Abstract
Introduction
Chronic exertional compartment syndrome (CECS) is a common injury in young athletes, causing pain in the involved leg compartment during strenuous exercise. The gold standard treatment is fasciotomy, but most of the reports on its effectiveness include relatively small cohorts and relatively short follow-up periods. This study reports the long-term results of a large cohort of young athletes who underwent single-incision fasciotomy for CECS.
Materials and methods
This a retrospective case-series study. All patients treated by fasciotomies performed for CECS between 2007 and 2011, in a tertiary medical institution. CECS was diagnosed following history taking and clinical evaluation, and confirmed by compartment pressure measurements. Ninety-five legs that underwent single-incision subcutaneous fasciotomy were included. Data on the numerical analog scale (NAS), Tegner activity score, and quality-of-life (QOL) as measured via the short form-12 (SF-12) were retrieved from all patients preoperatively and at the end of follow-up.
Results
The average time to diagnosis was 22 months and the mean follow-up was 50.1 months. Sixty-three legs underwent anterior compartment fasciotomy (an additional 30 legs also underwent lateral compartment release), and two legs underwent lateral and peroneal compartment releases. The average change in Tegner score was an improvement of 14.6 points. Similarly, the patients reported a significant improvement in the SF-12 and NAS scores. Satisfaction rates were high (average 75.5 %). The main complications were wound infection (2 patients) and nerve injuries (4 patients). Eight patients had recurrence.
Conclusion
Single-incision fasciotomy leads to long-term improvement in the activity level and QOL of patients with CECS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic exertional compartment syndrome (CECS) is a common injury among young adult athletes involved in endurance running, team sports (such as soccer, field hockey, and lacrosse [1]), as well as among military recruits. It is a recurrent, reversible ischemic condition related to a marked increase in intramuscular pressure within a specific compartment during exertion secondary to a fibro-osseous space that is non-compliant with volume expansion [2–4]. Risk factors include anabolic steroid and creatine use which increases muscle volume and eccentric exercise [5, 6]. The diagnosis of CECS is based on clinical history and characterized by pain during strenuous activity that is usually well localized for a specific compartment and that disappears quickly after rest [7, 8]. The diagnosis is confirmed by increased intramuscular pressure in the involved compartment [7, 8].
Although the condition is well established, there is usually a delay in diagnosis of up to 22 months [4] due to low levels of awareness among clinicians and a wide range of differential diagnosis for chronic exertional leg pain, which includes medial tibial stress syndrome, stress fracture, fascial defects, nerve entrapment syndromes, popliteal artery entrapment syndrome, and claudication [9, 10]. Although some patients initially attempt conservative treatment, such as activity modification, stretching, and physiotherapy [6], the only definitive treatment for CECS is fasciotomy, and it is the treatment of choice for young and active individuals. The diverse surgical decompression techniques in current use include open fasciotomies, minimally invasive subcutaneous fasciotomies through one or two incisions, partial fasciotomies, and endoscopic-assisted fasciotomy [11].
Fasciotomies for the anterior and lateral compartments of the leg, which present in up to 95 % of cases of CECS [12, 13], have the best outcome, with a success rate of around 80 % [5, 14]. The reported complications after surgical compartment release are hemorrhage, keloids, local pain, hematoma, deep vein thrombosis, wound infection, nerve injury, and vascular injury [5, 7, 11]. The incidence of complications ranges from 4.5 to 13 %, and the recurrence rate of symptoms ranges between 6 and 19 % of surgical cases [7, 15, 16]. A recent systemic review described that 84 % of patients are satisfied with their surgical outcomes at short- to mid-term follow-up [16]. The gold standard treatment is fasciotomy, but most of the reports on its effectiveness over time include relatively small cohorts and relatively short follow-up periods. The purpose of this study is to report the results and complications of a single minimal incision fasciotomy on a large cohort with a long follow-up.
Methods
Study population
Between 2007 and 2011, 54 patients (95 legs) diagnosed as having CECS who underwent single minimal incision subcutaneous fasciotomy and were available to respond to questionnaires at the time of study that were included in this study. There were no exclusion criteria.
Approval from the local institutional review board was obtained for this study and informed consent was waived.
Diagnosis of CECS
CECS was diagnosed according to a positive history for exercise-induced leg pain or paresthesia, which was relieved with rest, and the results of a clinical assessment of the affected leg(s). The diagnosis was confirmed by compartment pressure measurements before and after exercise by a sports physician using the Stryker® (Stryker Surgical, Kalamazoo, MI, USA) pressure monitoring system as described previously [9]. Due to the unpleasant nature of this test and the frequent occurrence of CECS in anterior and lateral compartments, only the anterior compartment pressure was measured in each involved leg, unless the pain arose directly from the posterior compartment. Patients who presented with symptoms in both legs underwent bilateral measurements.
All measurements were standardized for the knee and ankle joint position, and taken while the patient was supine, to avoid unwanted effects on the intra-compartmental pressures. After baseline pressure measurement, the patients performed the culpable exercise (e.g., by running on a treadmill with 2°–3° of elevation) until the onset of severe symptoms. They then rested for 5 min and compartment pressures were measured. The diagnosis of CECS was made according to the Pedowitz criteria [8] as follows: a resting pressure of ≥15 mmHg and/or a pressure of ≥30 mmHg at 1 min post-exercise in any compartment.
Data acquisition
This study is a retrospective review of clinical and operative notes of patients treated for CECS with single-incision subcutaneous fasciotomy. At the time of the study, all available participants were contacted and a telephone questionnaire was used to obtain data on self-reported complications, recurrence of symptoms, current activity level, and the level of satisfaction. The Tegner activity score was used to evaluate the level of activity before and after the surgery [17, 18] at the latest follow-up in the clinic, and quality-of-life was measured via the short form-12 (SF-12), a questionnaire with 12 health survey questions which combined the scoring results in two scales of mental and physical functioning [19, 20]. A numerical analog score (NAS) was used to measure pain, with 0 = no pain and 10 = worst pain imaginable [21].
Operative technique
All the procedures were performed in an ambulatory setting. Patients were under general anesthesia. Each limb was operated upon individually and without the use of a tourniquet. The anterior and lateral compartment fascias were released through 4-cm long incisions. The incision was located between the middle and the distal third of the leg, and placed at 3–4-cm lateral to the anterior tibia crest within 2 cm from the anterior intramuscular septum that divides the anterior and lateral compartments (Fig. 1), thereby allowing easy access to both compartments. Blunt dissection and exposure of the fascia were then carried out (Fig. 2). The fascia of the anterior and lateral compartments was dissected using laparotomy scissors (Fig. 3a–c), after which an Esmark Rubber Bandage was applied over the leg for 7–10 min for bleeding control. The wound was irrigated and closed, and a compressive Jones bandage dressing was applied.
Patients were allowed full weight-bearing immediately following the operation, and there, for prophylactic anticoagulation, was not administered. Crutches were recommended for the first 2–3 postoperative days for comfort and support. Local massage was recommended as well. Return to running was allowed after 1 month.
Statistical analysis
Analyses were performed on demographic data and outcomes. Categorical data were compared using Fisher’s exact test. Continuous data were analyzed using Student’s t test. A P value <0.05 was considered to be significant.
Results
A total of 95 single minimal incision fasciotomies for the treatment of CECS were performed in our institution between 2007 and 2011. The study population consisted of 49 men and 4 women with an average age of 23.6 years (range 16–43 years). The time to establish the diagnosis since symptom onset ranged between 2 weeks and 10 years, with a mean of 22.2 months. This study analyzed the treatment of these 53 patients, of whom 42 (88.4 %) underwent bilateral compartment release. Table 1 shows the patients’ demographics.
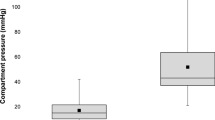
There was a significant difference (P < 0.001) in intra-compartment pressures between pre-exercise and post-exercise measurements (24.9 ± 10.8 and 61 ± 29.3 mmHg, respectively). Figure 4 presents pressure measurements for each side separately.
Preoperative pressure measurements. Pressure was measured with the Stryker pressure monitoring system. After baseline pressure measurement, the patients performed the culpable exercise (e.g., by running on a treadmill with 2°–3° elevation) until the onset of severe symptoms. They then rested for 5 min and compartment pressures were taken
A total of 63 legs (66.3 %) underwent anterior compartment fasciotomy, 30 legs also underwent lateral compartment release, and 2 legs underwent lateral and peroneal compartment releases. The postoperative follow-up for the entire group ranged from 4.6 to 97.5 months, with an average follow-up period of 50.1 months.
The Tegner activity score was calculated before and after the operation. The average preoperative Tegner score was 79 (SE 1.18, median 80), and the average postoperative Tegner score was 93.6 (SE 1.35, median 100), yielding an average change of 14.6 (SE 1.52, median 14). Similarly, patients reported a significant improvement in SF12 scores (both the physical and mental summary scores) after the surgery, as well as in pain reduction [as expressed by a NAS (Fig. 5)]. The results indicated that 75.5 % (40/53) were satisfied from the surgery and would have chosen to undergo it again in retrospect. No correlation was found between the degree of satisfaction from the surgery and the level of activity (P = 0.332), with the type of activity (P = 0.630) or with the patients’ age groups [high school student (age 16–18), an army soldier (age 18–21), or older than 21 years old] (P = 0.399).
Quality-of-life, pain assessment, and functioning questionnaires. Patients were asked to answer the Tegner, SF-12, and NAS questionnaires before the operation and at the last follow-up. The improvement in each parameter was significant. PCS and MCS refer to the physical and mental aspects of the SF-12 assessment questionnaire respectfully. NAS (numerical analog scale) was used to asses pain levels
Analysis of the surgical complications showed that 4.2 % (4/95) of the legs had nerve injuries: two of the affected patients reported altered sensation over the surgical scar, while the other two displayed decreased sensation at the superficial peroneal nerve distribution. One of the latter underwent surgical release of the nerve entrapped in the surgical scar 1 year after the compartment pressure release procedure. CECS symptoms recurred in 8.4 % legs (8/95). The surgery-related complications reported for the 95 operated legs are detailed in Fig. 6.
Discussion
The majority of patients with CECS of the leg that had been treated with single minimal incision fasciotomy reported satisfactory outcome rates (75.5 %) associated with the improvement in the level of activity and reduction in the level of pain compared with pre-fasciotomy scores. This study results are in line with those of the previous reports of favorable long-term outcome for anterolateral compartment release, i.e., 60–100 % [22–25]. The single minimal incision method has an esthetic advantage by reducing the number of scars.
In the current cohort, bilateral pain was reported by 88.4 % of the patients (42/53 patients) who were eventually operated upon both legs. Other publications reported bilateral pain in 70–82 % of the cases [6, 9, 13, 22, 26, 27]. The diagnosis of CECS was based on clinical signs and confirmed by compartment pressure testing after exercise [6, 9]. The current group did not include patients with posterior compartment syndrome, which is reported to achieve less favorable outcomes [10].
There was no significant difference in satisfaction from surgery among patients with preoperative Tegner scores which were below or above the median value (median 80, P = 1.0). This suggests that patients benefit from the operation regardless of the levels of functional limitation following it. In addition, unlike Parker et al. [28], we did not find any correlation between the occupation of the patients and their satisfaction levels from the surgery. Furthermore, while other studies [6, 29] found that soldiers exhibit lower levels of satisfaction following fasciotomy, this was not the case among the military recruits in our cohort, of whom 43.4 % (23/53) were in the army at the time of operation.
As reported in the previous studies [6, 9, 10], fasciotomy for the treatment of CECS can be associated with various complications. Recurrence of symptoms may occur as a result of inadequate release, failure to decompress a symptomatic compartment, postsurgical fibrosis, or nerve compression [6]. Eight of our patients (8.4 % of the legs) experienced symptom recurrence, and three of them are among the unsatisfied patients. These results are similar to other reports of recurrence rates up to 17 % [6]. Nerve injuries occurred in four (4.2 %) legs, similar to the findings of Finesone et al. who reported that 4.5 % (3/67) of their patients suffered from injury to the superficial peroneal nerve [27]. The deficit in sensation in one of our three dissatisfied patients who suffered nerve injury developed within weeks after the fasciotomy as a result of pressure from the scarred tissue that flattened the nerve. The fourth patient who presented with sensation deficit in the superficial peroneal nerve distribution soon after the fasciotomy was nevertheless highly satisfied: this patient was not operated again, and it is reasonable to assume that iatrogenic damage to the nerve had occurred at its exit from the fascia during the fasciotomy. Finally, two of our patients had wound infection which was treated uneventfully with antibiotics. A comparison of our results to those of others is presented in Table 2. It is important to note that while the preliminary results of fasciotomy using an endoscopic approach seem promising [11, 30–32], large prospective studies have yet to be performed.
The limitations of this study include its retrospective design and the absence of a control group.
To conclude, this report describes the treatment of CECS in a large cohort (54 patients, 95 legs) with a relatively long-term follow-up (mean 50.1 months). We found the single minimal incision fasciotomy to be a successful and reliable treatment for patients diagnosed as having CECS, with relatively high rates of surgical success and patient satisfaction and acceptable complication rates.
References
Davis DE, Raikin S, Garras DN, Vitanzo P, Labrador H, Espandar R (2013) Characteristics of patients with chronic exertional compartment syndrome. Foot Ankle Int 34:1349–1354
Wilder RP, Magrum E (2010) Exertional compartment syndrome. Clin Sports Med 29:429–435
Canale S (1998) Campbell’s operative orthopaedics. Elsevier, Philadelphia
Frontera W (2002) Essentials of physical medicine and rehabilitation. Hanley and Belfus, Canada
Brennan FH Jr, Kane SF (2003) Diagnosis, treatment options, and rehabilitation of chronic lower leg exertional compartment syndrome. Curr Sports Med Rep 2:247–250
Dunn JC, Waterman BR (2014) Chronic exertional compartment syndrome of the leg in the military. Clin Sports Med 33:693–705
Fraipont MJ, Adamson GJ (2003) Chronic exertional compartment syndrome. J Am Acad Orthop Surg 11:268–276
Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH (1990) Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 18:35–40
Tucker AK (2010) Chronic exertional compartment syndrome of the leg. Curr Rev Musculoskelet Med 3:32–37
Rom E, Tenenbaum S, Chechick O, Burstein G, Amit Y, Thein R (2013) Chronic exertional compartment syndrome. Harefuah 152:608–611
Wittstein J, Moorman CT 3rd, Levin LS (2010) Endoscopic compartment release for chronic exertional compartment syndrome: surgical technique and results. Am J Sports Med 38:1661–1666
Verleisdonk EJ, Schmitz RF, van der Werken C (2004) Long-term results of fasciotomy of the anterior compartment in patients with exercise-induced pain in the lower leg. Int J Sports Med 25:224–229
Cook S, Bruce G (2002) Fasciotomy for chronic compartment syndrome in the lower limb. ANZ J Surg 72:720–723
DeLee JC et al (2003) DeLee and Drez’s orthopaedic sports medicine. Saunders, Philadelphia
Slimmon D, Bennell K, Brukner P, Crossley K, Bell SN (2002) Long-term outcome of fasciotomy with partial fasciectomy for chronic exertional compartment syndrome of the lower leg. Am J Sports Med 30:581–588
Campano D, Robaina JA, Kusnezov N, Dunn JC, Waterman BR (2016) Surgical management for chronic exertional compartment syndrome of the leg: a systematic review of the literature. Arthroscopy 32(7):1478–1486
Lysholm J, Tegner Y (2007) Knee injury rating scales. Acta Orthop 78:445–453
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Ware J Jr, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Amir M, Lewin-Epstein N, Becker G, Buskila D (2002) Psychometric properties of the SF-12 (Hebrew version) in a primary care population in Israel. Med Care 40:918–928
McCaffery M, Beebe A et al (1989) Pain: clinical manual for nursing practice. Mosby, St. Louis
Detmer DE, Sharpe K, Sufit RL, Girdley FM (1985) Chronic compartment syndrome: diagnosis, management, and outcomes. Am J Sports Med 13:162–170
Howard JL, Mohtadi NG, Wiley JP (2000) Evaluation of outcomes in patients following surgical treatment of chronic exertional compartment syndrome in the leg. Clin J Sport Med 10:176–184
Rorabeck CH, Bourne RB, Fowler PJ (1983) The surgical treatment of exertional compartment syndrome in athletes. J Bone Jt Surg Am 65:1245–1251
Schepsis AA, Martini D, Corbett M (1993) Surgical management of exertional compartment syndrome of the lower leg. Long-term followup. Am J Sports Med 21:811–817 (discussion 817)
Raikin SM, Rapuri VR, Vitanzo P (2005) Bilateral simultaneous fasciotomy for chronic exertional compartment syndrome. Foot Ankle Int 26:1007–1011
Finestone AS, Noff M, Nassar Y, Moshe S, Agar G, Tamir E (2014) Management of chronic exertional compartment syndrome and fascial hernias in the anterior lower leg with the forefoot rise test and limited fasciotomy. Foot Ankle Int 35:285–292
Packer JD, Day MS, Nguyen JT, Hobart SJ, Hannafin JA, Metzl JD (2013) Functional outcomes and patient satisfaction after fasciotomy for chronic exertional compartment syndrome. Am J Sports Med 41:430–436
McCallum JR, Cook JB, Hines AC, Shaha JS, Jex JW, Orchowski JR (2014) Return to duty after elective fasciotomy for chronic exertional compartment syndrome. Foot Ankle Int 35:871–875
Bramante C, Gandolfo L, Bosco V (2008) Minimally invasive fasciotomy in the treatment of chronic exertional anterior compartment syndrome of the leg: personal technique. Chir Ital 60:711–715
Sebik A, Dogan A (2008) A technique for arthroscopic fasciotomy for the chronic exertional tibialis anterior compartment syndrome. Knee Surg Sports Traumatol Arthrosc 16:531–534
Lohrer H, Nauck T (2007) Endoscopically assisted release for exertional compartment syndromes of the lower leg. Arch Orthop Trauma Surg 127:827–834
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
M. Drexler and T. F. Rutenberg contributed equally to this work.
Rights and permissions
About this article
Cite this article
Drexler, M., Rutenberg, T.F., Rozen, N. et al. Single minimal incision fasciotomy for the treatment of chronic exertional compartment syndrome: outcomes and complications. Arch Orthop Trauma Surg 137, 73–79 (2017). https://doi.org/10.1007/s00402-016-2569-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2569-7