Abstract
Introduction
Tenosynovial giant-cell tumor also known as pigmented villonodular synovitis (PVS) is a benign but aggressive synovial proliferative disease most often affecting the knee joint. The mainstay of therapy is surgical resection. Due to a high rate of local recurrence, radiosynoviorthesis (RSO) is used as an adjuvant method in many cases. The aim of this study was to compare local recurrence (LR) rates after surgical synovectomy with and without adjuvant RSO.
Materials and methods
From 1996 to 2014, 37 surgical interventions were performed in 32 patients with diffuse pigmented villonodular synovitis of the knee. All patients underwent open synovectomy. Adjuvant radiosynoviorthesis (RSO) was applied in 26 cases, the control group consists of 11 cases without RSO.
Results
9 (24%) lesions recurred within a median of 19 months after surgery. Of those 9 recurrences, 3 (17%) were seen in primary disease, 6 (32%) in already recurring cases (n.s.). In 26 RSO treated patients 6 (23%) recurred, in 11 patients of the control group, 3 (27%) recurred (n.s.).
Conclusions
RSO is effective in PVS as also shown in some smaller reports in the literature. But surgery is still the mainstay of therapy. RSO is not a method of compensating for an insufficient surgical approach, but it may reduce the high rate of LR in patients with large and even recurrent diffuse forms of the disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tenosynovial giant-cell tumor, historically known as pigmented villonodular synovitis (PVS) is a benign but aggressive synovial proliferative condition [4, 10]. PVS is comparatively rare with an annual incidence of about 1.8 patients/million and occurs especially in adults in their third or fourth decade of life [16]. The knee joint is the most commonly affected joint in about 50% [24].
The etiology of the lesion is unknown, but neoplastic clones found in PVS often express colony-stimulating factor 1 (CSF1) and frequently have a t(1; 2) translocation [23]. In the localized (nodular) as well as in the diffuse form, brownish, villous and nodular growth can be observed, sometimes invading the adjacent bone [14]. The clinical presentation is nonspecific with symptoms such as swelling, pain and joints locking caused by interposition of nodular lesions [2].
The mainstay of therapy is surgical resection either with marginal excision in localized disease or with total synovectomy in diffusely involved joints or tendon sheaths [6]. Conventional radiotherapy, as well as radiosynoviorthesis might also affect the rate of local recurrence or even cure the disease [19]. Local recurrence (LR) is seen in more than 20% of the cases localized in the knee with the diffuse form of the disease [1]. Therefore, adjuvant intra-articular radiation synovectomy—radiosynoviorthesis—(RSO) has been employed for decades to reduce the risk of LR. The published results in some very small series of patients seem to be favorable (Table 1) but due to a lack of comparative studies with and without RSO, the overall benefits of RSO still remain unclear.
The aim of our study was to evaluate the treatment outcomes in a large single-centre retrospective study comparing patients after surgical synovectomy with and without adjuvant RSO.
Patients and methods
Patients
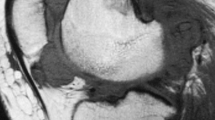
Between 1996 and 2014, 105 consecutive patients with PVS were treated in our institution and a total of 122 surgical interventions were performed. All lesions had a diagnosis of PVS based on histological features and immunohistochemistry. Preoperatively, predominantly magnetic resonance imaging (MRI) was used to define the size and localization of the tumor. All patients underwent surgical resections. This group has been described in detail before [3]. Out of those 58 (55%) patients had an involvement of the knee of which 26 (45%) were of the nodular type and 32 (55%) showed diffuse disease.
These latter 32 patients together with 37 surgeries constitute the study population. RSO was performed in 26 cases (70%). 11 Cases without RSO were used as the control.
The mean age in both groups was 49 (14–82) years. The RSO group consisted of 12 male and 14 female patients and the control group of 4 male and 7 female patients (n.s.). Patients with already recurrent disease were seen in 50% (RSO) and 46% (control) (n.s.).
The mean duration of symptoms prior to diagnosis was 26 (0–151) months in the RSO and 19.4 (0–115) months in the control group (n.s.). Progressive MRI findings were used as a marker of LR.
All patients underwent open synovectomy, in some cases additional arthroscopy for diagnostic reasons was performed prior to the actual surgical resection which consisted of a combined anterior and posterior open synovectomy. Adjuvant external beam radiotherapy or systemic targeted therapy were not utilized.
Three-phase bone scintigraphy
Three-phase bone scintigraphy was performed 24 h before RSO using a dual-detector (E.CAM, Siemens Medical Solutions, Erlangen, Germany) with a low-energy, high-resolution collimator (LEHR) and the energy window centered on the 140-keV 99mTc photopeak. Blood flow scans (first phase) consisted of serial dynamic images of the knee acquired for 2 min directly after iv injection of 500 MBq 99mTc-methylene diphosphonate (99mTc- MPD). Subsequently, blood pool images (second phase) were obtained for 2 min in the same position. Three hours later, whole-body delayed images (third phase) were acquired using a 15 cm/min table speed.
Radiosynoviorthesis (RSO)
RSO was performed under sterile conditions following a standardized protocol owing to the guidelines after the exclusion of contraindications 6–8 weeks after surgery. Under sterile conditions, the lateral suprapatellar recess was punctured, and 185 MBq (5 mCi) of 90Y-colloid was administered, after the intraarticular position of the needle tip was ensured by an injection of radiopaque contrast under fluoroscopy. Intra-articular distribution of the radiopharmacon was verified by Bremsstrahlung imaging.
Follow-up
All patients were contacted for this study and no patient had died or been lost to follow-up. MRI was used for follow-up imaging, routinely starting 3 months after surgery, then every 3 months in the 1 year, every 6 months in the second year and then yearly for 5 years. Not all patients adhered strictly to that schedule. Recurrence was defined either as a progressive typical appearance of PVS in MRI or histologically proven in a second surgery. For calculating the time to recurrence, the date of surgery was used as baseline.
Statistical analysis
For statistical analysis, the recurrence-free interval was calculated by the Kaplan–Meier method. Significance analysis was performed using the log-rank test or the Chi-square test. The data analysis software used was MedCalc®.
Ethics approval and consent to participate
This study was approved by the ethics committee of the Medical Faculty, University of Munich. Written consent was obtained from all the patients included in this study.
Results
At a median follow-up time of 49 months (14–193), 28 of the 37 resected patients showed no evidence of LR. 9 (24%) lesions recurred within a median of 19 months (3–75) after surgery (Fig. 1). From those 9 recurrences, 3 (17%) were seen in primary disease, 6 (32%) in already recurring cases (Fig. 2) (n.s.).
In 26 RSO treated patients, 6 (23%) recurred, in 11 patients of the control group 3 (27%) recurred (Fig. 3) (n-s.).
In 13 patients with local recurrences after treatment in other hospitals, 5 recurred again following second surgery in our Department. Of those five patients 3 had further surgery with a third LR in one case. In 3 cases with LR after initial resection in our Department, all 3 had a second resection and are disease free at final follow-up. Overall, out of 37 resections, four patients (11%) had LR at final follow-up. All 4 had undergone RSO.
Discussion
Radiosynoviorthesis is effective in diffuse forms of Pigmented Villonodular Synovitis. Even in tight joints as the hip RSO is an option for adjuvant therapy [9]. In this study, RSO reduced the rate of LR in patients with high-risk forms of the disease (large, recurrent, diffuse) to the moderate “normal” risk of diffuse PVS at the knee.
-
1.
Surgery is the mainstay of therapy. In a large meta-analysis including 630 patients with PVS of the knee in diffuse disease with open synovectomy and the combination of open and arthroscopic synovectomy or arthroscopic synovectomy, only LR was seen in 23% and 26%, respectively.
-
2.
To the best of our knowledge, only the study of Chin et al. in 2002 compared 5 patients with surgery alone (LR 0%), 30 with surgery and RSO (LR 15%) and 5 with surgery and external beam radiation (LR 40%). In a subset of studies including RSO, the LR rate was 14% in 43 patients, with external beam radiation 11% in 123 patients, compared to 37% in 282 patients without any form of adjuvant radiation (p < 0.001) [15]. The difference was more pronounced in patients receiving arthroscopic synovectomy only. Therefore, the authors concluded that any form of radiation therapy may have most benefit in those patients with residual disease. They also did not see any negative influence of these treatments on joint function or wound healing.
Taking into account only those 3 studies using RSO in more than 10 patients with diffuse PVS at the knee, the rate of LR was 21% in 95 patients. This reflects our own experience. The most optimistic results with 0% LR had been published in small, single-digit case series.
-
3.
The major limitation of our study is its retrospective, non-randomized character. This data has hence to be interpreted with several restrictions. The number of patients with already recurring disease was close to 50%. LR, therefore, had to be expected in a greater number of cases. In primary disease, LR was 17%, leaving not too much opportunity to lower this rate with RSO. In recurrent disease and due to the fact of our institution being a tertiary reference center, many of the cases had extensive disease and hence a worse prognosis from the outset. The indication for RSO might have been as in many retrospective studies biased by the fact that the indication for treatment was especially seen in those patients with an anticipated worse prognosis. However, and notwithstanding these limitations, our data suggests that RSO is not a method of compensating for an insufficient surgical resection, but rather that RSO might reduce the high rate of LR in patients with large and even recurrent diffuse forms of the disease to a risk similar to that of an average patient with a less problematic disease extent.
-
4.
As a second or third step in increasingly aggressive therapy, external beam radiation has to be mentioned as a further option in patients with diffuse disease for which an adequate surgical option does not exist [19]. Park et al. reported LR rates of 4 out of 23 patients (17%) treated with 12–34 Gy of external beam radiation at the knee. But in all of these patients, either arthroscopic or open synovectomy had been performed before. A LR of 0% after arthroscopic resection and radiotherapy with 20–30 Gy in 26 patients was reported by Li et al. [13]. Recently systemic approaches with an antibody blockade of CSF1R Kinase in a dose escalation study in 41 patients showed 8 subjects with stable disease and 1 with a partial response, whereas in the following treatment study on 23 patients, 12 had stable disease and 7 had partial responses [21]. Therefore, this novel therapy might present an additional option for PVS patients who have exhausted local therapies.
Conclusions
Radiosynoviorthesis is effective in diffuse forms of Pigmented Villonodular Synovitis. But surgery is still the mainstay of therapy. RSO is not a method of compensating for an insufficient surgical approach, but it may reduce the high rate of LR in patients with large and even recurrent diffuse forms of the disease. Its use should, therefore, be limited as an adjuvant therapy to patients after total synovectomy leaving no visible disease behind with a considerable risk of local recurrence.
References
Auregan JC, Klouche S, Bohu Y, Lefevre N, Herman S, Hardy P (2014) Treatment of pigmented villonodular synovitis of the knee. Arthroscopy 30(10):1327–1341
Bruns J, Ewerbeck V, Dominkus M et al (2013) Pigmented villo-nodular synovitis and giant-cell tumor of tendon sheaths: a binational retrospective study. Arch Orthop Trauma Surg 133(8):1047–1053
Capellen CF, Tiling R, Klein A, Baur-Melnyk A, Knösel T, Birkenmaier C, Roeder F, Jansson V, Dürr HR (2018) Lowering the recurrence rate in pigmented villonodular synovitis: a series of 120 resections. Rheumatology (Oxford) 57(8):1448–1452
Chassaignac M (1852) Cancer de la gaine des tendons. Gaz Hop Civ Milit 25:185–186
Chin KR, Barr SJ, Winalski C, Zurakowski D, Brick GW (2002) Treatment of advanced primary and recurrent diffuse pigmented villonodular synovitis of the knee. J Bone Joint Surg Am 84-A(12):2192–2202
Dürr HR, Stäbler A, Maier M, Refior HJ (2001) Pigmented villonodular synovitis. Review of 20 cases. J Rheumatol 28(7):1620–1630
Franssen MJ, Boerbooms AM, Karthaus RP, Buijs WC, van de Putte LB (1989) Treatment of pigmented villonodular synovitis of the knee with yttrium-90 silicate: prospective evaluations by arthroscopy, histology, and 99mTc pertechnetate uptake measurements. Ann Rheum Dis 48(12):1007–1013
Gumpel JM, Shawe DJ (1991) Diffuse pigmented villonodular synovitis: non-surgical management. Ann Rheum Dis 50(8):531–533
Hufeland M, Gesslein M, Perka C, Schroder JH (2018) Long-term outcome of pigmented villonodular synovitis of the hip after joint preserving therapy. Arch Orthop Trauma Surg 138(4):471–477
Jaffe HL, Lichtenstein L, SuroC.J (1941) Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol 31:731–765
Kat S, Kutz R, Elbracht T, Weseloh G, Kuwert T (2000) Radiosynovectomy in pigmented villonodular synovitis. Nuklearmedizin 39(7):209–213
Koca G, Ozsoy H, Atilgan HI et al (2013) A low recurrence rate is possible with a combination of surgery and radiosynovectomy for diffuse pigmented villonodular synovitis of the knee. Clin Nucl Med 38(8):608–615
Li W, Sun X, Lin J, Ji W, Ruan D (2015) Arthroscopic synovectomy and postoperative assisted radiotherapy for treating diffuse pigmented villonodular synovitis of the knee: an observational retrospective study. Pak J Med Sci 31(4):956–960
Mirra JM, Picci P, Gold RH (1989) Pigmented villonodular synovitis invading bone. In: Bone tumors, clinical, radiologic and pathologic correlations. Lea and Febiger, Philadelphia, pp 1766–1775
Mollon B, Lee A, Busse JW et al (2015) The effect of surgical synovectomy and radiotherapy on the rate of recurrence of pigmented villonodular synovitis of the knee: an individual patient meta-analysis. Bone Joint J 97-B(4):550–557
Myers BW, Masi AT (1980) Pigmented villonodular synovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 59(3):223–238
Ottaviani S, Ayral X, Dougados M, Gossec L (2011) Pigmented villonodular synovitis: a retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum 40(6):539–546
Ozturk H, Bulut O, Oztemur Z, Bulut S (2008) Pigmented villonodular synovitis managed by Yttrium 90 after debulking surgery. Saudi Med J 29(8):1197–1200
Park G, Kim YS, Kim JH et al (2012) Low-dose external beam radiotherapy as a postoperative treatment for patients with diffuse pigmented villonodular synovitis of the knee: 4 recurrences in 23 patients followed for mean 9 years. Acta Orthop 83(3):256–260
Shabat S, Kollender Y, Merimsky O et al (2002) The use of surgery and yttrium 90 in the management of extensive and diffuse pigmented villonodular synovitis of large joints. Rheumatology 41(10):1113–1118
Tap WD, Wainberg ZA, Anthony SP et al (2015) Structure-guided blockade of CSF1R kinase in tenosynovial giant-cell tumor. N Engl J Med 373(5):428–437
Ward Sr. WG, Boles CA, Ball JD, Cline MT (2007) Diffuse pigmented villonodular synovitis: preliminary results with intralesional resection and p32 synoviorthesis. Clin Orthop Relat Res 454:186–191
West RB, Rubin BP, Miller MA et al (2006) A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells. Proc Natl Acad Sci USA 103(3):690–695
Xie GP, Jiang N, Liang CX et al (2015) Pigmented villonodular synovitis: a retrospective multicenter study of 237 cases. PLoS One 10(3):e0121451
Zook JE, Wurtz DL, Cummings JE, Cardenes HR (2011) Intra-articular chromic phosphate ((3)(2)P) in the treatment of diffuse pigmented villonodular synovitis. Brachytherapy 10(3):190–194
Funding
All authors have no financial and personal relationships with other people or organizations that could inappropriately influence (bias) this work. This study was not supported by any grants or external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the ethics committee of the Medical Faculty, University of Munich.
Informed consent
Written consent was obtained from all patients included in this study.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Rights and permissions
About this article
Cite this article
Dürr, H.R., Capellen, C.F., Klein, A. et al. The effects of radiosynoviorthesis in pigmented villonodular synovitis of the knee. Arch Orthop Trauma Surg 139, 623–627 (2019). https://doi.org/10.1007/s00402-018-3097-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3097-4