Abstract
Background
Proper patellofemoral alignment is an important goal in total knee arthroplasty (TKA). Acceptable patellar alignment is defined as patellar tilt less than or equal to 5° and patellar displacement less than or equal to 5 mm. Previous studies reported an incidence of post-operative patellar malalignment in TKA from 7 to 35%. However, correlation between patellar malalignment and clinical outcome after TKA remains unclear. The purpose of the present study was to evaluate the effect of patellar tilt and displacement on the clinical outcome of TKA.
Methods
A retrospective review of 138 primary TKAs with a minimum of 2 year follow-up is reported. Pre-operative and post-operative mechanical axis, patellar tilting angle and patellar displacement were measured. Clinical outcomes were evaluated by the knee functional scores including the Knee Society Score (KSS), Knee injury and Osteoarthritis Outcome Score (KOOS), and Western Ontario McMaster University Osteoarthritis Index (WOMAC) at final follow-up.
Results
Forty-two (30%) primary TKAs had suboptimal patellofemoral alignment with a patellar tilt angle greater than 5° or lateral patellar displacement of more than 5 mm. There was no statistical difference in pre-operative mechanical axis, pre-operative patellar tilt angle, or pre-operative lateral patellar displacement between the primary TKAs with proper patellofemoral alignment and those with suboptimal alignment. Patients with post-operative patellar tilt or displacement had clinically significant reductions in KSS, KOOS, and WOMAC when compared with patients without post-operative patellar tilt or displacement. The odds of having a fair or poor post-operative result, an odds ratio of 3.4 (95% CI 1.6–7.2) for KSS, 6.4 (95% CI 2.9–14.2) for KOOS, and 5.9 (95% CI 2.6–13.5) for WOMAC, were associated with suboptimal patellofemoral alignment.
Conclusion
Establishing proper patellofemoral alignment remains an essential goal of primary TKA. There is a strong association between suboptimal post-operative patellofemoral alignment and poor clinical outcome scores after primary TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellofemoral issues remain a common post-operative complication after total knee arthroplasty (TKA). The prevalence of patellofemoral instability after TKA is between 1% and 12% [1, 2]. Mild degree of patellar maltracking, tilting or translation, may be associated with anterior knee pain and can lead to subluxation or dislocation [3,4,5]. There are several factors affecting the stability of the patellofemoral joint including prosthetic component position, overall limb alignment, rotational alignment, preparation of the patella, prosthetic design, and soft tissue balance.
Internal rotation of the femoral or tibial component increases lateral tilting and displacement of the patella. These findings are associated with patient dissatisfaction, poor functional outcomes, stiffness, and anterior knee pain after TKA [6,7,8,9,10]. Radiographs are not sufficient to assess component position in the axial plane and a computed tomography (CT) scanning is helpful in determining rotational position as a source of pain [6,7,8,9,10]. A computed tomography CT scan may be recommended in patients who present with anterior knee pain after primary TKA when no other causes are implicated. However, a patellar axial radiograph may play a major role in assessing patellofemoral alignment after TKA. Most surgeons routinely use an axial radiographic study during the routine follow-up visit. Proper patellar alignment is defined as patellar tilt less than or equal to 5° and patellar displacement less than or equal to 5 mm [11]. The correlation between patellar alignment on axial radiographs and clinical outcome after primary TKA remains the subject of debate [12,13,14]. The purpose of the present study was to evaluate the effect of patellar tilt and displacement after TKA on clinical outcome scores.
Methods
Retrospective review of 138 primary TKAs performed for osteoarthritis between January 2011 and December 2012 with minimum of 2-year follow-up was undertaken. Demographic information (age, sex, side, co-morbidities), operative information (date of surgery, lateral retinacular release) were abstracted from the medical record. 50 (36%) were male and 88 (64%) were female. The mean age was 71.3 (SD 10.3) years. The mean follow-up was 2.7 (SD 0.7) years. We excluded patients with a severe pre-operative coronal deformity (greater than 15° of varus or valgus from the mechanical axis), a severe post-operative coronal deformity (greater than 5° of varus or valgus from the mechanical axis), history of operation prior to primary TKA except knee arthroscopy for cartilage or meniscus procedure, history of knee arthroscopy to treatment of patellofemoral problems including instability or anterior knee pain syndrome and severe medical co-morbidity, lower extremity weakness, or spinal pathology and pre-operatively limited knee function. Pre-operatively 101 patients were in varus (73.2%) with a mean hip–knee ankle angle (HKA) of 7.8 (SD 3.5) degree and 37 patients were in valgus (26.8%) with a mean HKA of − 6.1 (SD 3.8) degrees. The post-operative HKA was 1.8 (SD 1.6) degrees. Knee Society Scores (KSS), Knee injury and Osteoarthritis Outcome Scores (KOOS), and the Western Ontario McMaster University Osteoarthritis Index (WOMAC) were calculated for each patient at final follow-up.
All procedures were performed by three experienced fellowship trained surgeons at a single institution. All cases utilized a medial parapatellar approach, conventional instrumentation with intramedullary alignment of the femoral component and extramedullary alignment of the tibial component. Two surgeons performed the NexGen Legacy posterior-stabilized (Zimmer Inc., Warsaw, Indiana fixed-bearing TKA) and another surgeon using the posterior-stabilized Advance Medial Pivot Knee (Wright Medical Technology Inc., Memphis, TN, USA), all were done with patellar resurfacing. Operative notes confirmed that intra-operative rotation of the femoral component referenced the transepicondylar axis and Whiteside’s line, and the rotation of the tibial component referenced the medial third of the tibial tubercle, the center of the knee and ankle joints.
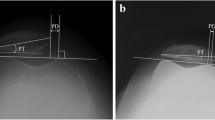
Radiographic measurements were made to determine pre-operative and final follow-up mechanical axis, patellar tilt, and patellar displacement. Mechanical axis was evaluated by a full-length hip–knee ankle radiographs made according to a previously described standardized protocol [15]. Patellar tilt and displacement were evaluated by the Merchant’s views [16]. A standard frame was used to hold the knee flexed at 45° and support the cassette at the patient’s ankle. The foot points directly upwards and the cassette holder maintains the lower border of the film parallel to the ground. The beam is aimed at approximately 60° to the horizon and tangential to the patella [12]. In this study, the pre-operative patellar tilt was defined as the angle between a line drawn from the anterior limits of the femoral condyles and a line drawn from the posterior limits of the articular surfaces of the medial and lateral facets of the patella (Fig. 1). The post-operative radiographic measurement after resurfacing was defined according to Gomes et al. [17]. Post-operative patellar tilt was defined as the angle between a line from the anterior limits of the femoral condyles and a line drawn down through the prosthesis–bone interface. Patellar displacement was measured as the distance between the center of the patella and a line drawn through the central area of the femoral condyles (Fig. 2). Acceptable patellofemoral alignment was defined as patellar tilt of less than or equal to 5° and patellar displacement of less than or equal to 5 mm [11]. All measurements were performed by one orthopedic surgeon who did not participate in the operations and was blinded with regards to demographic data and clinical outcome scores at two different intervals and reported as the mean of the measured values.
Statistical analysis
Continuous variables are presented as mean and standard deviation (SD), while categorical variables are presented as number and percent. Statistical differences in mechanical alignment, patellar tilt, patellar displacement, and clinical outcome scores between the TKAs with proper alignment of the patellofemoral joint and those without were compared using the non-paired t test. Odds ratio with 95% confidence intervals (CI) was used to evaluate risk of poor patellofemoral alignment and clinical outcome.
Results
The mean pre-operative patellar tilt was 5.5 (SD 4.7) degrees and the mean patellar displacement was 2.2 (SD 2.6) mm. The mean post-operative patellar tilt (3.4 (SD 2.4) degrees, P ≤ 0.001) was decreased after TKA but the mean patellar displacement (2.1 (SD 2.0) mm, P = 0.89) was not statistically altered after TKA. However, 38 (28%) TKAs had a patellar tilt greater than 5° and 10 (7%) TKAs had a patella displacement over 5 mm. 42 (30%) TKAs were defined as suboptimal patellofemoral alignment. There was no statistical differences in pre-operative HKA (P = 0.63), patellar tilt (P = 0.49), or patellar displacement (P = 0.82) between patients with suboptimally and properly aligned patellofemoral joints (Table 1).
In the proper patellofemoral alignment groups, the mean of post-operative patellar tilt (post-operative = 1.8 (SD 1.3), pre-operative = 5.3 (SD 4.6), P ≤ 0.001) and patellar displacement (post-operative = 1.5 (SD 1.2), pre-operative = 2.2 (SD 2.4), P = 0.01) were statistically decreased. In the suboptimal patellofemoral alignment groups, post-operative patellar tilt (mean = 6.9 (SD 2.5) degrees) was higher than pre-operative patellar tilt (mean = 5.9 (SD 4.8)) but no statistical difference was found (P = 0.26). The mean post-operative patellar displacement (3.6 (SD 2.5) mm) was statistically increased after TKA (mean pre-operative patellar displacement = 2.2 (SD 2.9) mm, P = 0.02) in the suboptimally aligned patellofemoral joints.
A lateral retinacular release was performed in 12 (9%) TKA and of these, 10 (83%) TKAs had aligned patellofemoral joints and 2 (17%) were suboptimally aligned at final follow-up.
Patients with suboptimal patellofemoral alignment were associated with significantly lower outcome scores when compared with patients with proper patellofemoral alignment in all of the knee scoring system (Table 2). The mean KSS was 124.2 (SD 25.3) in the TKAs with proper patellofemoral alignment patients and 99.9 (SD 39.2) in those with suboptimal patellofemoral alignment (P = 0.001). The mean KOOS was 85.1 (SD 39.2) in the TKAs with proper patellofemoral alignment patients and 71.0 (SD 20.0) in those with suboptimal patellofemoral alignment (P < 0.001). The mean WOMAC was 89.8 (SD 12.5) in the TKAs with proper patellofemoral alignment patients and 75.5 (SD 21.2) in those with suboptimal patellofemoral alignment (P < 0.001).
Patients who had good to excellent post-operative outcome scores, defined as more than or equal to 80% of the total points on a given outcome score, were associated with proper patellofemoral alignment (Table 3). Patients who had fair or poor post-operative outcome scores, defined as less than 80% of the total points on a given outcome score, were associated with suboptimal patellofemoral alignment (Table 3). The odds ratio of a poor outcome score with suboptimal patellofemoral mechanics was 3.4 (95% CI 1.6–7.2) for KSS, 6.4 (95% CI 2.9–14.2) for KOOS, and 5.9 (95% CI 2.6–13.5) for WOMAC.
Discussion
Proper patellofemoral tracking is an important goal in TKA. The gold standard for evaluation of patellofemoral tracking is unclear. There are several factors that affect to patellofemoral stability. The ideal investigation should evaluate patellofemoral tracking throughout the knee range of motion. However, kinematic testing of the patella femoral joint is currently limited to cadaveric study [18,19,20,21,22,23]. In vivo kinematics, and requires special radiographic methods not available in the clinic setting [24, 25].
Poor component rotation is a major cause for poor outcome after TKA. CT scan is the investigation of choice for evaluating rotational alignment in TKA. Improper component rotation has shown significant correlation to patient dissatisfaction, poor functional outcomes, stiffness and anterior knee pain after TKA [4, 6,7,8,9,10]. Bell et al. [6] compared the rotational alignment of components in 56 patients with unexplained pain following TKA with a matched control patients. They reported internal rotation of the tibial and/or femoral components to be a factor in pain following TKA. Conversely, external rotation of any of the component parameters was not identified to be a factor in painful TKA. Nicoll and Rowley [7] showed similar results in 39 painful TKA. Bédard et al. [8] demonstrated a cohort study of 52 patients (34 cases had pre-operative CT scan) with TKAs revised for stiffness. The incidence of internal rotation was 24 of 34 femoral and 33 of 34 tibial components. Bhattee et al. [9] reported a high possibility for poor outcomes after a secondary patellar resurfacing in the patients with more than 3° of femoral internal rotation. However, in the recent report, Young et al. [26] compared 71 patients with unexplained pain after primary TKA to the control cohort of 41 well-functioning TKA patients by CT scan to assess component rotation. They found no difference in both femoral and tibia component rotation between the painful and control groups. They also showed tibia component internal rotation appears to be common in both groups (49% in well-functioning TKA and 59% in painful TKA).
Conventional radiographs are routinely obtained during follow-up periods after TKA. Patellar axial view such as Merchant [16] or Laurin [27] views are widely used as the screening tool for diagnosis of patellofemoral malalignment after TKA. Suboptimal patellar alignment was defined as patellar tilt of greater than 5° or patellar displacement greater than 5 mm [1, 2]. The cut-point value was derived from the study in symptomatic patients with patellofemoral pain. In patients following TKA, the clinical utility of the patellar axial view and its correlation with functional outcome of the knee is unclear [12,13,14, 22]. Bindelgla et al. [12] evaluated 234 primary TKA with 45° Merchant view. The results showed 31% tilted over 5° and 15% displaced over 5 mm. They found no difference in the pain subscale of KSS system between well-aligned and poorly aligned knees. Barrack et al. [28] showed significant differences in component rotation with the patients with anterior knee pain compared with the control group, but no significant difference in the degree of radiographic patellar tilt or patellar subluxation was found between the two groups.
Conversely, other studies reported a positive correlation between patellar tilting or displacement with rotational alignment and clinical outcome. Bédard et al. [8] demonstrated patellar tilt and translation improved after revision TKA and was correlated with improvement of component rotational alignment and clinical outcome. Pongcharoen et al. [14] studied the incidence of poor patellar alignment and anterior knee pain using a limited medial parapatellar approach versus a mini-mid-vastus approach. They prospectively followed 60 primary TKA (30 with each approach) at minimum of 1 year post-operatively and found no difference in patellar tilt or displacement between groups and similar incidence of anterior knee pain (7%). In patellar retaining implants, patelloplasty which aimed to reduce patellar thickness and improve patellofemoral tracking have the potential to improve functional outcome and lower rate of anterior knee pain after TKA [29].
Suboptimal patellofemoral alignment is a common radiographic finding after TKA (28% have tilt and 8% have displacement). Our result is similar to the previous report by Bindelgla et al. [12]. The incidence of suboptimal patellofemoral alignment was high although all of cases were performed by 3 experienced surgeon and none of cases were planned for revision surgery. This is consistent with the finding that the majority of anterior knee pain after TKA is mild to moderate in intensity, only 8% of cases had persistent pain and rarely leading to revision TKA [30].
This study is a retrospective design. Many factors can affect to clinical outcomes cannot be controlled. Second, this study did not compare the results of conventional radiographs to CT scan. We did not directly correlate the degree of patellar tilt or displacement to axial component rotation. In the future, a well-controlled prospective study that evaluates both conventional radiographs and CT scans is warranted.
There is a strong correlation between patellofemoral alignment and clinical outcome in primary TKA. All of the knee function scoring systems in this study presented a similar trend of functional outcome between groups. Both the pain and functional subscales of all scoring systems demonstrated statistically and clinically significant differences of over 10 points. Suboptimal patellofemoral alignment correlates to an inferior clinical outcome after primary TKA. This finding advocates for the utility of conventional axial radiographs as a good screening tool for patients with unexplained pain or poor function after TKA.
References
Harwin SF (1998) Patellofemoral complications in symmetrical total knee arthroplasty. J Arthroplasty 13:753–762
Mont MA, Yoon TR, Krackow KA, Hungerford DS (1999) Eliminating patellofemoral complications in total knee arthroplasty: Clinical and radiographic results of 121 consecutive cases using the Duracon system. J Arthroplasty 14:446–455
Rand JA (2004) Extensor mechanism complications following total knee arthroplasty. JBJS-A 2062
Berger RA, Crossett LS, Jacobs JJ et al (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 144
Lakstein D, ZarrabianM, Kosashvili Y et al (2010) Revision total knee arthroplasty for component malrotation is highly beneficial: a case control study. J Arthroplasty 1047
Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B, Blyth M, McLean A (2014) Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee 21(1):272–277
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92(9):1238–1244
Bédard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469(8):2346–2355
Bhattee G, Moonot P, Govindaswamy R, Pope A, Fiddian N, Harvey A (2014) Does malrotation of components correlate with patient dissatisfaction following secondary patellar resurfacing? Knee 21(1):247–251
Panni AS, Ascione F, Rossini M, Braile A, Corona K, Vasso M, Hirschmann MT (2018) Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(6):1636–1644
Grelsamer RP, Bazos AN, Proctor CS (1993) Radiographic analysis of patellar tilt. J Bone Joint Surg Br 75(5):822–824
Bindelglass DF, Cohen JL, Dorr LD (1993) Patellar tilt and subluxation in total knee arthroplasty: relationship to pain, fixation, and design. Clin Orthop 286:103 (J Arthroplasty 1 I:507, 1996)
Bindelglass DE, Vince KG (1996) Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty. Implication for surgical technique. J Arthroplasty 11(5):507–511
Pongcharoen B, Yakampor T, Charoencholvanish K (2013) Patellar tracking and anterior knee pain are similar after medial parapatellar and midvastus approaches in minimally invasive TKA. Clin Orthop Relat Res 471(5):1654–1660. https://doi.org/10.1007/s11999-012-2778-5
McGrory JE, Trousdale RT, Pagnano MW, Nigbur M (2002) Preoperative hip to ankle radiographs in total knee arthroplasty. Clin Orthop Relat Res 404:196–202
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56-A:139 l–6
Gomes G, Scharf SC, Meltzer LP, Scott WN (1988) Patellar prosthesis positioning in total knee arthroplasty: a roentgenographic study. Clin Orthop 236:72
Kessler O, Patil S, Colwell CW Jr., D’Lima DD (2008) The effect of femoral component malrotation on patellar biomechanics. J Biomech 41(16):3332–3339
Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA (2011) The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(9):1479–1487
Merican AM, Ghosh KM, Baena FR, Deehan DJ, Amis AA (2014) Patellar thickness and lateral retinacular release affects patellofemoral kinematics in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(3):526–533
Bracey DN, Brown ML, Beard HR, Mannava S, Nazir OF, Seyler TM, Lang JE (2015) Effects of patellofemoral overstuffing on knee flexion and patellar kinematics following total knee arthroplasty: a cadaveric study. Int Orthop 39(9):1715–1722
Maderbacher G, Keshmiri A, Springorum HR, Maderbacher H, Grifka J, Baier C (2017) Influence of component rotation in total knee arthroplasty on tibiofemoral kinematics-a cadaveric investigation. J Arthroplasty 32(9):2869–2877
Calliess T, Ettinger M, Schado S, Becher C, Hurschler C, Ostermeier S (2016) Patella tracking and patella contact pressure in modular patellofemoral arthroplasty: a biomechanical in vitro analysis. Arch Orthop Trauma Surg 136(6):849–855
Sharma GB, Saevarsson SK, Amiri S, Montgomery S, Ramm H, Lichti DD, Lieck R, Zachow S, Anglin C (2012) Radiological method for measuring patellofemoral tracking and tibiofemoral kinematics before and after total knee replacement. Bone Joint Res 1(10):263–271
Slevin O, Schmid FA, Schiapparelli F, Rasch H, Hirschmann MT (2018) Increased in vivo patellofemoral loading after total knee arthroplasty in resurfaced patellae. Knee Surg Sports Traumatol Arthrosc 26(6):1805–1810
Young SW, Saffi M, Spangehl MJ, Clarke HD (2018) Unexplained pain following total knee arthroplasty: Is rotational malalignment the problem? Knee 25(2):329–334
Laurin CA, Dussault R, Levesque HP (1979) The tangential X-ray investigation of the patellofemoral joint: X-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res 144:16–26
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Cerciello S, Robin J, Lustig S, Maccauro G, Heyse TJ, Neyret P (2016) The role of patelloplasty in total knee arthroplasty. Arch Orthop Trauma Surg 136(11):1607–1613
Sensi L, Buzzi R, Giron F, De Luca L, Aglietti P (2011) Patellofemoral function after total knee arthroplasty: gender-related differences. J Arthroplasty 26(8):1475–1480
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Ethics committee approvals were obtained.
Rights and permissions
About this article
Cite this article
Narkbunnam, R., Electricwala, A.J., Huddleston, J.I. et al. Suboptimal patellofemoral alignment is associated with poor clinical outcome scores after primary total knee arthroplasty. Arch Orthop Trauma Surg 139, 249–254 (2019). https://doi.org/10.1007/s00402-018-3073-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3073-z