Abstract
Introduction
The clavicle exhibits considerable movement in three planes making rigid fixation challenging. The addition of a second plate may be considered to improve fixation rigidity, but risks compromising the blood supply to the fracture site. The purpose of this study is to assess if extraperiosteal dual plate fixation increases the rate of non-union, reoperation, and complications at 1 year for surgically treated acute mid-shaft clavicle fractures.
Methods
Between June 1998 and June 2013, surgically treated mid-shaft clavicle fractures undergoing open reduction internal fixation within 4 weeks of injury were retrospectively reviewed. Patients undergoing single plate fixation were compared to dual plate fixation. Patients were followed for a minimum of 1 year. Charts were reviewed to assess union rates, reoperation, and complications.
Results
One hundred and sixty-three clavicles (125 single plates, 34 dual plates) were evaluated. All patients (100%) in dual plating group and one hundred and fourteen (91%) in single plating group obtained bony union by 1 year (p = 0.13). Six patients (4.8%) experienced a non-union in the single plating cohort compared to the dual plating cohort who had a 100% union rate. Seven patients required reoperation in the single plate cohort due to implant failure (N = 4), infection (N = 2), and non-union (N = 1).
Conclusions
This limited series of patients demonstrates dual plate fixation is a reliable option for acute mid-shaft clavicle fractures, with excellent union rates and low complication rates. Compared to single plate fixation, no significant differences in outcomes were identified. In the case of more complex fracture patterns, application of a second extraperiosteal plate may be utilized without compromising healing or increasing complication rates.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Mid-shaft clavicle fractures are relatively common accounting for 10% of all fractures [1, 2]. Although these fractures occur in a relatively high-frequency non-union rates remain low, with a reported rate of 2.2%, compared to 15% for those treated non-operatively [3, 4]. One known risk factor for non-union is inadequate fracture fixation leading to excess motion through the fracture site. In cases with increased fracture complexity, surgeons may consider dual plate fixation to improve construct rigidity. However, additional fixation often places the blood supply to the fracture site at risk secondary to soft-tissue exposure.
We hypothesized that the addition of a second plate would not compromise bony union or increase complications. A stiffer construct can be obtained with the addition of a second plate as compared to single plate fixation [5, 6]. This was also demonstrated more recently by Prasarn et al. who utilized dual minifragment plates in a biomechanical study, comparing them to single locking plates [7]. For this reason, dual plates have been used for the treatment of non-unions with high rates of healing [8, 9]. Studies examining the results of dual plate fixation of acute mid-shaft clavicle fractures remain limited [10]. The purpose of this study is to compare the rate of non-union, reoperation, and complications at 1 year for surgically treated acute mid-shaft clavicle fractures when extraperiosteal dual plate fixation is used in place of the conventional single plate fixation.
Patients and methods
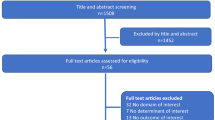
Over a 15 year period (June 1998–June 2013), 188 consecutive acute mid-shaft clavicle fractures were treated at a single institution with open reduction internal fixation. Indications for surgery included greater than 100% fracture displacement and 2 cm or more of shortening. One hundred and forty-seven were treated with a single plate and forty-one with dual plate fixation. A subset of patients treated with dual plating has previously published as a technique article [10]. Clinical charts were reviewed for patient characteristics, and clinical and radiographic outcomes. Immediate postoperative radiographs were reviewed for quality of reduction (excellent/fair/poor) with 92% of patients in the single plate cohort demonstrating excellent reduction (135) with the remaining patients having a 7% fair (9) and 2% poor reduction (3). The dual plate cohort demonstrated 93% had an excellent reduction (38) and 7% had a good reduction (3). Patients were included if they had an acute (≤28 days), displaced mid-shaft clavicle fracture; a fracture treated with plate fixation (single plating or dual plating technique); age greater than or equal to 18 years; follow-up of at least 1 year or until fracture union. Patients were excluded if they had a pathologic fracture, previous surgery on the same clavicle, or a prior ipsilateral clavicle fracture.
Three trauma fellowship trained surgeons performed all surgeries. Fracture patterns and surgeon preference dictated the number and types of plates utilized. Surgeons routinely took into account fragment position, disruption of the periosteum, the sequence of reduction, plate properties, and weight-bearing requirements of the patient when choosing fixation.
Both groups were similar in regards to age, sex, involved side, hand dominance, injury mechanism, and tobacco use (see Table 1). Type C fractures were more common in the dual plate fixation group (8.0 vs 32.3%, p = 0.001). Average time from injury to surgery was similar in both groups (8.1 vs 9.8 days, p = 0.16).
Radiographic union was assessed at routine follow-up visits which occur at 2 weeks, 6 weeks, 3 months, and every 2–3 months until union. Radiographic evaluations were performed utilizing clavicle anteroposterior (AP) views with caudal-tilt and cephalic-tilt to assess for union, delayed union, malunion, non-union, and implant failure at each follow-up visit. Complications assessed included: implant removal, refracture after implant removal, reoperation, infection, plate prominence, and peri-incisional numbness.
Statistical analysis
Patients were divided into two groups based on the use of single plate fixation (Single plating group) versus dual plate fixation (Dual plating group). Statistical analysis was performed with SPSS software (version 13.0, SPSS, Chicago, Illinois). Standard statistical analysis was performed with the assistance of a statistician. Student t test, Chi-square test, and Fisher’s exact test were performed in the analysis, to compare the union rate, reoperation rate, and complications between the two groups. All tests were two-sided, and the level of significance was set at alpha <0.05.
Results
Fixation characteristics
Fractures were fixed with a variety of plates per the surgeon’s preference. In the single plating group, 51 clavicles (40.8%) were fixed with locking plates and 74 (59.2%) with reconstruction plates. 73 plates (58.4%) were placed on the anteroinferior aspect of the clavicle and 52 plates (41.6%) were placed on the superior aspect of the clavicle. In the dual plating group, 12 clavicles (35.3%) were fixed using tubular & locking plates, 22 clavicles (64.7%) with tubular & reconstruction plates, and 4 (11.7%) with locking and reconstruction plates. In the dual plate group, eight patients (23.5%) were treated with the main plate in the superior position with a smaller aid plate anteriorly (Figs. 1, 2). Twenty-six (82.3%) were treated with an anteriorly based primary working plate and a smaller aid plate superiorly (Figs. 3, 4).
Four clavicles in the dual plate cohort required bone graft due to extensive comminution and bone loss compared to one in the single plating group (p = 0.012).
Fixation outcomes
One hundred and fourteen of one hundred and twenty-five patients (91.1%) treated with single plating achieved radiographic union within 6 months (Table 2). Five patients (4.0%) had pain without bridging callus on plain radiographs at 6 months, but went on to union by 1 year without intervention. Six patients (4.8%) had persistent radiographic non-union at 1 year. Of the six non-unions, two were treated for postoperative deep infection; three developed implant failure; one had a stable implant with radiographic non-union. In the dual plating group, all the 34 patients obtained bony union within 6 months. When comparing groups at 3 months, radiographic union was present in 52.8% of single plates and 35.2% in the dual plating group (p = 0.02). However, at 6 months, no significance difference existed (91.1 vs 100%, p = 0.13). Twenty-two clavicles (15.0%) in single plating group and seven (17.1%) in dual plating group were lost to follow-up prior to 1 year. Therefore, 125 patients in the single plating group and 34 in the dual plating group were followed for an average of 0.8 years (range 0.3–2.6 years) and assessed clinically.
To control for the differences in AO-OTA classification, fixation groups were re-evaluated specifically for AO-OTA B and AO-OTA C fractures. No differences found in union (p = 0.42, 0.22), delayed union (p = 0.83, 0.22), and non-union (p = 0.826, 1.000) rates between single and dual plate fixation. In addition, union rate within 3 and 6 months demonstrated no significant difference for AO/OTA B-type (p = 0.27, 0.42) and AO/OTA C-type (p = 0.92, 0.22).
Twenty-four complications occurred in twenty-two patients treated with single plate fixation. The most common complications were peri-incisional numbness (8) and implant prominence (8). Six patients experienced implant failure—each of which was an anteriorly based 2.7 mm pelvic recon plate. These included broken plates (2), implant loosening (2), and broken screws (2). Two patients developed deep infection. Seven clavicles in the single plating group required reoperation. Four patients required revision surgery following implant failure at a mean of 9.8 months after the initial fixation. Other causes for reoperation in the single plate group included infection (2) and non-union (1). Ten patients elected to undergo plate removal. Seven of these were superior based plates. One patient with an anterior plate that was removed 8 months after the initial fixation refractured 1 month after plate removal following a fall from standing height. This patient required revision ORIF and achieved bony union 6 months after reoperation.
No clavicles in the dual plating group required reoperation (p = 0.30). There were no implant failures in the dual plating group (p = 0.61). Implant prominence was observed in two patients with superiorly based working plates but did not require reoperation. One patient noted peri-incisional numbness. There was no significant difference in the rate of complications between groups (p = 0.8).
Discussion
Extraperiosteal dual plating for acute mid-shaft clavicle fractures can be safely considered for the treatment of complex acute mid-shaft clavicle fractures without increasing the risk of non-union or reoperation. The increased soft-tissue exposure for the addition of the second plate did not require any stripping of the periosteum in an attempt to retain native blood supply. Union rates of 91.1% in the single plate and 100% in the dual plate groups compare favorably to the current literature for operatively treated acute mid-shaft clavicle fractures, where union rates of 98.5% have been reported [4]. Union was significantly greater at 3 months in the single plate group as compared to the dual plate group (52.8 vs 35.2%), but no difference remained at 6 months (91.1 vs 100%). When analyzing fractures by AO-OTA classification, there was no difference in time to union between subgroups treated with single versus dual plate fixation.
The addition of a superior plate theoretically increases the risk of plate prominence and reoperation [11]. In an effort to decrease the need for reoperation due to implant prominence, some surgeons place the plate anteroinferiorly on the clavicle [12]. In our study, the dual plating technique did not demonstrate an increased incidence of plate prominence compared to the single plating group (5.3 vs 6.4%). With the concern of implant prominence, we tended to place the mini aid plate superiorly and the large neutralization plate anteriorly. Ten patients (8.0%) in the single plate group required plate removal, which is similar to the rate reported by Robsinson, et al., (11.6%) [13]. No patient in the dual plating group required implant removal; however, 2 (6%) did express subjective prominence. Six patients in the single plate cohort experienced implant failure of their anterorinferiorly based 2.7 mm recon plates. This failure may have been due to the use of a 2.7 mm recon plate which prior biomechanical evaluations have demonstrated recon plates to have significantly lower stiffness values in regards to axial compression and external rotation compared to superiorly based locking compression plates [16]. Although Jones and colleagues demonstrated excellent clinical results for patients treated with anteroinferiorly based 2.7 mm plate fixation [12].
Multiple limitations exist in our study, mainly due to its retrospective nature which limited the amount of data collected. This study was performed at a single institution; however, no standardized surgical approach or implants were utilized. The sample size of the dual plate group also remains relatively small, limiting the power of our study. Obvious selection bias exists, since surgeons were allowed to choose their fixation construct as deemed necessary for each individual fracture pattern. However, the dual plate fixation group represents a subset of patients who demonstrated more complex and challenging fractures intra-operatively. In some cases, these patients were even allowed to weight bear through their operative extremity due to the need to mobilize in the setting of polytrauma. Despite the increased fracture complexity, dual plating still compared favorably to single plate fixation in regard to non-union and reoperation [14, 15]. As mentioned prior, there was no standardization of implants, but the previous studies have demonstrated both reconstruction and locking plates achieve acceptable bony union and clinical outcomes [16, 17]. Due to the length of the study period, the authors decided not to assess functional outcomes scores, as controlling for time from surgery would have been difficult.
Dual plate fixation, although requiring some-increased soft-tissue exposure but remaining entirely extraperiosteal, offers improved construct stability which may be beneficial in more complex fracture patterns. Despite increased soft-tissue exposure, the addition of a second plate did not increase the risk of non-union or reoperation when compared to single plate fixation. Surgeons may consider utilizing a dual plate construct when necessary without compromising healing or increasing complication rates in the setting of acute displaced mid-shaft clavicle fractures.
References
Robinson CM (1998) Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 80(3):476–484.
Postacchini F, Gumina S, De Santis P, Albo F (2002) Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 11(5):452–456.
McKee RC, Whelan DB, Schemitsch EH, McKee MD (2012) Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am 18;94(8):675–684.
Hill JM, McGuire MH, Crosby LA (1997) Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 79(4):537–539
Scolaro JA, Hsu JE, Svach DJ, Mehta S (2014) Plate selection for fixation of extra-articular distal humerus fractures: a biomechanical comparison of three different implants. Injury 45(12):2040–2044
Kosmopoulos V, Nana AD (2014) Dual plating of humeral shaft fractures: orthogonal plates biomechanically outperform side-by-side plates. Clin Orthop Relat Res 472(4):1310–1317
Prasarn ML, Meyers KN, Wilkin G, Wellman DS, Chan DB, Ahn J, Lorich DG, Helfet DL (2015) Dual mini-fragment plating for midshaft clavicle fractures: clinical and biomechanical investigation. Arch Orthop Trauma Surg 135(12):1655–1662
Sadiq S, Waseem M, Peravalli B, Doyle J, Dunningham T, Muddu BN (2001) Single or double plating for nonunion of the clavicle. Acta Orthop Belg 67(4):354–360
El Haj M, Khoury A, Mosheiff R, Liebergall M, Weil YA (2013) Orthogonal double plate fixation for long bone fracture nonunion. Acta Chir Orthop Traumatol Cech 80(2):131–137
Shannon SF, Chen X, Torchia M, Schoch B (2016) Extraperiosteal dual plate fixation of acute mid-shaft clavicle fractures: a technical trick. J Orthop Trauma 30(10):e346–e350. doi:10.1097/BOT.0000000000000633
Formaini N, Taylor BC, Backes J, Bramwell TJ (2013) Superior versus anteroinferior plating of clavicle fractures. Orthopedics 36(7):e898–e904. doi:10.3928/01477447-20130624-20
Jones CB, Sietsema DL, Ringler JR, Endres TJ, Hoffmann MF (2013) Results of anterior-inferior 2.7 mm dynamic compression plate fixation of midshaft clavicular fractures. J Orthop Trauma 27(3):126–129
Robinson CM, Goudie EB, Murray IR, Jenkins PJ, Ahktar MA, Read EO, Foster CJ, Clark K, Brooksbank AJ, Arthur A, Crowther MA, Packham I, Chesser TJ (2013) Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am 95(17):1576–1584.
Oh W, Jeon IH, Kyung S, Park C, Kim T, Ihn C et al (2002) The treatment of double disruption of the superior shoulder suspensory complex. Int Orthop 26(3):145–149 (Epub 2002 Feb 14).
Chakravarthy M, Kabber S, Kumar D, Mattur K, Reddy K, Kumar S et al (2009) Fixation of the fracture clavicle for early restoration of the patient to preinjury status. J Trauma 67(1):216
Eden L, Doht S, Frey SP, Ziegler D, Stoyhe J, Fehske K et al (2012) Biomechanical comparison of the locking compression superior anterior clavicle plate with seven and ten hole reconstruction plates in midshaft clavicle fracture stabilisation. Int Orthop 36(12):2537–2543
Cho CH, Song KS, Min BW, Bae KC, Lee KJ et al (2010) Operative treatment of clavicle midshaft fractures: comparison between reconstruction plate and reconstruction locking compression plate. Clin Orthop Surg 2(3):154–159. doi:10.4055/cios.2010.2.3.154 (Epub 2010 Aug 3)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does contain human participants operated on by one of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study prior to surgery.
Rights and permissions
About this article
Cite this article
Chen, X., Shannon, S.F., Torchia, M. et al. Radiographic outcomes of single versus dual plate fixation of acute mid-shaft clavicle fractures. Arch Orthop Trauma Surg 137, 749–754 (2017). https://doi.org/10.1007/s00402-017-2676-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2676-0