Abstract
Background
Direct fixation of posterior malleolar fractures has been shown to lead to higher accuracy of fracture reduction compared to an indirect anterior to posterior fixation but lacks long-term clinical results. This study shows the mid- to long-term clinical and radiological outcome after direct fixation of the posterior malleolus through a posterolateral approach.
Materials and methods
Thirty-six patients with an ankle fracture including a posterior malleolar fragment (23 × AO-44C, 12 × AO-44B, 1 × unclassifiable) treated with direct fixation of the fragment through a posterolateral approach were retrospectively evaluated. There were 24 females (67%) with a mean age of 63 (range 34–80) years and a BMI of 28 (range 19–41) kg/m2 at the time of surgery. An initial fracture-dislocation was seen in 67%. The clinical outcome was assessed with the Visual Analog Scale (VAS, 0–10 points) and the American Foot and Ankle Society (AOFAS, 0–100 points) score. Posttraumatic osteoarthritis was recorded with the Van Dijk Classification (grade 0–III). Subgroup analyses of patient- and fracture-associated risk factors (age, BMI, smoking, fracture–dislocation, postoperative articular step-off) were assessed to reveal possible negative prognostic predictors.
Results
After a mean follow-up of 7.9 (range 3–12) years, the median VAS was 1 (IQR 0–2) point, and the median AOFAS score was 96 (IQR 88–100) points. Ankle range of motion measurements showed a significant, but clinically irrelevant, difference in plantar- and dorsiflexion between the affected and unaffected ankle. 92% of the patients were very satisfied or satisfied with the postoperative course. 89% had no preoperative signs of ankle osteoarthritis. Osteoarthritis progression was seen in 72%, with 50% showing grade II or III osteoarthritis at the final follow-up. No significant negative prognostic factors for a worse clinical outcome could be detected.
Conclusion
Direct fixation of posterior malleolar fractures through a posterolateral approach showed good clinical mid- to long-term results with a high satisfaction rate but substantial development of posttraumatic ankle osteoarthritis. Further studies should include CT analysis of the preoperative fracture morphology and even, perhaps, the postoperative reduction accuracy to evaluate the benefit of posterior malleolar fracture reduction in preventing ankle osteoarthritis in the long term.
Level of evidence
Therapeutic Level IV. See Instructions for authors for a complete description of levels of evidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ankle fractures are among the most common lower extremity injuries treated by orthopedic trauma surgeons [1,2,3,4]. Fractures of the posterior lip of the distal tibia, namely the posterior malleolus, are present in 7–44% of all ankle fractures [5,6,7,8], and are associated with a higher risk of ankle osteoarthritis and a poorer clinical outcome compared to bimalleolar fractures [7, 9,10,11].
The indications for surgical fixation of a posterior malleolar fragment (PMF) are still controversial. Historically, only the PMFs that comprised more than one-third of the distal tibial articular surface were treated with reduction and fixation. This treatment approach was notably based on a study published in 1940, which only contained eight cases [12]. Some biomechanical cadaver studies proved changes in contact area or contact peak pressure of the ankle joint in larger fragments [13,14,15]; other studies contradicted these results [16,17,18]. More recent studies, including CT evaluation, postulated that not the fragment size but rather the fragment morphology, which is given by the pathomechanism of the injury, may influence the outcome [19, 20].
Direct open reduction and internal fixation of the PMF has been shown to provide higher fragment reduction accuracy and better short-term clinical results than indirect fixation with anteroposterior screws [21,22,23]. Since malreduction of the PMF has been proven as a risk factor for the development of ankle osteoarthritis [24, 25], direct open reduction may be key to reduce this risk. So far, there is limited evidence on the long-term clinical and radiological outcome after PMF fixation, with only small case studies that often included various treatment modalities [25,26,27,28].
Therefore, the purpose of this retrospective study was to evaluate the clinical and radiological mid- to long-term outcome after direct open and internal fixation of posterior malleolar fractures through a posterolateral approach. Furthermore, we aimed to identify patient- and fracture-associated factors that could potentially influence the clinical outcome.
Patients and methods
Patient acquisition
We conducted a retrospective review of all patients treated with direct open reduction and internal PMF fixation using a posterolateral approach with a minimum follow-up of 3 years. Our hospital-own administration software was searched for radiographs of ankle fractures in our trauma unit from 2005 to 2014. All patients with an additional fracture or surgery on the affected ankle were excluded. Sixty-three eligible patients with direct PMF fixation were included in the study and contacted by telephone and letter: 13 patients could not be found, 6 patients were unwilling to participate, 3 patients moved abroad, 3 patients had died, and 1 patient could not be evaluated due to severe dementia. One patient had undergone ankle arthrodesis 5 years after the initial surgery, which led to exclusion from the final analysis. The study was approved by the local research ethics committee (EKNZ No. 2017-02057). All patients received oral and written information and signed written informed consent.
Patient data
After a mean follow-up of 7.9 (range 3.1–12.3) years, 36 patients were available for a clinical and radiological examination at our outpatient clinic. There were 12 men and 24 women with a mean age of 63 (range 34–80) years and a mean body mass index (BMI) of 28.3 (range 19.2–41.0) kg/m2 (Table 1). According to the AO/OTA Classification, the most common fracture type was 44-C2 (n = 18; 50%), followed by 44-B3 (n = 12; 33%), 44-C1 (n = 4; 11%), and 44-C3 (n = 1; 3%). Based on the Lauge–Hansen Classification, there were 23 (64%) pronation-external rotation Type IV, and 12 supination-external rotation Type IV (33%) injuries; 1 case (3%; intact fibula and posteromedial fragment with anterior subluxation of the tibia) was unclassifiable by both classifications. In 24 patients (67%), a fracture–dislocation could be seen on the initial radiographs.
Clinical evaluation
Ankle pain was evaluated with the Visual Analog Scale (VAS, 0–10 points) and ankle function with the American Orthopaedic Foot and Ankle Society Ankle Hindfoot (AOFAS, 0–100 points) score, respectively. Patients were asked to rate their satisfaction with the postoperative course based on a modified Coughlin scale (1: very satisfied, 2: satisfied, 3: partially satisfied, 4: dissatisfied) [29]. Range of motion (ROM) of ankle plantar- and dorsiflexion was measured with a goniometer. Patients’ demographical data (age, BMI, smoking) were assessed in subgroup analyses as possible negative predictive factors for a worse clinical outcome.
Radiological evaluation
All patients received plain radiographs of the affected ankle (lateral and Mortise view) at the final follow-up. These radiographs were compared to the preoperative radiographs regarding osteoarthritis development based on the Van Dijk Classification (grade 0: normal joint or subchondral sclerosis, II: osteophytes without joint space narrowing, III: joint space narrowing with or without osteophytes, III: (sub)total disappearance or deformation of the joint space) [30]. Postoperative incongruency of the distal tibial articular surface was documented as a displacement of the PMF ≥ 1 mm (so-called step-off). Initial fracture-dislocation and postoperative step-off were evaluated in subgroup analyses as possible negative predictive factors. Only a few patients of this cohort had preoperative CT scans of the affected ankle. Since previous data showed that evaluation of the posterior malleolus based on plain lateral radiographs is not reliable [31,32,33], we omitted to measure the PMF size.
Surgical technique
Surgery was performed by an experienced surgeon of the trauma team. The patient was positioned in a lateral decubitus position. A posterolateral longitudinal skin incision was made over the posterior fibular margin. After the lesser saphenous vein and sural nerve had been identified and protected, blunt dissection was performed to the flexor hallucis longus, which was peeled off the posterior tibia exposing the PMF. The fracture gap was identified and cleaned from hematoma and non-fixable small intercalated fragments. Direct fixation was performed with a buttress plate or screws.
Sixteen patients (44%) were treated with a same-day open reduction and internal fixation, whereas 20 patients (56%) received delayed definitive surgery due to soft tissue swelling or lack of operating theatre capacities or surgically skilled personnel. In six cases (17%), an external fixator was applied for temporary reduction and fixation. The mean delay from injury to surgery was 6 (range 1–18) days. The PMF was mainly fixed with one (n = 31) or two (n = 4) buttress plates (Fig. 1). In one case, two partially threaded screws were used. One-third tubular plates and screws were used in all cases with lateral malleolar fractures (n = 31). Fractures of the medial malleolus (n = 22) were fixed with one screw (n = 5), one screw and a K-wire (n = 3), two screws (n = 13), or two K-wires with a tension band construct (n = 1), respectively. Additional syndesmotic screw fixation was performed in one case.
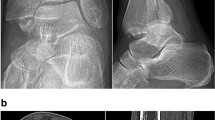
Anteroposterior and lateral radiographs of case 17, trimalleolar ankle fracture-dislocation with a large PMF. The radiographs were taken a preoperatively, b 3 months postoperatively, and c 10.7 years postoperatively (after hardware removal). Postoperative imaging documents no step-off, but OA progression of 1 K&L grade. The clinical outcome in this patient was moderate (VAS 2, AOFAS 88)
Statistics
Descriptive statistics used frequencies and percentages to present the data. All parameters were tested with Shapiro–Wilk test for normality. When the criteria for normality were met, a two-tailed t test was used. Otherwise, the Wilcoxon signed-rank test was applied. A multiple logistic regression analysis was performed to evaluate whether clinical outcomes and ankle osteoarthritis progression were associated with patient- or fracture-associated factors. All the statistical analyses were performed using SPSS version 23 software (SPSS Inc, Chicago, IL, USA).
Results
The 36 study participants showed a median VAS of 1 (interquartile range (IQR) 0–2) point and a median AOFAS score of 96 (IQR 88–100) points at the final follow-up. Plantar- and dorsiflexion of the affected ankle were significantly reduced compared to the contralateral ankle but did not differ in the median values (Table 2). Thirty patients (83%) were very satisfied, three patients (8%) satisfied, and three patients (8%) unsatisfied with the overall outcome. Several patient characteristics (age < 65 years, BMI ≥ 25 kg/m2, smoking) resulted in a non-significant tendency towards a worse clinical outcome (Table 3).
All patients showed a congruent ankle joint at the final follow-up. Osteoarthritis development based on the Van Dijk Classification is summarized in Fig. 2. Preoperatively, 89% of the patients showed no signs of ankle osteoarthritis. Osteoarthritis progression was detected in 72%, with a progression of 1 grade in 9 patients (25%), 2 grades in 14 patients (39%), and 3 grades in 3 patients (8%). At the final follow-up, 50% showed a grade II or III ankle osteoarthritis. A step-off in the articular surface was seen in five cases (14%) but did not lead to significantly poorer clinical results (Table 3).
Postoperative local complications occurred in two patients (6%). One patient had a wound-healing problem, which resolved without further intervention. Another patient presented with a painful sural nerve injury, which was treated with neurotomy. Nineteen patients (53%) underwent removal of disturbing hardware after a mean postoperative period of 1.1 (range 0.6–1.9) years. One patient received arthroscopic removal of tibial osteophytes causing anterior impingement. No other surgeries were performed during the follow-up period.
Discussion
The treatment of posterior malleolar fragments in ankle fractures remains controversial. A recent systematic review showed an overall poor outcome for ankle fractures containing a PMF; however, this review included various operative treatment methods, and 48% of the cases had been treated without fixation of the PMF [11]. In the present study, all patients underwent direct fixation of the posterior malleolus through a posterolateral approach and showed good functional results (median AOFAS of 96/100 points) with only mild residual pain (VAS 1/10 points) and a high satisfaction rate of 92% after a mean follow-up period of 7.9 years. The median values of plantar- and dorsiflexion of the affected and unaffected ankle did not differ at the final follow-up. The statistically significant ROM difference is, therefore, probably not of clinical relevance. These results are comparable to previous short-term results after direct posterior PMF fixation [34,35,36,37] and suggest that the clinical results remain stable in the long-term. Erdem et al. showed good clinical results (mean AOFAS 94) and no difference between direct posterior screw (n = 20) or plate (n = 20) PMF fixation at a mean follow-up of 3.2 years [36]. Choi et al. found similar results in 50 patients (mean AOFAS 91) after 2.2 years [37]. Forberger et al. investigated 45 patients and reported a median AAOS of 93/100 points at a follow-up of 2.1 years [34].
Several studies investigated the influence of the PMF size on the clinical outcome [7, 9, 27]. Broos et al. studied 612 ankle fractures, including 175 cases with a PMF. They found that PMFs larger than one-third of the joint surface showed worse clinical results compared to smaller unfixed fragments, even after perfect anatomical reduction [9]. De Vries et al. examined 45 ankle fractures including a PMF after a 13-year follow-up. In their study, patients who underwent fixation of the PMF did not have a significantly better outcome than patients in which the PMF was not fixed. However, the fragment size in the fixation group was significantly larger [27]. A major flaw of these previous studies is that they measured the PMF size on plain lateral radiographs. Meanwhile, other studies showed that the PMF size might be either over- or underestimated since the fracture line of the posterior malleolus is hardly ever perpendicular to the distal tibial articular surface [31,32,33]. The measurement of the PMF based on plain lateral radiographs seems, therefore, arbitrary. More recent studies described different fracture patterns of the posterior malleolus based on CT scans [19, 38, 39]. Mason and Molloy proposed a classification system, which is based on the pathomechanism of the injury pattern [19]. The authors pointed out the importance of CT scans in determining the adequate surgical approach and technique of PMF fixation [40]. In another study, the same authors found worse results for their type-3 fragments, which rather represent posterior pilon fractures, are generally larger fragments, and correlate with a more severe injury [20]. These results might be an explanation why the previous studies found worse results for fixed larger fragments compared to unfixed smaller fragments [9, 27]. Since this study lacked CT scans, we deliberately decided not to analyze the PMF size.
A step-off in the distal tibial articular surface has been claimed as a negative prognostic factor for worse clinical results and the development of osteoarthritis [24, 25, 28]. Van Hooff et al. reported on indirect anterior to posterior percutaneous screw fixation of 131 PMFs and showed a persisting articular step-off ≥ 1 mm in 42% of the cases; however, they did not analyze the rate of osteoarthritis development [26]. Verhage et al. investigated 169 patients, of which 14% had been fixed in a direct open manner. Ankle osteoarthritis was reported in 30% at a mean follow-up of 6.3 years. Patients with a malreduced posterior malleolus showed a significantly higher rate of ankle osteoarthritis compared to those with postoperative articular congruency (46% versus 25%, p = 0.02) [28]. The five cases with a postoperative articular step-off in this study did not have a significantly worse clinical outcome at the final follow-up and ankle osteoarthritis progression was observed in only three out of these five patients (60%). However, this subgroup is certainly too small to draw any conclusions.
This is the first study that provides mid- to long-term data on ankle osteoarthritis development after direct PMF fixation in a larger cohort. Anatomical reduction was achieved in 31 out of 36 cases (86%) in this study, which is comparable to the available studies reporting on reduction accuracy after direct PMF fixation (30–92%) [21, 23, 28]. Notably, 72% of the patients showed progression of ankle osteoarthritis at a mean follow-up of 7.9 years, which is a higher percentage compared to previous studies reporting on various treatment modalities for PMFs [26, 28]. One explanation might be that the follow-up in these studies was not as long as in this study. However, we also note that our radiological evaluation of the preoperative PMF morphology and postoperative reduction accuracy was limited due to the lack of CT scans, which is one of the main limitations of this study and might have led to underreporting of fragment malreduction. Moreover, the study is missing a control group of ankle fractures treated either nonoperatively or with indirect fixation. However, several studies have already shown that direct open PMF fixation leads to a significantly higher reduction accuracy as well as significantly better outcome scores compared to indirect screw fixation from anterior to posterior [21,22,23]. Vidović et al. randomized 48 patients to either direct or indirect PMF fixation and found a significantly higher reduction quality in the directly fixed group, achieving excellent reduction in 79% of the cases compared to 45% in the indirect group [21]. Shi et al. compared 64 cases with direct fixation to 52 cases with indirect fixation and found significantly higher AOFAS scores for the direct fixation group (87 vs. 80 points; (p = 0.034)) after a minimum follow-up of 12 months [23]. With the results of our study, we could show that patients who underwent direct PMF fixation were able to maintain a good clinical outcome in the longer term. Lastly, the subgroup analyses were underpowered because of the small numbers in each subgroup. We could not find any significant correlations between the above-mentioned risk factors and a poorer clinical outcome. However, patients with preoperative fracture–dislocation, BMI ≥ 25 kg/m2, and age < 65 years tended to have poorer clinical outcomes. Whereas Forberger et al. could also only detect a tendency towards poorer results for patients with fracture-dislocation [34], De Vries et al. found significant worse outcomes for fracture-dislocations compared to non-dislocated fractures [27]. Verhage et al. could show that a higher BMI was an independent significant risk factor for a worse functional outcome [28]. These patient-related factors may be, therefore, worthwhile to investigate in larger case series.
Conclusions
In conclusion, we could show that patients with direct fixation of posterior malleolar fractures through a posterolateral approach showed good clinical results and a high overall satisfaction rate, but substantial osteoarthritis development after a mid- to long-term follow-up of 3–12 years. Further studies should include CT analysis of the preoperative fracture morphology if not even the postoperative reduction accuracy to evaluate the benefit of posterior malleolar fracture reduction in preventing ankle osteoarthritis in the long term.
References
Juto H, Nilsson H, Morberg P (2018) Epidemiology of adult ankle fractures: 1756 cases identified in Norrbotten County during 2009–2013 and classified according to AO/OTA. BMC Musculoskelet Disord 19:441. https://doi.org/10.1186/s12891-018-2326-x
Daly PJ, Fitzgerald RH, Melton LJ, Llstrup DM (1987) Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand 58:539–544. https://doi.org/10.3109/17453678709146395
Jensen SL, Andresen BK, Mencke S, Nielsen PT (1998) Epidemiology of ankle fractures. A prospective population-based study of 212 cases in Aalborg, Denmark. Acta Orthop Scand 69:48–50
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697. https://doi.org/10.1016/j.injury.2006.04.130
Elsoe R, Ostgaard SE, Larsen P (2018) Foot and ankle surgery population-based epidemiology of 9767 ankle fractures. Foot Ankle Surg 24:34–39. https://doi.org/10.1016/j.fas.2016.11.002
Court-Brown CM, McBirnie J, Wilson G (1998) Adult ankle fractures—an increasing problem? Acta Orthop Scand 69:43–47. https://doi.org/10.3109/17453679809002355
Jaskulka RA, Ittner G, Schedl R (1989) Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma 29:1565–1570. https://doi.org/10.1097/00005373-198911000-00018
Koval KJ, Lurie J, Zhou W, Sparks MB, Cantu RV, Sporer SM, Weinstein J (2005) Ankle fractures in the elderly: what you get depends on where you live and who you see. J Orthop Trauma 19:635–639. https://doi.org/10.1097/01.bot.0000177105.53708.a9
Broos PL, Bisschop AP (1991) Operative treatment of ankle fractures in adults: correlation between types of fracture and final results. Injury 22:403–406
Heim D, Niederhauser K, Simbrey N (2010) The Volkmann dogma: a retrospective, long-term, single-center study. Eur J Trauma Emerg Surg 36:515–519. https://doi.org/10.1007/s00068-010-0061-6
Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S (2016) Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg 55:140–145. https://doi.org/10.1053/j.jfas.2015.04.001
Nelson MC, Jensen NK (1940) The treatment of trimalleolar fractures of the ankle. Surg Gynec Obs 71:509–514
Macko VW, Matthews LS, Zwirkoski P, Goldstein SA (1991) The joint-contract area of the ankle. The contribution of the posterior malleolus. J Bone Joint Surg Am 73:347–351. https://doi.org/10.2106/00004623-199173030-00005
Fitzpatrick DC, Otto JK, McKinley TO, Marsh JL, Brown TD (2004) Kinematic and contact stress analysis of posterior malleolus fractures of the ankle. J Orthop Trauma 18:271–278. https://doi.org/10.1097/00005131-200405000-00002
Scheidt KB, Stiehl JB, Skrade DA, Barnhardt T (1992) Posterior malleolar ankle fractures: an in vitro biomechanical analysis of stability in the loaded and unloaded states. J Orthop Trauma 6:96–101
Harper MC, Hardin G (1988) Posterior malleolar fractures of the ankle associated with external rotation–abduction injuries. Results with and without internal fixation. J Bone Joint Surg Am 70:1348–1356. https://doi.org/10.2106/00004623-198870090-00012
Vrahas M, Fu F, Veenis B (1994) Intraarticular contact stresses with simulated ankle malunions. J Orthop Trauma 8:159–166
Evers J, Fischer M, Zderic I et al (2018) The role of a small posterior malleolar fragment in trimalleolar fractures: a biomechanical study. Bone Joint J 100-B:95–100. https://doi.org/10.1302/0301-620X.100B1.BJJ-2017-0435.R1
Mason LW, Marlow WJ, Widnall J, Molloy AP (2017) Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int 38:1229–1235. https://doi.org/10.1177/1071100717719533
Mason LW, Kaye A, Widnall J, Redfern J, Molloy A (2018) Posterior malleolar ankle fractures: an effort at improving outcomes. JBJS Open Access 4:e0058. https://doi.org/10.2106/JBJS.OA.18.00058
Vidović D, Elabjer E, Muškardin IVA, Milosevic M, Bekic M, Bakota B (2017) Posterior fragment in ankle fractures: anteroposterior vs posteroanterior fixation. Injury 48:S65–S69. https://doi.org/10.1016/S0020-1383(17)30743-X
O’Connor TJ, Mueller B, Ly TV, Jacobson AR, Nelson ER, Cole PA (2015) “A to P” screw versus posterolateral plate for posterior malleolus fixation in trimalleolar ankle fractures. J Orthop Trauma 29:e151–e156. https://doi.org/10.1097/BOT.0000000000000230
Shi H, Xiong J, Chen Y, Wang JF, Qiu XS, Huang J, Gui XY, Wen SY, Wang YH (2017) Comparison of the direct and indirect reduction techniques during the surgical management of posterior malleolar fractures. BMC Musculoskelet Disord 18:109. https://doi.org/10.1186/s12891-017-1475-7
Xu HL, Li X, Zhang DY, Fu Z, Wang T, Zhang P, Jiang B, Shen H, Wang G, Wang G, Wu X (2012) A retrospective study of posterior malleolus fractures. Int Orthop 36:1929–1936. https://doi.org/10.1007/s00264-012-1591-9
Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM (2002) Results of ankle fractures with involvement of the posterior tibial margin. J Trauma 53:55–60. https://doi.org/10.1097/00005373-200207000-00012
Drijfhout van Hooff CC, Verhage SM, Hoogendoorn JM (2015) Influence of fragment size and postoperative joint congruency on long-term outcome of posterior malleolar fractures. Foot Ankle Int 36:673–678. https://doi.org/10.1177/1071100715570895
De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR (2005) Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg 44:211–217. https://doi.org/10.1053/j.jfas.2005.02.002
Verhage SM, Krijnen P, Schipper IB, Hoogendoorn JM (2019) Persistent postoperative step-off of the posterior malleolus leads to higher incidence of post-traumatic osteoarthritis in trimalleolar fractures. Arch Orthop Trauma Surg 139:323–329. https://doi.org/10.1007/s00402-018-3056-0
Coughlin MJ (1990) Arthrodesis of the first metatarsophalangeal joint with mini-fragment plate fixation. Orthopedics 13:1037–1044
van Dijk CN, Verhagen RA, Tol JL (1997) Arthroscopy For problems after ankle fracture. J Bone Joint Surg Br 79:280–284. https://doi.org/10.1302/0301-620X.79B2.7153
Ferries JS, Decoster TA, Firoozbakhsh KK, Garcia JF, Miller RA (1994) Plain radiographic interpretation in trimalleolar ankle fractures poorly assesses posterior fragment size. J Orthop Trauma 8:328–331. https://doi.org/10.1097/00005131-199408000-00009
Meijer DT, Doornberg JN, Sierevelt IN et al (2015) Guesstimation of posterior malleolar fractures on lateral plain radiographs. Injury 46:2024–2029. https://doi.org/10.1016/j.injury.2015.07.019
Meijer DT, De Muinck Keizer RJO, Doornberg JN et al (2016) Diagnostic accuracy of 2-dimensional computed tomography for articular involvement and fracture pattern of posterior malleolar fractures. Foot Ankle Int 37:75–82. https://doi.org/10.1177/1071100715603999
Forberger J, Sabandal PV, Dietrich M, Gralla J, Lattmann T, Platz A (2009) Posterolateral approach to the displaced posterior malleolus: functional outcome and local morbidity. Foot Ankle Int 30:309–314. https://doi.org/10.3113/FAI.2009.0309
Verhage SM, Boot F, Schipper IB, Hoogendoorn JM (2016) Open reduction and internal fixation of posterior malleolar fractures using the posterolateral approach. Bone Joint J 98-B:812–817. https://doi.org/10.1302/0301-620X.98B6.36497
Erdem MN, Erken HY, Burc H, Saka G, Korkmaz MF, Aydogan M (2014) Comparison of lag screw versus buttress plate fixation of posterior malleolar fractures. Foot Ankle Int 35:1022–1030. https://doi.org/10.1177/1071100714540893
Choi JY, Kim JH, Ko HT, Suh JS (2015) Single oblique posterolateral approach for open reduction and internal fixation of posterior malleolar fractures with an associated lateral malleolar fracture. J Foot Ankle Surg 54:559–564. https://doi.org/10.1053/j.jfas.2014.09.043
Bartoníček J, Rammelt S, Tuček M (2017) Posterior malleolar fractures: changing concepts and recent developments. Foot Ankle Clin 22:125–145. https://doi.org/10.1016/j.fcl.2016.09.009
Haraguchi N, Haruyama H, Toga H, Kato F (2006) Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am 88:1085–1092. https://doi.org/10.2106/JBJS.E.00856
Vosoughi AR, Jayatilaka MLT, Fischer B, Molloy AP, Mason LW (2019) CT analysis of the posteromedial fragment of the posterior malleolar fracture. Foot Ankle Int 40:648–655. https://doi.org/10.1177/1071100719830999
Acknowledgements
None of the authors have received at any time payment or services from a third party (government, commercial, private foundation, etc.) for any aspect of the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Lizzy Weigelt, Julian Hasler, Andreas Flury, Dimitris Dimitriou, and Naeder Helmy declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weigelt, L., Hasler, J., Flury, A. et al. Clinical and radiological mid- to long-term results after direct fixation of posterior malleolar fractures through a posterolateral approach. Arch Orthop Trauma Surg 140, 1641–1647 (2020). https://doi.org/10.1007/s00402-020-03353-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03353-2