in cases of unrepairable ligament tears.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal radius fractures with concomitant distal radioulnar joint (DRUJ) instability are often an underestimated entity which may entail devastating consequences for the complete upper extremity [1]. Bearing the latter in mind focus on distal radius fractures does not suffice at all. The anatomical surroundings are to be examined precisely to cope with the complete extent of the injury and to draw the proper conclusions [2, 3]. This review article focuses on triangular fibrocartilage complex (TFCC) lesions as these injuries are far more common than concomitant lesions to the distal part of the interosseous membrane in the context of distal radius fractures [4, 5].
Anatomy
The TFCC is in combination with the distal part of the interosseus membrane the most important stabilizer of the DRUJ to enable unrestricted range of motion of the forearm [3, 6, 7]. The interaction of the TFCC and the distal part of the interosseous membrane are crucial to guarantee DRUJ stability [6,7,8,9,10]. Osseous structures of DRUJ are of minor significance. Basically, four sigmoid notch configurations are known: C-shaped, slope-shaped, S-shaped, and a flat configuration [11]. The latter one may predipose to greater translation of the joint partners within the DRUJ [11].
The radioulnar ligaments of the DRUJ are attached at the palmar and dorsal rims of the sigmoid notch and enclose the articular disc. The superficial fibers of the former ligaments insert at the base of the styloid process whereas the deep fibers insert at the ulnar fovea instead (Fig. 1; video 1) [7, 12].
The centric insertions of the deep fibers at the ulnar fovea and the epicentric insertions of the superficial fibers at the base of the ulnar styloid process enable smooth tension transition between these structures during pronosupination [13, 14]. These kinematic properties guarantee unrestricted forearm rotation while DRUJ stability is preserved [4, 7, 13]. Furthermore, the biomechanically irrelevant meniscus homologue is part of the TFCC and is located distal to the horizontal articular disc. This former structure is well vascularised and is often located in front of the ulnocarpal recess [15]. The ligg. ulnolunatum et ulnotriquetrum, the floor of the sixth extensor tendon compartment including the tendon sheath, and the lig. collaterale carpi ulnare complete the TFCC [15, 16].
Especially, ulnar-sided TFC tears may cause DRUJ instability with disabling consequences [4, 8, 10, 13, 17, 18]. These kind of lesions are to be detected immediately especially after treatment of distal radius fractures and should be dealt with accordingly.
Etiology
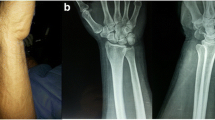
Instabilities of the DRUJ may be caused by osseous or primarily soft tissue lesions. Distal radius fractures with or without avulsion of the ulnar styloid process or forced forearm rotation are responsible for the majority of DRUJ instabilities [19, 20]. Sometimes, Galeazzi type fractures and fractures of the distal ulna may cause instability, as well. Basically, the possibility of instability rises in accordance to the proximal fracture location of the ulnar styloid process and the extent of comminution of the fracture (Fig. 2) [7, 21].
Dorso-palmar x-ray of the wrist: intra-articular distal comminuted radius fracture with proximal ulnar styloid process avulsion. Dislocation of proximal avulsion of the styloid process is the same as the radial dislocation of the radius fracture. This may correlate with intact superficial fibers. Whereas a flake fracture (Δ) of the ulna head epitomizes the avulsion of the deep fibers of the radioulnar ligaments;
Regarding soft tissue injuries, especially ulnar-sided TFC tears may cause DRUJ instability, as well [18].
Nakamura et al. distinguish between acute (< 6 months) and chronic DRUJ instabilities (> 6 months) whereas the authors do not consider the latter definition as relevant for the below outlined treatment strategy [2, 22].
Symptoms and diagnostics
Evaluation of DRUJ stability is mandatory in case of forearm fractures. The former evaluation is performed during surgery or after completion of conservative fracture treatment.
Isolated soft tissue lesions with instability are often subtle and patients often seek attendance after weeks or even months. Patients suffer typically from ulnocarpal pain with exacerbation during forced forearm rotation. Symptoms may be discreet or more debilitating depending on the extent of instability. Joint laxity and instability ought to be distinguished properly. Therefore, examination in comparison to the contralateral side is advisable. Moreover, static instability with uni- or multi-directional translation of the DRUJ partners and dynamic instability with clicking during forearm rotation are further crucial parameters to be identified [23].
These parameters ought to be analyzed:
Direction of instability
Extent of injury
Ligamentous versus osseous
Ligamentous: complete or isolated tear of either superficial or deep fibers
Quality of the TFCC: un- versus repairable
Ulna variance
Clinical history
Detailed history taking should include: analysis of trauma; precise topographic pain detection; persistent pain versus pain during load; functional deficits during forearm rotation; prior lesions; functional restrictions regarding recreational or professional activities; prior surgeries; dexterity; patient expectation [2].
Clinical examination
Swelling is often identified ulnarly and the ulna head is often prominent dorsally whereas the carpus is supinated in relation to the forearm [23, 24]. Dorsal subluxation of the ulna head is typically detected with supination loss whereas palmar subluxation of the ulna head may be seen in combination with pronation loss [25, 26].
Pronation and supination may often provoke pain around the distal ulna [23, 24, 27, 28]. "Clicking" or "snapping" sensations of the extensor carpi ulnaris tendon might be observed during forerarm rotation [26,27,28].
The following clinical test are evaluated scientifically [3].
Ulna fovea sign
Ulna fovea sign is positive whenever pain is provoked within the "soft spot" between the flexor carpi ulnaris tendon, styloid process, pisiform, and ulna head. A positive sign hints at ulnar-sided tears of the radioulnar ligaments [29].
Dorso-palmar stress test
The forearm is in neutral rotation and the examiner holds the distal radius firmly. Dorsal and palmar translation of the ulna head is applied at the same time with the second hand. Extent of translation is graded: grade 0 defines physiological articulation, grade 1 defines ligament laxity without loss of function and firm endpoint, grade 2 defines dynamic instability with loss of function without firm endpoint, and grade 3 defines spontaneous subluxation with reduction during active forearm rotation (video 2) [3, 30].
Press test
The patient pushes his hands from an armchair to stand up. If a reproducible ulnocarpal pain is provoked, this test is positive [31]. Lester et al. examined 27 patients with suspected TFCC lesions and 14 patients underwent arthroscopy because of persistent pain. TFCC lesions could be detected in all patients. The authors concluded that a 100% sensitivity regarding TFCC lesions is present. A 100% specificity was declared since a control group of 100 patients with other complaints excluding TFCC lesions were examined. In all cases a negative test was found [31].
Radiological examination
Two perpendicular oriented x-ray projections of the wrist are mandatory. Specific projections and/or projections of the contralateral side may be added. Osseous or ligamentous malformations can prevent properly performed x-rays [32]. Therefore, computed tomography may be useful in these cases.
Prerequisites for a proper lateral x-ray projection of the wrist
-
Ulnar styloid process is projected centrally to the ulna [13, 33, 34].
-
The pisiform is projected between the interval of the palmar cortex of the capitate and the palmar cortex of the distal scaphoid (Fig. 3) [35, 36].
Fig. 3 Lateral x-ray of the wrist: the pisiform is located between the palmar cortex of the capitate (left line) and the palmar cortex of the distal scaphoid (right line); the radial styloid process (outlined) is centrally oriented; lunate, triquetrum, and proximal scaphoid are overlapping each other;
-
Overlapping of proximal scaphoid, lunate, and triquetrum [32, 37].
-
Radial styloid process is projected centrally to the proximal carpal row.
Distances of greater than 6 mm between the dorsal cortex of the distal radius and distal ulna are very suspicious regarding DRUJ instability. Distances of 4–5 mm are ambiguous whereas distances of less than 3 mm are not indicative for DRUJ instability [38]. X-ray projections which are angled at least 10° from standard prevent correct interpretation of the films [37].
Prerequisites for a proper dorso-palmar x-ray projection of the wrist
-
Both radial and ulnar styloid processes are contouring the wrist [13, 33].
-
The lunate lies completely within the lunate facet [33].
Flake fractures at the ulna head (Fig. 2), proximal ulnar styloid process fractures, DRUJ gap, sagittal dislocation of distal radius fractures greater than 20°, and shortening of the radius greater than 5 mm are indicative for DRUJ instability [25, 39]. Overlapping of radius and ulna hints at a palmar luxation of the ulna whereas a wider gap may be suspicious for a dorsal luxation of the ulna [25].
Computed tomography
This technique enables the best visualization to diagnose DRUJ instability since anatomic structures do not overlap each other [40, 41]. Both wrists should be examined in neutral forearm rotation, pronation, and supination [26, 41].
Several assessment methods have been published so far [26, 32, 37, 41,42,43,44]. The radioulnar ratio method proved to be reliable and feasible during daily routine [3, 42]. A transparent template with marked concentric circles with increasing radii is put at the ulna head to determine the center of the ulna head. Then a line connecting the palmar and dorsal rims of the sigmoid notch is drawn. A line perpendicular to the latter line is then drawn through the center of the ulnar head. The distance between the dorsal and palmar rims of the sigmoid notch is measured along the line. The ratio of the latter length to the distance of both rims is finally calculated (Fig. 4) [42].
Studies which have determined physiological ratios are listed in Table 1 [40, 42, 45].
Wrist arthroscopy
Wrist arthroscopy is still the reference standard to diagnose TFCC lesions precisely (video 1 and 3, copyright Springer) [46]. Arthroscopic visualization facilitating the 3/4 portal enables direct detection of lesions regarding the superficial part and/or complete ruptures of the TFCC. A positive “Hook” test (video 3) may indirectly hint at a tear of the deep part of the TFCC whereas DRUJ arthroscopy enables direct identification of such lesions [22]. Precise classification of TFCC lesions is only possible if wrist arthroscopy is applied to initiate adequate therapy (Fig. 5, 6).
Classification of TFCC lesions according to Palmer [15];
Atzei classification regarding ulnar-sided TFCC lesions [48];
Therapy
The following treatment concept is a current strategy which proved to be reliable in our hands even with concomitant distal radius fractures [2].
Osseous avulsions of the TFCC
Examination of the DRUJ stability is mandatory intraoperatively after fixation of distal radius fractures. Especially, avulsions of the ulnar styloid process are suspicious of DRUJ instability and should be dealt with accordingly (Fig. 7). After reduction and internal fixation of the fracture the “Ballottement” test as a modified dorso-palmar stress test is performed dynamically in different rotational positions of the forearm (Fig. 8) [3, 30, 47]. Reference for the latter test is the contralateral side. Refixation of the ulnar styloid process is mandatory in case of instability (Fig. 9). Afterwards immobilization in neutral forearm rotation is recommended in a long arm cast for 2–3 weeks.
Tears of the superficial part of the TFCC (Atzei 1)
Tears of the superficial part of the TFCC may cause both pain and instability. These symptoms are often less evident than tears of the deep part of the TFCC (Atzei 3) or complete ulnar-sided lesions (Atzei 2). Arthroscopic fixation of the superficial part to the capsule may suffice in most cases [48].
Tears of the deep part of the TFCC (Atzei 3)
Anatomic refixation of the deep fibers of the radioulnar ligaments are necessary [49].
This can be achieved either arthroscopically or conventionally. The deep fibers ought to be attached at the ulnar fovea. Arthroscopic assisted transosseous refixation is done facilitating the 3/4 portal. An incision between the flexor carpi ulnaris and extensor carpi ulnaris tendons at the distal ulna reveals the base of styloid process to drill two parallel tunnels aiming at the ulnar fovea for suture fixation (Fig. 10) [50].
The mattress suture is facilitated through both tunnels (Fig. 11).
The refixation of the deep fibers can also be performed conventionally using transosseous technique or anchor suture (Fig. 12). The approach described by Garcia-Elias may be applied for both procedures (Fig. 13) [51].
Outlined skin incision for the Garcia–Elias approach (left); dissection to the extensor retinaculum (right) [51];
It is crucial to flex the elbow, elevate the forearm, and reduce the ulnar head in neutral rotation of the forearm before the suture is tightened firmly at the ulnar entrance of the tunnels. Contraindications are DRUJ osteoarthritis. A long arm cast in neutral forearm rotation is applied. Immobilization is recommended for 4 weeks. Afterwards, a Bowers splint which restricts pronation and supination to 45° in each direction may be worn for further 4 weeks (Fig. 14) [52]. Activities without restrictions are encouraged after 3 months.
Complete tears of the TFCC (Atzei 2)
Complete tears involve both the deep and superficial fibers of the distal radioulnar ligaments. These lesions should be refixated anatomically, especially for high demand patients such as athletes or adolescents [49, 53]. The conventional technique should be applied since this approach enables a precise distinction between the deep and superficial fibers [51, 53]. The deep fibers are to be attached according to the aforementioned section (Fig. 15). The superficial fibers are refixated at the base of the styloid process facilitating a third bone tunnel which is located distally to the first two parallel tunnels respectively (Fig. 16). The anatomic transosseous fixation of both fibers may restore a physiological situation [6, 10, 53, 54].
Contraindications are similar to the aforementioned technique regarding the refixation of the deep fibers.
Post-traumatic DRUJ instability with unrepairable TFCC
In case of an unrepairable TFCC the distinction between a dorsal uni-directional and a multi-directional instability is of uppermost importance. The capsule imbrication is a reliable procedure to treat dorsal uni-directional instabilities (Fig. 17) [55, 56]. This technique is easily performed and may be combined with further procedures.
It is crucial to elevate the forearm and to reduce the ulna before capsule imbrication is performed. The suturing is done in forearm supination. Contraindications are DRUJ osteoarthritis, and insufficient capsule tissue. Afterwards, a long arm cast is applied in 60° forearm supination for 4 weeks. Then a Bowers splint may be applied for further 4 weeks (Fig. 14).
In case of a multi-directional instability with unrepairable TFCC the radioulnar ligaments ought to be reconstructed. The Adams' procedure has proved its reliability [57]. Adams facilitates the palmaris longus tendon and put this tendon through a dorsal-palmar bone tunnel at the distal ulnar corner of the radius. Then the tendon is transfered and anchored within a second bone tunnel through the ulnar fovea (Fig. 18). An interference screw secures the tendon within the tunnel at the distal ulna in neutral forearm rotation. Contraindications are the same as mentioned above. Immobilization is recommended for 6 weeks in a long arm cast in neutral forearm rotation. Afterwards a Bowers splint is applied for further 4 weeks. Strenuous exercises are allowed after 6 months.
In case of a partially shrunken TFC which cannot be reattached at the ulnar fovea, Nakamura uses half of the extensor carpi ulnaris tendon which remains attached distally and fixes the tendon at the remains of TFC [58].
Current treatment concept for DRUJ instability (Fig. 19).
Conclusion
A systematic examination is crucial to diagnose and treat DRUJ instability correctly. The precise analysis of instability is the cornerstone of an adequate therapeutic strategy. Anatomic reconstruction of the TFCC is to be preferred whenever possible. Osseous avulsions with concomitant instability require osteosynthetic refixations. Ulnar-sided ligamentous TFCC tears (Palmer 1b/Atzei 3) may be treated either by transosseous mattress suture or anchor suture respectively. Ulnar-sided ligamentous TFCC tears (Palmer 1b/Atzei 2) may be treated by anatomic transosseous refixation of both superficial and deep fibers for high demand patients such as athletes or adolescents. Otherwise refixation of the deep fibers may suffice. Unrepairable, multi-directional instabilities (Atzei 4) may be reconstructed applying the Adams' procedure.
Distal radius fractures do not alter this treatment algorithm.
Up to now neither arthroscopic refixations nor open procedures have been proven to be superior regarding functional outcome [59,60,61].
References
Unglaub F, Spies CK (2018) Operative Therapie einer persistierenden palmaren Luxation im distalen Radioulnargelenk bei floridem CRPS—2 klinische Fälle. Handchir Mikrochir Plast 50:202–206. https://doi.org/10.1055/a-0645-6845
Spies CK, Prommersberger KJ, Langer M et al (2015) Instabilität des distalen Radioulnargelenks. Unfallchirurg 118:701–717. https://doi.org/10.1007/s00113-015-0044-5
Spies CK, Müller LP, Oppermann J et al (2014) Die Instabilität des distalen Radioulnargelenks—Zur Wertigkeit klinischer und röntgenologischer Testverfahren—eine Literaturübersicht. Handchir Mikrochir Plast 46:137–150. https://doi.org/10.1055/s-0033-1363662
Gofton WT, Gordon KD, Dunning CE et al (2004) Soft-tissue stabilizers of the distal radioulnar joint: an in vitro kinematic study. J Hand Surg Am 29:423–431. https://doi.org/10.1016/j.jhsa.2004.01.020
Moritomo H, Omori S (2014) Influence of ulnar translation of the radial shaft in distal radius fracture on distal radioulnar joint instability. J Wrist Surg 3:18–21. https://doi.org/10.1055/s-0033-1364093
Hagert CG (1994) Distal radius fracture and the distal radioulnar joint—anatomical considerations. Handchir Mikrochir Plast 26:22–26
Kleinman WB (2007) Stability of the distal radioulnar joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function. What we have learned in 25 years. J Hand Surg Am 32:1086–1106. https://doi.org/10.1016/j.jhsa.2007.06.014
Haugstvedt J-R, Berger Ra, Nakamura T et al (2006) Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg Am 31:445–451. https://doi.org/10.1016/j.jhsa.2005.11.008
Moritomo H (2015) The function of the distal interosseous membrane and its relevance to the stability of the distal radioulnar joint: an anatomical and biomechanical review. Handchir Mikrochir Plast 47:277–280. https://doi.org/10.1055/s-0035-1545348
Xu J, Tang JB (2009) In vivo changes in lengths of the ligaments stabilizing the distal radioulnar joint. J Hand Surg Am 34:40–45. https://doi.org/10.1016/j.jhsa.2008.08.006
Tolat AR, Stanley JK, Trail IA (1996) A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg Eur 21:587–594. https://doi.org/10.1016/S0266-7681(96)80136-7
Pan C-C, Lin Y-M, Lee T-S, Chou C-H (2003) Displacement of the distal radioulnar joint of clinically symptom-free patients. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000093906.12372.63
Hagert E, Hagert CG (2010) Understanding stability of the distal radioulnar joint through an understanding of its anatomy. Hand Clin 26:459–466. https://doi.org/10.1016/j.hcl.2010.05.002
Haugstvedt JR, Langer MF, Berger RA (2017) Distal radioulnar joint: functional anatomy, including pathomechanics. J Hand Surg. https://doi.org/10.1177/1753193417693170
Palmer AK, Werner FW (1981) The triangular fibrocartilage complex of the wrist–anatomy and function. J Hand Surg Am 6:153–162. https://doi.org/10.1097/00006534-198210000-00071
Doyle J, Botte M (2003) Surgical anatomy of the hand and upper extremity. Lippincott Williams & Wilkins, Philadelphia
Han BR, Cho YJ, Yang JS et al (2014) Clinical features of wrist drop caused by compressive radial neuropathy and its anatomical considerations. J Korean Neurosurg Soc 55:148–151. https://doi.org/10.3340/jkns.2014.55.3.148
Haugstvedt J, Berger RA, Berglund LJ et al (2002) An analysis of the constraint properties of the distal radioulnar ligament attachments to the ulna. J Hand Surg Am 27:61–67. https://doi.org/10.1053/jhsu.2002.30912
Sachar K (2012) Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am 37:1489–1500. https://doi.org/10.1016/j.jhsa.2012.04.036
Van Schoonhoven J, Prommersberger KJ, Lanz U (1999) Die bedeutung des distalen radioulnargelenks bei rekonstruktiven eingriffen nach fehlverheilten korperfernen speichenbruchen. Orthopäde 28:864–871. https://doi.org/10.1007/s001320050477
May MM, Lawton JN, Blazar PE (2002) Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg Am 27:965–971. https://doi.org/10.1053/jhsu.2002.36525
Nakamura T, Matsumura N, Iwamoto T et al (2014) Arthroscopy of the distal radioulnar joint. Handchir Mikrochir Plast 46:295–299
Wijffels MME, Brink PRG, Schipper IB (2012) Clinical and non-clinical aspects of distal radioulnar joint instability. Open Orthop J 6:204–210. https://doi.org/10.2174/1874325001206010204
Hui FC, Linscheid RL (1982) Ulnotriquetral augmentation tenodesis: a reconstructive procedure for dorsal subluxation of the distal radioulnar joint. J Hand Surg Am 7:230–236. https://doi.org/10.1016/S0363-5023(82)80171-8
Tsai PC, Pakisma DO (2009) The distal radioulnar joint. Bull NYU Hosp Jt Dis 67:90–96
Wechsler RJ, Wehbe Ma, Rifkin MD et al (1987) Computed tomography diagnosis of distal radioulnar subluxation. Skeletal Radiol 16:1–5
Breen TF, Jupiter JB (1989) Extensor carpi ulnaris and flexor carpi ulnaris tenodesis of the unstable distal ulna. J Hand Surg Am 14:612–617. https://doi.org/10.1016/0363-5023(89)90176-7
Jupiter JB (2009) Commentary: the effect of ulnar styloid fractures on patient-rated outcomes after volar locking plating of distal radius fractures. J Hand Surg Am 34:1603–1604. https://doi.org/10.1016/j.jhsa.2009.06.022
Tay SC, Tomita K, Berger RA (2007) The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg Am 32:438–444. https://doi.org/10.1016/j.jhsa.2007.01.022
Seo KN, Park MJ, Kang HJ (2009) Anatomic reconstruction of the distal radioulnar ligament for posttraumatic distal radioulnar joint instability. Clin Orthop Surg 1:138–145. https://doi.org/10.4055/cios.2009.1.3.138
Lester B, Halbrecht J, Levy IM, Gaudinez R (1995) “Press test” for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg 35:41–45
Mino DE, Palmer AK, Levinsohn EM (1985) Radiography and computerized tomography in the diagnosis of incongruity of the distal radio-ulnar joint. A prospective study. J Bone Jt Surg Am 67:247–252
Epner RA, Bowers WH, Guilford WB (1982) Ulnar variance—the effect of wrist positioning and roentgen filming technique. J Hand Surg Am 7:298–305. https://doi.org/10.1016/S0363-5023(82)80183-4
Levinsohn EM (1990) Imaging of the wrist. Radiol Clin North Am 28:905–921
Goldfarb Ca, Yin Y, Gilula La et al (2001) Wrist fractures: what the clinician wants to know. Radiology 219:11–28. https://doi.org/10.1148/radiology.219.1.r01ap1311
Yang Z, Mann FA, Gilula LA et al (1997) Scaphopisocapitate alignment: criterion to establish a neutral lateral view of the wrist. Radiology 205:865–869
Mino DE, Palmer AK, Levinsohn EM (1983) The role of radiography and computerized tomography in the diagnosis of subluxation and dislocation of the distal radioulnar joint. J Hand Surg Am 8:23–31. https://doi.org/10.1016/S0363-5023(83)80046-X
Nakamura R, Horii E, Imaeda T et al (1995) Distal radioulnar joint subluxation and dislocation diagnosed by standard roentgenography. Skeletal Radiol 24:91–94. https://doi.org/10.1007/BF00198067
Szabo RM (2006) Distal radioulnar joint instability. J Bone Jt Surg Am 88:884–894
Kim JP, Park MJ (2008) Assessment of distal radioulnar joint instability after distal radius fracture: comparison of computed tomography and clinical examination results. J Hand Surg 33:1486–1492. https://doi.org/10.1016/j.jhsa.2008.05.017
Pirela-Cruz MA, Goll SR, Klug M, Windler D (1991) Stress computed tomography analysis of the distal radioulnar joint: a diagnostic tool for determining translational motion. J Hand Surg Am 16:75–82. https://doi.org/10.1016/S0363-5023(10)80017-6
Lo IKY, MacDermid JC, Bennett JD et al (2001) The radioulnar ratio: a new method of quantifying distal radioulnar joint subluxation. J Hand Surg Am 26:236–243. https://doi.org/10.1053/jhsu.2001.22908
Nakamura R, Horii E, Imaeda T, Nakao E (1996) Criteria for diagnosing distal radioulnar joint subluxation by computed tomography. Skeletal Radiol 25:649–653. https://doi.org/10.1007/s002560050152
Min B, Park J, Kim JP (2008) Reliability and normal values of various DRUJ translation. Biomed Res. https://doi.org/10.2106/JBJS.F.01603
Park MJ, Kim JP (2008) Reliability and normal values of various computed tomography methods for quantifying distal radioulnar joint translation. J Bone Jt Surg Am 90:145–153. https://doi.org/10.2106/JBJS.F.01603
Löw S, Pillukat T, Prommersberger KJ, Van Schoonhoven J (2013) The effect of additional video documentation to photo documentation in wrist arthroscopies on intra- and interobserver reliability. Arch Orthop Trauma Surg 133:433–438. https://doi.org/10.1007/s00402-012-1670-9
Garcia-Elias M (2012) Clinical examination of the ulnar-sided painful wrist. Arthroscopic management of ulnar pain. Springer, Berlin, pp 25–44
Atzei A (2009) New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur 34:582–591. https://doi.org/10.1177/1753193409100120
Spies CK, Niehoff A, Unglaub F et al (2015) Biomechanical comparison of transosseous re-fixation of the deep fibres of the distal radioulnar ligaments versus deep and superficial fibres: a cadaver study. Int Orthop. https://doi.org/10.1007/s00264-015-2986-1
Tünnerhoff H-G (2018) Nahttechniken am Diskus. Orthopäde 47:655–662. https://doi.org/10.1007/s00132-018-3595-7
Garcia-Elias M, Smith DE, Llusá M (2003) Surgical approach to the triangular fibrocartilage complex. Tech Hand Up Extrem Surg 7:134–140. https://doi.org/10.1097/00130911-200312000-00002
Pillukat T, van Schoonhoven J (2009) Die Hemiresektions-Interpositionsarthroplastik des distalen Radioulnargelenks nach Bowers. Oper Orthop Traumatol 21:484–497. https://doi.org/10.1007/s00064-009-1913-2
Spies CK, Müller LP, Unglaub F et al (2014) Anatomical transosseous fixation of the deep and superficial fibers of the radioulnar ligaments. Arch Orthop Trauma Surg 134:1783–1788. https://doi.org/10.1007/s00402-014-2103-8
Kihara H, Short WH, Werner FW et al (1995) The stabilizing mechanism of the distal radioulnar joint during pronation and supination. J Hand Surg Am 20:930–936. https://doi.org/10.1016/S0363-5023(05)80139-X
Ahrens C, Unglaub F, Bruckner T et al (2014) Midterm functional outcome after dorsal capsular imbrication for posttraumatic instability of the distal radioulnar joint. Arch Orthop Trauma Surg 134:1633–1639. https://doi.org/10.1007/s00402-014-2092-7
Manz S, Wolf MB, Leclre FM et al (2011) Capsular imbrication for posttraumatic instability of the distal radioulnar joint. J Hand Surg Am 36:1170–1175. https://doi.org/10.1016/j.jhsa.2011.04.002
Adams BD, Berger RA (2002) An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg Am 27:243–251. https://doi.org/10.1053/jhsu.2002.31731
Nakamura T (2015) Anatomical reattachment of the TFCC to the ulnar fovea using an ECU half-slip. J Wrist Surg 04:015–021. https://doi.org/10.1055/s-0035-1544195
Anderson ML, Larson AN, Moran SL et al (2008) Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am 33:675–682. https://doi.org/10.1016/j.jhsa.2008.01.020
Andersson JK, Åhlén M, Andernord D (2018) Open versus arthroscopic repair of the triangular fibrocartilage complex: a systematic review. J Exp Orthop 5:6. https://doi.org/10.1186/s40634-018-0120-1
Luchetti R, Atzei A, Cozzolino R et al (2014) Comparison between open and arthroscopic-assisted foveal triangular fibrocartilage complex repair for post-traumatic distal radio-ulnar joint instability. J Hand Surg Eur 39:845–855. https://doi.org/10.1177/1753193413501977
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the review article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 video 1 DRUJ arthroscopy identifies the intact deep fibers of the radioulnar ligaments; copyright Springer (MP4 4675 kb)
Supplementary file2 video 2 multi-directional DRUJ instability; copyright Springer (MP4 2664 kb)
Supplementary file3 video 3 wrist arthroscopy facilitating the 3/4 portal, hook introduced via 6R portal: trampoline test enables examination of the articular disc; video shows an insufficient resilience = negative trampoline test and a positive hook test hint at a tear of the deep radioulnar ligaments: TFCC Lesion Palmer 1b/Atzei 3; copyright Springer (MP4 20233 kb)
Rights and permissions
About this article
Cite this article
Spies, C.K., Langer, M., Müller, L.P. et al. Distal radioulnar joint instability: current concepts of treatment. Arch Orthop Trauma Surg 140, 639–650 (2020). https://doi.org/10.1007/s00402-020-03371-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03371-0