Abstract
Objectives
It is unclear whether all completely displaced midshaft clavicle fractures require primary surgical intervention. The aim of this study was to elucidate the radiological and clinical outcomes after conservative treatment, and to identify subgroups at risk of an inferior outcome.
Design
Retrospective case series.
Setting
Level II trauma center.
Patients
Between 2005 and 2008, 122 patients were conservatively treated for a completely displaced midshaft clavicle fracture of whom 92 were eligible for inclusion in this study. Of these, 59 completed the study after a median of 2.7 years after the fracture (min–max, 1.1–4.9).
Intervention
The patients received the standard treatment administered at our institution at the time: nonsurgically with a sling without physiotherapy. Patients with painful nonunions were subsequently offered surgery.
Main outcome measurements
At follow-up, the patients’ Disabilities of Arm, Shoulder, and Hand (DASH) and the Constant scores were evaluated. Radiographs were taken at follow-up and compared to those taken acutely.
Results
Nonunion was found in 9 of the 59 (15.3 %) patients. Twenty-four (24 %) patients reported a fair-to-poor DASH score (i.e. >20). Patients with fractures that were vertically displaced by more than 100 % (one bone width) were significantly less satisfied than those with fractures vertically displaced at 100 % (p = 0.04). Initial shortening of more than 15 mm was not associated with a worse outcome or nonunion. The odds ratio of developing a nonunion increased with age (p = 0.04).
Conclusions
By treating completely displaced midshaft clavicle fractures conservatively with a sling and offering plate fixation for eventual painful nonunions, we found a 24 % risk of a fair or poor clinical result with a DASH score over 20. A vertical displacement of more than 100 % between the main fragments on the initial radiograph was associated with an inferior clinical outcome in this study.
Level of evidence
IV.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Clavicle fractures are common, reportedly accounting for 2.6–4 % of all fractures, with midshaft fractures constituting approximately 80 % of all clavicle fractures [1, 2]. Midshaft clavicle fractures are traditionally thought to have a good prognosis, and most are treated nonsurgically with a sling or a figure-of-eight bandage. Studies by Neer and Rowe in the 1960s demonstrated very low nonunion rates of 0.1–0.7 % [3, 4]. More recent studies have distinguished between adults and children, the latter of whom have an inherently good prognosis [5], and found a higher incidence of symptomatic malunion and nonunion after conservatively treated displaced fractures than was previously reported for adults [6–12]. In adults, 4–7 % of diaphyseal fractures result in nonunion, and this increases to 15–20 % for completely displaced fractures [13, 14]. Several studies have revealed a somewhat better clinical outcome of surgically managed displaced midshaft clavicle fractures than sling treatment. Although the differences are statistically significant, their clinical significance is uncertain [15–21]. The number of patients needed to treat to avoid a painful mal- or nonunion has been reported to be 3.3–4.6 [22, 23]. The subgroups of completely displaced midshaft clavicle fractures to whom primary osteosynthesis should be offered to avoid these complications have yet to be identified, although displacement, shortening, gender, and age have been suggested as risk factors for a worse outcome [13].
The aim of this study was to determine the radiological and clinical outcomes in a series of completely displaced midshaft clavicle fractures treated with a sling, with a follow-up period of 1–4 years. We sought to identify patient and fracture characteristics that would provide prognostic information for the orthopaedic surgeon when considering the right primary treatment for individual patients.
Patients and methods
Patients and study design
At the time of inclusion, Akershus University Hospital served a population of about 320,000 inhabitants. From the hospital information system, 145 cases of midshaft clavicle fractures displaced one bone width or more were identified between January 1, 2005 and December 31, 2008 in patients aged 16–60 years who were treated at our institution. At the time of the study, the department’s main treatment method was conservative with a sling for 2 weeks, after which the patients were encouraged to perform increasing pendulum exercises below 90° of abduction for the first 6 weeks. Physiotherapy was not routinely administered. Patients who had undergone primary plate fixation, were unable to fill out forms, had an open fracture, neurovascular injury, other shoulder injury or a concomitant medical condition that would compromise the calculation of shoulder scores was excluded from the study. Patients not living within the hospital’s catchment area were also excluded from the study, as follow-up information was not available in our medical files.
In 2010, 92 eligible patients received a written invitation, of which 59 (64 %) attended an ambulatory follow-up visit at the hospital with one of the investigating orthopaedic surgeons. Radiological and physical examinations were performed and clinical outcomes were assessed using standardized questionnaires. We also reviewed the medical records to obtain information about the injury mechanism, presence of surgical treatment for nonunion and assessment of initial radiographs.
The study was approved by the South East Regional Ethics Committee of for Medical and Health Research Ethics of Norway (Ref. s-09378c2009/7999).
Radiological assessment
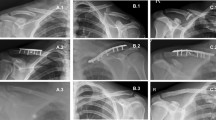
All patients were submitted to radiography at the time of injury to produce standing 15° cranial and 15° caudal views (initial radiographs). Anteroposterior panoramic radiographs of both clavicles were obtained at the follow-up to evaluate shortening by comparing the length of the injured clavicle with that on the contralateral uninjured side [24]. Both the primary and follow-up radiographs were examined for shortening, measured in millimetres. Because panoramic radiographs were not obtained at the time of injury, the initial degree of shortening was estimated by measuring the shortening between the overlapping bone ends on the initial radiographs [10, 25] (Fig. 1). The vertical displacement in the cranio-caudal direction was measured in per cent, where one bone width displacement was set as 100 %. We divided the group into patients with cortical contact of the main fragments (100 % vertical displacement) and without bony contact (>100 % vertical displacement). Nonunion was defined as no bridging callus formation 6 months after injury.
Radiographs of a displaced midshaft clavicle fracture in a single patient with outlines of the measurements. a Initial frontal 15° cranial view. Arrow the measured shortening. b Frontal 15° caudal view. Arrow estimated vertical displacement of 200 % in this case. c Panoramic view of both claviculae after healing. Arrows the measured shortening (i.e. length of the normal clavicle minus length of the fractured clavicle). a and b were taken at the time of injury, c at follow-up
Assessment of clinical outcomes
The clinical outcome was assessed with the Disability of Arm, Shoulder and Hand (DASH) questionnaire [26] and the modified Constant Shoulder (CS) score [27, 28]. DASH and CS scores were considered as the primary outcome variables.
The DASH questionnaire is a patient-oriented score, validated in Norwegian [29], and is scored from 0 (perfect extremity) to 100 (completely disabled limb). The minimal clinically important difference for the shoulder has been determined to be 10.2 for the DASH score [30]. Since patients with previous shoulder injury or concomitant injuries that would compromise shoulder function were excluded from this study, a score of ≤10 was considered excellent, while a score of 10–20 was considered good, 20–30 as fair, and >30 as poor [5].
The CS is scored by the physician and takes into account pain, activities of daily living, range of movement and power abduction strength. Pain is scored as an average score on a visual analogue scale (VAS) ranging from 0 (no pain) to 15 (maximum possible pain), and graded as no, mild, moderate, or severe pain. Isometric power was measured using a Berkley TDS35 scale in the scapular plane with 90° of shoulder abduction and a constant pull over 5 s. The average of five repetitions was calculated. A perfect shoulder would achieve a score of 100 points, and a lower score indicates a higher level of disability.
VAS scales were used to measure secondary outcome variables. The 15-point VAS scale for pain in the CS was used as a separate evaluation with the score converted to 0–10 by simply dividing the score by 1.5, because we felt that introducing a second pain scale would be confusing for the patients. The patients were asked if they were satisfied with their overall shoulder function after their clavicle fracture, and marked their result on a 10 cm VAS scale divided into from 0 to 10 points, where 10 indicated complete satisfaction. They were also asked to mark their satisfaction of the cosmetic result after fracture on an identical VAS scale.
Statistical analysis
The normality of the DASH, CS, and the three VAS scores was assessed graphically and with the Shapiro–Wilk test, indicating that the VAS scales for pain and patient satisfaction and the CS and DASH scores had non-normal distributions. Therefore, descriptive statistics are presented for all of these variables using the median and the range between 25th and 75th percentiles. Parametric tests were used for vertical displacement and shortening and Chi square for analysis of categorical data. Parameters with non-normal distributions were log transformed in multivariate logistic and linear regression analysis.
Statistical analysis was performed using Stata 12.1 (StataCorp, College Station, TX, USA). The cutoff for statistical significance was set at p < 0.05 using two-sided tests.
Results
We identified 145 patients with completely displaced midshaft clavicle fractures, of whom 122 patients were conservatively treated with a sling for 1–2 weeks. The remaining 23 patients were elected to open reduction and plate fixation by the surgeon on call because of skin compromise in five patients or displacement (Table 1; Fig. 2). Thirty patients did not meet the inclusion criteria and were excluded from the study.
Of 92 remaining eligible patients, 33 did not respond to the written invitation and thus were lost to follow-up or chose not to participate. The 59 participants had a higher proportion of motor vehicle injuries and a lower proportion of sport injuries than non-participants; otherwise, the demographics and fracture characteristics were not statistically significantly different (Table 1). Five patients (15.2 %) were diagnosed with a nonunion and operated with plate fixation and bone grafting. The median time from injury to follow-up was 2.7 years (min–max, 1.1–4.9).
Radiological outcomes
The median initial shortening was 15 mm (25th–75th percentiles, 12–20 mm) in the entire cohort (n = 59) and 15 mm (7.8–18.3 mm) in the 50 fractures that progressed to primary union. In the fractures that healed, the median difference in length measurement between the initial and final radiographs was 7.5 (4–10 mm).
A nonunion was found in 9 (15.3 %) of the 59 patients (Table 1). One patient with a painful nonunion was discouraged from surgery due to concomitant medical disorders and an unacceptable risk of complications. Three had minor or no complaints, and were thus not offered surgery. The remaining five had a painful nonunion and no contraindications and so underwent surgery with plate fixation prior to the study. There was no difference in initial shortening when compared to fractures that healed primarily.
Multivariate logistic regression analysis revealed that the odds ratio (OR) for the risk of nonunion more than doubled for every 10 years increase in patient age (p = 0.04). Women had an OR of 5.1 versus men to develop nonunion, but with a wide confidence interval (0.8–32.4).
Clinical outcomes
The median DASH score was 6.7 (0.8–19). The DASH score was good or excellent (i.e. <20) in 76 % of the patients; thus, 24 % had a DASH score of over 20. In bivariate linear regression analysis, female sex was associated with a higher DASH score. There was a tendency toward the DASH score being higher in the nonunion group, than for fractures that healed with conservative treatment (p = 0.06). We did not find significantly worse DASH scores with shortening, vertical displacement, or intermediary fragments on the entire cohort (Table 2). In multivariate analysis, only female sex was associated with a higher DASH score. In the five nonunions treated surgically with plate fixation, three ended up with a DASH score of more than 37 after union, signifying a substantial clinical disability.
The median CS was 81 (69–90) for the entire cohort (n = 59). Females had lower CS scores than males, and those with nonunion had lower scores than those with primary healing (Table 2). In multivariate linear regression analysis, only sex was significantly associated with the lower CS score.
Forty-nine of the 59 experienced residual pain under normal activities, with a median score of 1.3 on a VAS scale from 0 to 10. In bivariate analysis, the reported pain was greater in patients with a nonunion even after successful surgery than in those with fractures with primary healing (Table 2); however, the difference was not statistically significant in multivariate analysis (Table 3).
The median VAS score for satisfaction after the clavicular fracture was 5 (25th–75th percentiles, 4–8.7). Only 10 % (6/59) of patients scored 10 (perfect), while 58 % (34/59) scored 6 or lower. In bivariate analysis, patients were less satisfied when the vertical displacement was more than 100 % (p = 0.04; Table 2), although the difference was not statistically significant after adjustment for age and sex (Table 3).
The median VAS score for the cosmetic result was 5 (3.3–9.0). Only 9 of the 59 patients were completely satisfied with their cosmetic result. The outcome was not significantly worse for vertical displacement over 100 % or shortening of greater than the median value of 15 mm (Table 3).
Discussion
One out of four patients in this study with completely displaced midshaft fractures of the clavicle who were initially treated non-surgically had a fair or poor clinical outcome at a median follow-up of 2.7 years. Nonunion developed in 9 of the 59 patients, of whom 5 underwent surgery but had a reduced clinical outcome even after healing was completed.
Females were more likely to develop a nonunion than were men, in line with other reports [13]. They also had inferior clinical outcome than men, as assessed with the DASH and Constant scores. It is important to note that gender does influence both scoring systems with inferior results in women [31–33]. This might influence the results in our study.
Shortening was not associated with an inferior clinical outcome or with nonunion in either the initial or control radiographs. Several studies have found inferior clinical outcome in the presence of shortening of 1.5–2 cm after healing [9, 10, 14, 34, 35], whereas others have not demonstrated such a relationship [8, 36, 37]. We found that the median initial and final shortening were similar in the group that healed as a whole, but there was a large individual adjustment during the healing process, suggesting that it is not possible to predict final shortening from the initial radiograph. It is important to realize that shortening was measured in different ways in those studies, and that calibrated radiographs were used in very few, raising a question as to the accuracy of measurements.
There was a tendency toward an inferior clinical outcome with vertically displaced fractures greater than 100 %, and these patients were less satisfied with their overall shoulder function. This subgroup can be identified on the acute radiograph due to the presence of clear distance between the main fragments and has been identified in several other studies as an important radiographic marker for pain and inferior clinical outcomes [6, 8, 14, 38]. Vertical displacement has a better intra- and interobserver reliability in radiographs than shortening [25] and may therefore have greater value in predicting the outcome in acute fractures than shortening.
A nonunion developed in 14/92 (15 %) of the eligible patients, which is comparable to the proportions found in recent studies [6, 10, 39]. Female sex and increasing age were found to be associated with a higher probability of developing a nonunion, but there was no association between nonunion and the degree of displacement, initial shortening, or the number of intermediary fragments. Therefore, we were unable to detect any fracture configuration associated with an increased risk of nonunion development. This finding contrast with those of some studies [10, 13, 39, 40], but is supported by a recent randomized controlled trial [17]. Six out of nine nonunions were symptomatic; five of these were suitable for surgery and healed with open reduction and plate fixation. These five had a significantly reduced clinical outcome at follow-up. In contrast to earlier reports, this suggests that osteosynthesis of an established clavicular nonunion may lead to a substantially reduced shoulder function [41, 42]. This finding raises questions as to the treatment protocol used in the present patient series, in which most displaced midshaft clavicular fractures were allocated to initial conservative treatment on the assumption that nonunions could be dealt with when manifest without loss of prognosis. When seen in light of the DASH scores reported in several RCTs [17, 21, 43], this study lends support to primary surgery in fractures displaced with more than 100 %.
This study was subject to some limitations. Although one-third of the patients were not available for follow-up, this group had the same registered percentage of nonunions and similar descriptive characteristics as those patients completing the study. Acute surgery was performed in 23 patients with more vertically displaced fractures. If this group had been treated conservatively with a sling, we might expect worse results in the entire group. This was a retrospective study with a limited number of patients from a single institution, which might limit the external validity of the results and reduce the power of the analyses. This study also had a potential for type II errors due to the smallness of the sample. Several of the given point estimates indicate clinical importance, but the uncertainty was too large to enable conclusions to be drawn. The presence of acute displacement was assessed on standard radiographs; CT scans would have been superior, but were not available. Notwithstanding these limitations, the strength of our study includes the use of validated patient-oriented outcomes in addition to clinical and radiographic evaluation.
Conclusion
By treating completely displaced midshaft clavicle fractures conservatively with a sling and offering plate fixation for eventual painful nonunions, we found a 24 % risk of a fair or poor functional result with a DASH score over 20. A vertical displacement of more than 100 % between the main fragments on the initial radiograph was associated with an inferior clinical outcome in this study.
References
Nordqvist A, Petersson C (1994) The incidence of fractures of the clavicle. Clin Orthop Relat Res 300:127–132
Postacchini F, Gumina S, De Santis P, Albo F (2002) Epidemiology of clavicle fractures. J Shoulder Elbow Surg 11(5):452–456 pii:S1058274602000678
Neer CS 2nd (1960) Nonunion of the clavicle. J Am Med Assoc 172:1006–1011
Rowe CR (1968) An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res 58:29–42
Randsborg PH, Fuglesang HF, Rotterud JH, Hammer OL, Sivertsen EA (2013) Long-term patient-reported outcome after fractures of the clavicle in patients aged 10 to 18 years. J Pediatr Orthop. doi:10.1097/BPO.0000000000000082
Nowak J, Holgersson M, Larsson S (2005) Sequelae from clavicular fractures are common: a prospective study of 222 patients. Acta Orthop 76(4):496–502. doi:10.1080/17453670510041475
Nowak J, Stalberg E, Larsson S (2002) Good reduction of paresthesia and pain after excision of excessive callus formation in patients with malunited clavicular fractures. Scand J Surg 91(4):369–373
Nowak J, Holgersson M, Larsson S (2004) Can we predict long-term sequelae after fractures of the clavicle based on initial findings? A prospective study with nine to ten years of follow-up. J Shoulder Elbow Surg 13(5):479–486. doi:10.1016/S1058274604000436
Lazarides S, Zafiropoulos G (2006) Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg 15(2):191–194. doi:10.1016/j.jse.2005.08.007
Hill JM, McGuire MH, Crosby LA (1997) Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 79(4):537–539
McKee MD, Wild LM, Schemitsch EH (2003) Midshaft malunions of the clavicle. J Bone Joint Surg 85:790–797
McKee MD, Pedersen EM, Jones C, Stephen DJ, Kreder HJ, Schemitsch EH, Wild LM, Potter J (2006) Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am 88(1):35–40. doi:10.2106/JBJS.D.02795
Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE (2004) Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 86-A(7):1359–1365
Eskola A, Vainionpaa S, Myllynen P, Patiala H, Rokkanen P (1986) Outcome of clavicular fracture in 89 patients. Arch Orthop Trauma Surg 105(6):337–338
Ban I, Branner U, Holck K, Krasheninnikoff M, Troelsen A (2012) Clavicle fractures may be conservatively treated with acceptable results—a systematic review. Dan Med J 59(7):A4457 pii:A4457
Virtanen KJ, Remes V, Pajarinen J, Savolainen V, Bjorkenheim JM, Paavola M (2012) Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: a randomized clinical trial. J Bone Joint Surg Am 94(17):1546–1553. doi:10.2106/JBJS.J.01999
Robinson CM, Goudie EB, Murray IR, Jenkins PJ, Ahktar MA, Read EO, Foster CJ, Clark K, Brooksbank AJ, Arthur A, Crowther MA, Packham I, Chesser TJ (2013) Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am 95(17):1576–1584. doi:10.2106/JBJS.L.00307
Canadian Orthopaedic Trauma S (2007) Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am 89(1):1–10. doi:10.2106/JBJS.F.00020
Kulshrestha V, Roy T, Audige L (2011) Operative versus nonoperative management of displaced midshaft clavicle fractures: a prospective cohort study. J Orthop Trauma 25(1):31–38. doi:10.1097/BOT.0b013e3181d8290e
Judd DB, Pallis MP, Smith E, Bottoni CR (2009) Acute operative stabilization versus nonoperative management of clavicle fractures. Am J Orthop (Belle Mead NJ) 38(7):341–345
Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS (2009) Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures—a randomized, controlled, clinical trial. J Orthop Trauma 23(2):106–112. doi:10.1097/BOT.0b013e318190cf88
McKee RC, Whelan DB, Schemitsch EH, McKee MD (2012) Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am 94(8):675–684. doi:10.2106/JBJS.J.01364
Jenkins PJ, Huntley JS, Robinson CM (2008) Primary fixation of displaced clavicle fractures: unanswered questions. J Bone Joint Surg 89A:1–10
Smekal V, Deml C, Irenberger A, Niederwanger C, Lutz M, Blauth M, Krappinger D (2008) Length determination in midshaft clavicle fractures: validation of measurement. J Orthop Trauma 22(7):458–462. doi:10.1097/BOT.0b013e318178d97d
Jones GL, Bishop JY, Lewis B, Pedroza AD, Group MS (2014) Intraobserver and interobserver agreement in the classification and treatment of midshaft clavicle fractures. Am J Sports Med 42(5):1176–1181. doi:10.1177/0363546514523926
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29(6):602–608. doi:10.1002/(SICI)1097-0274(199606)29:6<602:AID-AJIM4>3.0.CO;2-L
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Constant CR, Gerber C, Emery RJ, Sojbjerg JO, Gohlke F, Boileau P (2008) A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg 17(2):355–361. doi:10.1016/j.jse.2007.06.022
Finsen V (2008) Norwegian version of the DASH questionnaire for examination of the arm shoulders and hand. Tidsskr Nor Laegeforen 128(9):1070 pii:1685668
Roy JS, MacDermid JC, Woodhouse LJ (2009) Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum 61(5):623–632. doi:10.1002/art.24396
Kim KS, Kim MG (2010) Gender-related factors associated with upper extremity function in workers. Safety Health Work 1(2):158–166. doi:10.5491/SHAW.2010.1.2.158
Jester A, Harth A, Germann G (2005) Measuring levels of upper-extremity disability in employed adults using the DASH questionnaire. J Hand Surg 30(5):1074 e1071–1074 e1010. doi:10.1016/j.jhsa.2005.04.009
Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR (2005) Normalization of the Constant score. J Shoulder Elbow Surg 14(3):279–285. doi:10.1016/j.jse.2004.10.009
Wick M, Muller EJ, Kollig E, Muhr G (2001) Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch Orthop Trauma Surg 121(4):207–211
Thormodsgard TM, Stone K, Ciraulo DL, Camuso MR, Desjardins S (2011) An assessment of patient satisfaction with nonoperative management of clavicular fractures using the disabilities of the arm, shoulder and hand outcome measure. J Trauma 71(5):1126–1129. doi:10.1097/TA.0b013e3182396541
Stegeman SA, de Witte PB, Boonstra S, de Groot JH, Nagels J, Krijnen P, Schipper IB (2015) Posttraumatic midshaft clavicular shortening does not result in relevant functional outcome changes. Acta Orthop 86(5):542–552. doi:10.3109/17453674.2015.1040982
Nordqvist A, Redlund-Johnell I, von Scheele A, Petersson CJ (1997) Shortening of clavicle after fracture incidence and clinical significance, a 5-year follow-up of 85 patients. Acta Orthop Scand 68(4):349–351
Postacchini R, Gumina S, Farsetti P, Postacchini F (2010) Long-term results of conservative management of midshaft clavicle fracture. Int Orthop 34(5):731–736. doi:10.1007/s00264-009-0850-x
Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD (2005) Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma 19(7):504–507 pii:00005131-200508000-00017
Murray IR, Foster CJ, Eros A, Robinson CM (2013) Risk factors for nonunion after nonoperative treatment of displaced midshaft fractures of the clavicle. J Bone Joint Surg Am 95(13):1153–1158. doi:10.2106/JBJS.K.01275
Ballmer FT, Lambert SM, Hertel R (1998) Decortication and plate osteosynthesis for nonunion of the clavicle. J Shoulder Elbow Surg 7(6):581–585
Potter JM, Jones C, Wild LM, Schemitsch EH, McKee MD (2007) Does delay matter? The restoration of objectively measured shoulder strength and patient-oriented outcome after immediate fixation versus delayed reconstruction of displaced midshaft fractures of the clavicle. J Shoulder Elbow Surg 16(5):514–518. doi:10.1016/j.jse.2007.01.001
van der Meijden OA, Houwert RM, Hulsmans M, Wijdicks FJ, Dijkgraaf MG, Meylaerts SA, Hammacher ER, Verhofstad MH, Verleisdonk EJ (2015) Operative treatment of dislocated midshaft clavicular fractures: plate or intramedullary nail fixation? A randomized controlled trial. J Bone Joint Surg Am 97(8):613–619. doi:10.2106/JBJS.N.00449
Acknowledgments
Dr. Fuglesang has received funding from Akershus University Hospital and from the Sophies Minde foundation. This funding also paid for radiographs. No other authors received any financial support for this study. We are grateful for the cooperation from Dr. Hasan Banitalebi, Department of Radiology, Akershus University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest.
Rights and permissions
About this article
Cite this article
Fuglesang, H.F.S., Flugsrud, G.B., Randsborg, PH. et al. Radiological and functional outcomes 2.7 years following conservatively treated completely displaced midshaft clavicle fractures. Arch Orthop Trauma Surg 136, 17–25 (2016). https://doi.org/10.1007/s00402-015-2354-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2354-z