Abstract
Purpose
Although the spacer block technique has been recommended for the implantation of unicompartmental knee arthroplasty (UKA), there is still a lack of data concerning the resulting component positioning.
Methods
This retrospective study included 193 consecutive patients who had undergone medial UKA using the spacer technique. On the basis of the postoperative long standing radiographs, the coronal component alignment was determined in relation to the mechanical axes and the sagittal component alignment in relation to the anatomical axes of the tibia and femur. The coronal alignment of the femoral component was determined through post hoc 3D planning with the CAD data projected onto the radiograph.
Results
The angle of the tibial component was on the average 2.3° ± 2.8° in varus, the femoral component on the average 2.6° ± 3.7° in varus. Only 4 implants (2%) were outside an assumed tolerance range of 10° varus–10° valgus. A tilting from the femoral to the tibial component of more than 10° was observed in 8 cases (4%). A valgus positioning of the tibial component was followed by a valgus alignment of the femoral component (R = − 0.194, p = 0.007). An increased posterior slope of the tibial component led to an extended positioning of the femoral component (R = − 0.230, p = 0.001).
Conclusions
The spacer block technique produces results comparable to the intramedullary guided technique. However, the precision is low and outlier frequent. Due to the possibility of transferring a tibial malalignment to a femoral malalignment, even greater attention should be paid to the precision of tibial resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) produces excellent functional results and provides sufficient long-term survival [1,2,3,4,5]. In UKA, intramedullary alignment of the femoral component is increasingly being questioned [6]. The limited precision of femoral component alignment and the practice of perforating the trochlea has become the driving force behind the development of alternative techniques [7, 8]. That is in contrast to total knee arthroplasty (TKA) where the trochlea has to be replaced over the further course of the operation. Whereas navigation systems orient the femoral component perpendicularly to the mechanical axis of the femur, the so-called spacer technique aligns the distal resection of the femur parallel to the tibial resection in extension after the removal of all osteophytes. This functional approach pursues the goal of producing a rectangular medial extension gap, with the maximum contact area between the femoral and tibial component. In the process, the alignment can be checked in relation to the mechanical femoral axis, but in principle this does not play a role in adjustment of the resection plane.
Coronal alignment of the femoral component of a UKA, in contrast to that of a TKA, does not influence the leg axis but it does have an effect on the component positioning relative to each other in extension [9]. Here, the sagittal geometry of the femoral component defines the extent of the tolerable malalignment and, e.g., for the Oxford UKA is stated as ± 10° [9,10,11,12,13]. For the extension/flexion of the femoral component, a narrower tolerance range of ± 5° in relation to the distal femoral anatomical axis is noted [9,10,11,12,13].
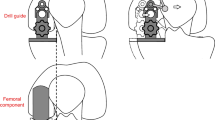
The spacer block technique has been recommended by many manufacturers for the implantation of UKA over a number of years (Zimmer, S&N, DePuy and others). In this technique, the femoral component is aligned according to the tibial cut by introducing a spacer in extension after cutting the tibia (Fig. 1). This spacer is connected to the distal femoral cutting block, so that the femoral cut is aimed to be parallel to the tibia cut in extension. Based on this, the resulting distal femoral cut is independent of the anatomical and mechanical axis of the femur.
Using a spacer to evaluate appropriately the medial joint gap and align the distal femoral cut requires knowledge about the physiological tension of this gap. Suzuki et al. assessed this gap using a dedicated tensioning device [14]. They showed a correlation between tensioning force and gap size. The gap became 2.5 mm wider when applying a 150 N instead of a 50 N force, thus corresponding to a “tight” and “loose” feeling when introducing a spacer. Consistently, and independent of the tensioning force, the flexion gap was 1 mm wider than the extension gap. Introduction of a spacer should therefore result in a flexion gap that is 1 mm looser than the extension gap. Ten Ham et al. reproduced this tension profile of the medial joint gap in a better fashion when using a spacer instead of a tensioning device [15]. The latter resulted in an equal joint gap in extension and flexion. The authors concluded that the valgus laxity found with the spacer-guided system approximated the physiological valgus laxity more closely.
Although the results of the spacer block technique in reconstructing physiological joint tension in extension and flexion are promising, there still appears to be a lack of data concerning the resulting position of the femoral component in the coronal and sagittal planes.
The objective of the present study was therefore, to the best of our knowledge for the first time, to determine in what position and at what degree of flexion a femoral component inserted using the spacer technique is implanted in relation to the mechanical femoral axis. In addition, it was to be investigated whether the intraoperatively adjusted parallel medial gap between the distal femoral and tibial resection also remains parallel in follow-up, and what patient-specific or intraoperative factors influence this.
Materials and methods
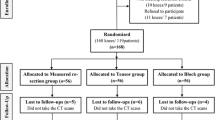
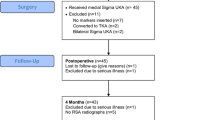
This retrospective study included 193 consecutive patients who had undergone medial UKA using the spacer technique (ZUK, Zimmer, now Lima). Before the start of the study, the approval of the local ethics committee was obtained (4833–06/16). Patient-specific data (age, sex, height, weight) were taken from the files. Preoperative and postoperative whole leg standing radiographs were available for all patients. On the basis of the preoperative and postoperative images, the leg axes were determined as the angle between the hip joint center, knee joint center, and ankle joint center. The coronal and sagittal position of the tibial component was determined from the digital postoperative images as the angle between the mechanical axis and the clearly visualized lower edge of the tibial plateau. Whereas the flexion of the femoral component could be measured as the angle between the femoral fixation pins and the anterior cortical bone of the distal femur, this was not possible in the coronal plane.
Here, a post hoc three-dimensional planning of the femoral component was performed on the basis of the respective CAD data in projection onto the postoperative radiograph. For this, the component which was projected three-dimensionally onto the radiograph was rotated and moved in space until its shadow best matched the radiographic projection (Fig. 2). The adjusted angle of the coronal alignment was determined in relation to the mechanical femoral axis (Fig. 3).
This method was validated using five sawbones having femoral components aligned precisely between 5° valgus and 15° varus (− 5°, 0°, 5°, 10°, and 15°). The observer was the same person who analyzed the patients’ radiographs (T.M.) and was blinded against the given femoral alignment. The difference between measured and given femoral alignment was between 0.3° and 1.2°, so that the method showed a sufficient precision to test the study hypothesis.
From the tibial and femoral coronal alignments thus determined, the asymmetry of the medial extension gap could be calculated as the deviation from parallelism.
The Pearson correlation coefficient was calculated on a significance level of 0.05 to test for correlation between the femoral and tibial component alignment.
Results
The average age of the 111 male and 82 female patients was 64.9 ± 8.3 (46–86) years (Table 1). The preoperative leg axis was on the average 5.8° ± 3.6° in varus (3° valgus–22° varus). Postoperatively, the leg axis was only 1.7° ± 3.3° in varus (8° valgus–10° varus). The tibial component was inserted on the average 2.3° ± 2.8° in varus (5° valgus–10° varus), the average posterior slope was 5.0° ± 2.5° (0°–11°). The femoral component was not aligned perpendicular to the mechanical axis, but was on the average 2.6° ± 3.7° in varus, whereby the range extended from 12° varus to 9° valgus (Fig. 4a). Only 4 implants (2%) were outside an assumed tolerance range of 10° varus–10° valgus [9,10,11,12,13].
The average flexion of the femoral components was − 2.4 ± 5.0°, with a range between 17° extension and 14° flexion (Fig. 4b). Assuming a tolerance range of ± 5°, 127 implants (66.1%) were implanted correctly.
In accordance with the spacer block technique, the position of the femoral component was determined in both planes from the position of the tibial component. In the coronal plane, a valgus positioning of the tibial component was followed by a valgus alignment of the femoral component (R = − 0.194, p = 0.007). In the sagittal plane, an increased posterior slope of the tibial component led to an extended positioning of the femoral component (R = − 0.230, p = 0.001). As a result of this femoral alignment being dependent on tibial alignment, an average parallel position of femoral to tibial component ensued, with 0.3° ± 5.1° asymmetry. However, there is a remarkable range of between 13° valgus and 15° varus tilting of the components in the coronal plane. Assuming a tolerable range of ± 10°, 8 UKAs (4%) were therefore outside of the tolerance range. The asymmetry of implants in the coronal plane that resulted despite the spacer-dependent parallel intraoperative alignment of the implants in extension was not found to be dependent on any of the parameters recorded here.
Discussion
The main result of the present study is that the femoral component is implanted systematically in a slight varus of 2.6° by the spacer block technique, with a considerable overall range of 21°. However, these values do not differ from the alignment that is achieved through an intramedullary alignment. Here, Gulati et al. also showed an approximately 1.4° ± 4.0° varus positioning of the femoral component with an overall range of 21.4° (8.9° valgus–12.5° varus) [10]. Again with intramedullary alignment, Shakespeare et al. determined a range of between 10° varus and 10° valgus at average neutral alignment [11]. For coronal alignment of the femoral component, Kim et al. achieved a range of between 11° valgus and 8° varus, again at average neutral alignment [9].
However, since the leg axis is dependent on the level of the distal femoral resection and not on the alignment of the femoral component [16], the extent of the axial correction by UKA remains identical to data in the literature. In this study, the leg axis was changed on the average by 4.1° ± 5.2° valgus, whereby Inoue et al. in fact observed 4.1° ± 1.9° [17].
The overall range of the sagittal femoral alignment was 31° in the present study, which means that 33.9% of all femoral components were outside an assumed tolerance range of ± 5°. This is in line with the results of Clarius et al., who also showed an overall range of 30° accompanied by 32% outliers in his study [18]. Additionally, in the study conducted by Müller et al., 34% of the components were outside the tolerance range [19]. However, the data available on sagittal alignment of the femoral component after intramedullary alignment appear to be inconclusive, since Shakespeare et al. state just 8% outliers [11], and Gulati et al. even observed no outliers at all in an extended tolerance range of ± 10° [10].
As a recent result of unsatisfactory implantation, precision-customary instruments are continuously being enhanced. Tu et al. confirmed an improved component alignment using the latest instruments in comparison with conventional instruments of the last generation [20]. They had only 5% outliers in every observed plane (femoral and tibial) although the tolerance range was defined to be only ± 3° for both components and planes. In contrast to that, Jang et al. claimed that they failed to show any benefit of this new instrument system in comparison to instruments of the last generation with wider tolerance ranges (femur coronal ± 10°, sagittal 15°, tibial coronal ± 5°) [12]. Hence, the potential to improve precision of implantation simply by improving conventional instruments remains uncertain in the literature.
Weber et al. included one randomized controlled study and nine cohort trials in a meta-analysis regarding the effect of navigation on implantation precision in UKA [21]. The navigated implantations produced significantly less outliers in all planes observed (femoral and tibial, coronal and sagittal) than the conventional implantations did. Zhang et al. confirmed this result in a more recent publication for UKA implanted using a minimally invasive approach [22].
Gaudiani et al. demonstrated an excellent reconstruction of the tibial joint line in the coronal plant using robotics, but here they observed a systematic trend towards increased tibial slope compared to the preoperative status [23]. In a meta-analysis, van der List et al. included only studies with a conventionally operated control group and demonstrated a higher precision of robotics for implantation of UKA [24]. For robotics compared to conventional instruments, Cobb et al. showed a better reconstruction of the mechanical whole leg axis [25]. Lonner et al. and MacCallum et al. observed a higher precision of tibial alignment in the coronal and sagittal plane [26, 27].
In contrast to computer-assisted implantation techniques like those involving robotics and navigation, patient-specific instruments (PSI) have failed to show consistently an improvement in UKA component alignment. Alvand et al. did not observe any difference in tibial and femoral component alignment after comparing PSI with conventional implantation [13]. PSI resulted even more often in a tibial resection making higher inserts necessary than in the conventional control group. Consistently van Leeuwen et al. demonstrated significant differences between the preoperatively planned and the resulting component alignments when using PSI (for the femoral component in the sagittal plane, and for the tibial component in the coronal plane) [28].
The fact that the spacer block technique achieves a precision in alignment of the femoral component comparable to that of the intramedullary technique supports the further use of this surgical technique. Nevertheless, the present results show that the intraoperatively symmetrically resected medial extension gap basically also leads to a parallel position of the implants in the coronal plane, but in 4% of the cases to outliers with more than 10° asymmetry. Corresponding data from intramedullary-aligned UKA are lacking, so that this result cannot be evaluated in the context of the intramedullary-aligning technique. The danger of edge loading resulting from the tilted position of the implants in the coronal plane is dependent on the geometry of the femoral component, so that rounded designs would appear to be advantageous here [29].
In conclusion, the results show that the spacer block technique produces results comparable to the intramedullary guided technique, but less precise than those using navigation or robotics. Overall, the precision is low, and outliers frequent. Due to the possibility of transferring a tibial malalignment to a femoral malalignment, even greater attention should be paid to the precision of tibial resection in the spacer block technique.
References
Iacono F, Raspugli GF, Akkawi I et al (2016) Unicompartmental knee arthroplasty in patients over 75 years: a definitive solution? Arch Orthop Trauma Surg 136:117–123. https://doi.org/10.1007/s00402-015-2323-6
Hawi N, Plutat J, Kendoff D et al (2016) Midterm results after unicompartmental knee replacement with all-polyethylene tibial component: a single surgeon experience. Arch Orthop Trauma Surg 136:1303–1307. https://doi.org/10.1007/s00402-016-2515-8
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2017) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4817-y
Mohammad HR, Strickland L, Hamilton TW, Murray DW (2017) Long-term outcomes of over 8,000 medial Oxford Phase 3 Unicompartmental Knees-a systematic review. Acta Orthop. https://doi.org/10.1080/17453674.2017.1367577
Matziolis G, Röhner E (2015) Arthritis of the medial knee joint compartment. Z Orthop Unfall 153:553–564. https://doi.org/10.1055/s-0035-1557834 (quiz 565–6)
Levine B, Rosenberg AG (2014) The simple unicondylar knee: extramedullary technique. Clin Sports Med 33:77–85. https://doi.org/10.1016/j.csm.2013.06.003
Kort NP, van Raay JJAM., Thomassen BJW (2007) Alignment of the femoral component in a mobile-bearing unicompartmental knee arthroplasty: a study in 10 cadaver femora. Knee 14:280–283. https://doi.org/10.1016/j.knee.2007.04.007
Ma B, Long W, Rudan JF, Ellis RE (2006) Three-dimensional analysis of alignment error in using femoral intramedullary guides in unicompartmental knee arthroplasty. J Arthroplasty 21:271–278. https://doi.org/10.1016/j.arth.2004.07.012
Kim JG, Kasat NS, Bae JH et al (2012) The radiological parameters correlated with the alignment of the femoral component after Oxford phase 3 unicompartmental knee replacement. J Bone Jt Surg Br 94:1499–1505. https://doi.org/10.1302/0301-620X.94B11.29217
Gulati A, Chau R, Simpson DJ et al (2009) Influence of component alignment on outcome for unicompartmental knee replacement. Knee 16:196–199. https://doi.org/10.1016/j.knee.2008.11.001
Shakespeare D, Ledger M, Kinzel V (2005) Accuracy of implantation of components in the Oxford knee using the minimally invasive approach. Knee 12:405–409. https://doi.org/10.1016/j.knee.2005.03.003
Jang K-M, Lim HC, Han S-B et al (2017) Does new instrumentation improve radiologic alignment of the Oxford® medial unicompartmental knee arthroplasty? Knee 24:641–650. https://doi.org/10.1016/j.knee.2017.02.001
Alvand A, Khan T, Jenkins C et al (2017) The impact of patient-specific instrumentation on unicompartmental knee arthroplasty: a prospective randomised controlled study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4677-5
Suzuki T, Ryu K, Kojima K et al (2015) Evaluation of spacer block technique using tensor device in unicompartmental knee arthroplasty. Arch Orthop Trauma Surg 135:1011–1016. https://doi.org/10.1007/s00402-015-2231-9
Ham ten AM, Heesterbeek PJC, van der Schaaf DB et al (2013) Flexion and extension laxity after medial, mobile-bearing unicompartmental knee arthroplasty: a comparison between a spacer- and a tension-guided technique. Knee Surg Sports Traumatol Arthrosc 21:2447–2452. https://doi.org/10.1007/s00167-012-2021-7
Kim S-J, Bae J-H, Lim HC (2012) Factors affecting the postoperative limb alignment and clinical outcome after Oxford unicompartmental knee arthroplasty. J Arthroplasty 27:1210–1215. https://doi.org/10.1016/j.arth.2011.12.011
Inoue A, Arai Y, Nakagawa S et al (2016) Comparison of alignment correction angles between fixed-bearing and mobile-bearing UKA. J Arthroplasty 31:142–145. https://doi.org/10.1016/j.arth.2015.07.024
Clarius M, Hauck C, Seeger JB et al (2010) Correlation of positioning and clinical results in Oxford UKA. Int Orthop 34:1145–1151. https://doi.org/10.1007/s00264-009-0881-3
Müller PE, Pellengahr C, Witt M et al (2004) Influence of minimally invasive surgery on implant positioning and the functional outcome for medial unicompartmental knee arthroplasty. J Arthroplasty 19:296–301
Tu Y, Xue H, Ma T et al (2017) Superior femoral component alignment can be achieved with Oxford microplasty instrumentation after minimally invasive unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:729–735. https://doi.org/10.1007/s00167-016-4173-3
Weber P, Crispin A, Schmidutz F et al (2013) Improved accuracy in computer-assisted unicondylar knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 21:2453–2461. https://doi.org/10.1007/s00167-013-2370-x
Zhang Z, Zhu W, Zhu L, Du Y (2016) Superior alignment but no difference in clinical outcome after minimally invasive computer-assisted unicompartmental knee arthroplasty (MICA-UKA). Knee Surg Sports Traumatol Arthrosc 24:3419–3424. https://doi.org/10.1007/s00167-014-3456-9
Gaudiani MA, Nwachukwu BU, Baviskar JV et al (2017) Optimization of sagittal and coronal planes with robotic-assisted unicompartmental knee arthroplasty. Knee 24:837–843. https://doi.org/10.1016/j.knee.2017.05.002
van der List JP, Chawla H, Joskowicz L, Pearle AD (2016) Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc 24:3482–3495. https://doi.org/10.1007/s00167-016-4305-9
Cobb J, Henckel J, Gomes P et al (2006) Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Jt Surg Br 88:188–197. https://doi.org/10.1302/0301-620X.88B2.17220
Lonner JH, John TK, Conditt MA (2010) Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res 468:141–146. https://doi.org/10.1007/s11999-009-0977-5
MacCallum KP, Danoff JR, Geller JA (2016) Tibial baseplate positioning in robotic-assisted and conventional unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol 26:93–98. https://doi.org/10.1007/s00590-015-1708-0
van Leeuwen JAMJ., Röhrl SM (2017) Patient-specific positioning guides do not consistently achieve the planned implant position in UKA. Knee Surg Sports Traumatol Arthrosc 25:752–758. https://doi.org/10.1007/s00167-016-4268-x
Argenson J-NA, Parratte S (2006) The unicompartmental knee: design and technical considerations in minimizing wear. Clin Orthop Relat Res 452:137–142. https://doi.org/10.1097/01.blo.0000229358.19867.60
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matziolis, G., Mueller, T., Layher, F. et al. The femoral component alignment resulting from spacer block technique is not worse than after intramedullary guided technique in medial unicompartimental knee arthroplasty. Arch Orthop Trauma Surg 138, 865–870 (2018). https://doi.org/10.1007/s00402-018-2911-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2911-3