Abstract
Objective
The purpose of this study is to compare the effectiveness and safety of cervical disc arthroplasty with anterior cervical discectomy and fusion for treatment of symptomatic cervical disc disease.
Summary of background data
Anterior cervical discectomy and fusion (ACDF) is the conventional surgical treatment for symptomatic cervical disc disease. Recently, cervical disc arthroplasty (CDA) has been developed to address some of the shortcomings associated with ACDF by preserving function of the motion segment. Controversy still surrounds regarding whether CDA is better.
Methods
We systematically searched six electronic databases (Medline, Embase, Clinical, Ovid, BIOSIS and Cochrane registry of controlled clinical trials) to identify randomized controlled trials (RCTs) published up to April 2014 in which CDA was compared with ACDF for the treatment of symptomatic cervical disc disease. Effective data were extracted after the assessment of methodological quality of the trials. Then, we performed the meta-analysis.
Results
Eighteen relevant RCTs with a total of 4061 patients were included. The results of the meta-analysis indicated that CDA was superior to ACDF regarding better neurological success (P < 0.00001), greater motion preservation at the operated level (P < 0.00001), fewer secondary surgical procedures (P < 0.00001), and fewer rates of adverse events (P < 0.00001) but inferior to ACDF regarding operative times (P < 0.00001). No significant difference was identified between the two groups regarding blood loss (P = 0.87), lengths of hospital stay (P = 0.76), neck pain scores (P = 0.11) and arm pain scores (P = 0.78) reported on a visual analog scale.
Conclusion
The meta-analysis revealed that CDA demonstrated superiorities in better neurological success, greater motion preservation at the operated level, lower rate of adverse events and fewer secondary surgical procedures compared with ACDF. However, the benefits of blood loss, lengths of hospital stay, neck and arm pain functional recovery are still unable to be proved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and fusion (ACDF) remains the established gold standard treatment for symptomatic cervical disc disease [1, 2], but it has the drawbacks of the loss of motion at the operated segment and adjacent segmental disc degeneration [3–5]. Recently, cervical disc arthroplasty (CDA), a motion-preserving option, has been used to treat the patients with symptomatic cervical disc disease [6, 7]. But there is still a controversy whether CDA is more effective and safer than ACDF [8]. Previous meta-analyses concluded that CDA shows the significant superiority (lengths of hospital stay, clinical indices, range of motion at the operated level, adverse events, and secondary surgical procedures) for the treatment of symptomatic cervical disc disease compared with ACDF [9–12]. However, these meta-analyses were based on a small sample size and insufficient analyses. The need remains for strong evidence based on the latest high-quality RCTs to test the above conclusion. The purpose of this study was to perform a meta-analysis of the available evidence comparing CDA with ACDF for the treatment of symptomatic cervical disc disease.
Materials and methods
Search methods
Up to April 2014, all published RCTs comparing CDA with ACDF for the treatment of symptomatic cervical disc disease were searched for by two authors (MJR and SPN) independently. We performed the research of Medline, Embase, Clinical, Ovid, BIOSIS and Cochrane central registry of controlled trials. A manual search of Spine, European Spine Journal, and the American and British versions of Journal of Bone and Joint Surgery was also performed to identify additional studies. There was no language restriction. Key words used for search were as follows: cervical disc disease, anterior cervical discectomy, cervical disc replacement and randomized controlled trial.
Criteria for selected trials
Two reviewers (MJR and SPN) checked titles and abstracts identified from the database. Full text for items that could not be decided on the basis of titles and abstracts were retrieved for second-round selection. All randomized controlled clinical trials (RCTs) comparing CDA with ACDF for the treatment of symptomatic cervical disc disease were taken into consideration. Multiple publications of the same study were not included. The indication for surgical treatment was radiculopathy, myelopathy, or disc herniation that failed to respond to at least 6 weeks of conservative treatment. Patients older than 18 years with symptomatic cervical disc disease were included in this study. The interventions included various types of CDA in the cervical spine. Studies with patients who had acute spinal fracture, infection, tumor, osteoporosis, or rheumatoid arthritis were excluded. The reviewers applied the inclusion criteria to select the potentially appropriate trials. Disagreements between two investigators were resolved by discussion, and a consensus was attempted.
Data extraction
Two reviewers participated in the extraction of relevant data from the included reports. One reviewer (MJR) extracted all relevant data onto a table; a second reviewer (SPN) checked the data. A third reviewer (SSC) was consulted for the final decision if any disagreement on eligibility existed between the first two reviewers. The data extracted to describe characteristics of the investigations were characteristics of participants, intervention details, number of participants in each intervention group, sex radio, follow-up rate and period.
Methodological assessment
The modified Jadad scale was used as the methodological assessment for the study [13]. There are eight items designed to assess randomization, blinding, withdrawals and dropouts, inclusion and exclusion criteria, adverse effects and statistical analysis (Table 1). The score could range from 0 to 8. Scores of 0–3 indicate poor-to-low quality and 4–8 good-to-excellent quality. Critical appraisal was conducted by one viewer (GHZ) and was verified by another (BWX).
Outcomes for meta-analysis
Surgical parameters (operative time, blood loss, and length of hospital stay), clinical indices [visual analog scale (VAS) neck and arm pain scores, and neurological success], range of motion at the operated level, adverse events, and secondary surgical procedures were the primary criteria by which the studies included in the meta-analysis were evaluated. The motion at the operated level was determined by drawing lines between the superior endplate of the operated cranial vertebra and the inferior endplate of the operated caudal vertebra in dynamic flexion and extension lateral views [20].
Statistical analysis
The Q- and I 2-statistics were used to test for statistical heterogeneity [14, 15]. The Q-statistic tested the null hypothesis that all studies shared a common effect size with minimal dispersion of the effect size across studies. I2 can be readily calculated from basic results obtained from a typical meta-analysis as, I 2 = 100 % × (Q − df)/Q, where Q is Cochrane’s heterogeneity statistic and df is the degrees of freedom. An I 2 value less than 25 % was considered homogeneous, an I 2-statistic between 25 and 50 % as low heterogeneity, an I 2-statistic between 50 and 75 % as moderate heterogeneity, and an I 2-statistic above 75 % as high heterogeneity [15]. Dichotomous variables are presented as relative risk (RR) and continuous variables as mean difference (MD), both with 95 % confidence intervals (CI) and probability value. These data were calculated when one outcome was assessed in different ways in different trials. The meta-analysis was performed by RevMan 5.2 software (Cochrane Collaboration, Oxford, UK) for outcome measures. A level of P ≤ 0.05 was considered statistically significant.
Results
Search results
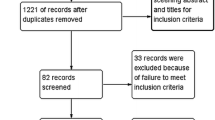
The process of searching relevant literature and the results are shown in Fig. 1. Eighteen published RCTs [16–33] with a total of 4,061 patients were included according to the inclusion criteria. The characteristics of the studies and participants are listed in Table 2.
Results of methodological quality
As shown in Table 2, it is indicated that most studies achieved high quality by modified Jadad scale. All the designs scored ≥4, but the main shortcoming reflected in nearly all studies was the lack of blinding method, which might lead to a certain degree of detection bias. All of the participants in the included studies had performed the follow-up more than 2 years. Of these, three studies [16, 25, 28] were performed for 5 years follow-up.
Heterogeneity
There were similar demographic characteristics, pain and functioning status baseline for the participants from the 18 included studies. Four different artificial discs (Prestige ST, ProDisc-C, Bryan and Kineflex\C) were used in these studies. Different anterior plates and sources of the bone were performed in these studies. The surgical data were not pooled together because of the above differences. Most outcomes were measured by the same method in the studies. In fixed-effects meta-analysis, heterogeneity was observed in operation time (I 2 = 81 %, P < 0.00001), blood loss (I 2 = 89 %, P = 0.87), length of the hospital stay (I 2 = 76 %, P = 0.76), range of motion at the operated level (I 2 = 97 %, P < 0.00001). The outcomes regarding neurological success were consistent (I 2 = 0 %) and secondary surgical procedures (I 2 = 13 %).
Meta-analyses results
Surgical parameters
Eighteen studies with a total of 4,061 patients (2,144 in CDA group and 1,917 in ACDF group) were eligible for meta-analysis. The operative time was significantly longer in the CDA group (MD 17.03, 95 % CI 13.92, 20.13, P < 0.00001, Fig. 2). However, Fig. 3 shows that there was no significant difference in blood loss (MD −0.41, 95 % CI −5.12, 4.31, P = 0.87). Also, the length of the hospital stay did not differ significantly between the two groups (MD −0.01, 95 % CI −0.08, 0.06, P = 0.76, Fig. 4).
Clinical Indices
No statistically significant difference was found between the two groups in the neck pain scores (MD −0.25; 95 % CI −0.56, 0.06, P = 0.11, Fig. 5) and the arm pain scores (MD 0.04, 95 % CI −0.23, 0.31, P = 0.78, Fig. 6). However, the CDA group had significant superiority in neurological success (OR 1.57, 95 % CI 1.30, 1.90, P < 0.00001, Fig. 7), range of motion at the operated level (OR 6.95, 95 % CI 6.81, 7.09, P < 0.00001, Fig. 8), the rate of adverse events (OR 0.58, 95 % CI 0.46, 0.73, P < 0.00001, Fig. 9), and secondary surgical procedures in the arthroplasty group (OR 0.47, 95 % CI 0.34, 0.65, P < 0.00001, Fig. 10) compared with the ACDF group.
Discussion
Anterior cervical discectomy and fusion (ACDF) is a well-established procedure for the treatment of symptomatic cervical disc disease [34, 35]. However, the original biomechanics of the cervical spine was altered because of the loss of range of motion at the fused segments [4]. Besides, spinal fusion is commonly associated with the complication of adjacent disc degeneration [36, 37]. Hilibrand et al. [38] reported that annually 2.9 % of patients developed adjacent segment disease after anterior interbody fusion that required cervical intervention. The loss of the motion at the fused segments can cause significant neck pain, poor functional recovery, cervical instability and accelerated adjacent disc degeneration, for which additional operations are often required [39].
Cervical disc arthroplasty (CDA) has increased in popularity as an alternative for symptomatic cervical disc disease [7]. The technique is to restore and maintain the original biomechanics of cervical spine, which is attempted to prevent adjacent level degeneration at the operated segments [6, 40]. However, controversy still surrounds regarding whether CDA is better than ACDF. The purpose of this study is to compare the effectiveness and the safety of CDA to ACDF for the treatment of symptomatic cervical disc disease.
Results of our meta-analysis that included a greater number of latest RCTs available once again confirmed that CDA shows significant superiority in maintaining range of motion at the operated level compared with ACDF. This is in accordance with the conclusion proposed by Gao et al. [11]. Our meta-analysis, however, offered new findings. Our meta-analysis indicated that there was no significant difference between the two groups regarding blood loss, lengths of hospital stay, neck pain scores and arm pain scores reported on a visual analog scale. In other words, the two groups had a similar surgical procedures and quality of life.
Some basic epidemiological information of the participants can be derived from Table 2. It is noticeable that the number of CDA was almost equivalent to the fusion group except Davis et al. [18] (2:1). Secondly, most cervical disc disease patients were in their 40s–50s. This indicated that the middle-aged population should be given more attention on cervical activities because their cervical intervertebral discs are no longer as good as they were in adolescence. Thirdly, sex ratio was 1:1 and may indicate that it has no correlation with cervical disc disease.
The previous meta-analysis [11] confirmed that the surgical parameters (operative times and blood loss) for ACDF were superior or equivalent to those for CDA and other outcomes (length of hospital stay, clinical indices, range of motion at the operated level, adverse events, and secondary surgical procedures) for CDA were superior or equivalent to the same outcomes for ACDF. The latest four high-quality RCTs [16–19] which compare CDA to ACDF were added in our study, with a total of 4,061 patients. When effective data from the 18 high-quality included studies were pooled, we find that the patients with CDA had a better neurological success, greater motion preservation at the operated level, lower rate of adverse events and fewer secondary surgical procedures. There was no significant difference in blood loss, lengths of hospital stay, neck and arm pain functional recovery between CDA group and the ACDF group.
Our meta-analysis indicates that cervical disc arthroplasty provided better recovery of neurologic dysfunction than anterior cervical discectomy and fusion. Patients treated with cervical disc arthroplasty showed a higher neurologic success rate than those of the fusion group. The reason for greater improvement in neurologic recovery after cervical disc arthroplasty potentially could be related to the maintenance of motion in the cervical spine. However, cervical disc arthroplasty did not showed superiority in pain relief compared with fusion. The pooled data for the arm and neck VAS scores indicated that cervical arthroplasty procedures resulted in equivalent decompression to that of anterior cervical discectomy and fusion. This relief of clinical symptoms was achieved by adequate decompression of the spinal cord and nerve roots that were being compressed by herniated discs or osteophytes, and these patients benefited from reconstruction of the spinal column. All function outcomes evaluated after cervical disc arthroplasty were superior or at least equivalent to those after fusion except the operative time in our study. This is in accordance with the conclusion proposed by Murrey et al. [21], who considered the increased operative time for arthroplasty to be attributable to the time required to learn the new technique and time due to additional use of fluoroscopy.
Cervical disc arthroplasty was more durable with lower rate of adverse events and fewer secondary surgical procedures related to index surgeries compared with the fusion in our analysis. Adverse events include implant-related adverse events and surgery-related adverse events (i.e., dysphagia, edema, gastrointestinal symptoms, genitourinary symptoms, dural tear, infection, and pain) [16]. Secondary surgical procedures were defined as any reoperation, revision, supplemental fixation, or removal of the implant [16]. The RRs for the adverse events rates were 0.58, supporting cervical disc arthroplasty rather than fusion (P < 0.00001). Cervical disc arthroplasty also was associated with a fewer secondary surgical procedure (4.16 %) than anterior cervical decompression and fusion (8.48 %). We considered the lower rate of adverse events and fewer secondary surgical procedures for arthroplasty to be attributable to the followings. First, to some certain extent, artificial disc arthroplasty recovers the functional units of the spine, mitigates extra loads on adjacent segments and eases intervertebral pressure at adjacent levels. In addition, we noted that patients who had severe facet joint degenerative disease or adjacent segment degeneration were excluded from cervical arthroplasty group.
In our meta-analysis, 18 published RCTs on CDA versus ACDF were analyzed. All the studies had good methodological qualities (Jadad scores ≥4) which imply a lower risk of bias. The most prevalent methodological shortcomings appeared to be insufficient regarding the blinding method and intention-to-treat analysis. None of the included studies did blinding method for the patients and encompassed the information of intention-to-treat analyses. We consider that blinding is not always feasible because of the nature of the surgical intervention, adequate allocation concealment is always possible in a RCT. Different types of cervical artificial disc may affect the comparing outcomes between the interventions, although no cervical artificial disc is shown to be superior or inferior to the others. We did not assess the relative outcomes of arthroplasty in subgroups with different types of prostheses for stratified analysis because of the limited number of included trials. Furthermore, the CDA group attempted to exclude patients with severe facet joint disease or degeneration because of the maintenance of the operated level motion. This limitation may be another potential source of bias for the final conclusion. As the follow-ups for our studies examined were no longer than 5 years, it was impossible to draw conclusions regarding the long-term results of follow-up.
In addition, the results are affected by heterogeneity. For example, the results of operation time, blood loss, lengths of the hospital stay and range of motion at the operated level presented significant heterogeneity. Of the 18 RCTs, only 4 studies mentioned the motion at the operated level and found significant difference between the two groups. But a high heterogeneity (I 2 = 97 %) existed among these studies, probably because the measuring errors are inevitable in measuring process. Therefore, the results of this meta-analysis should be cautiously accepted. Besides, the benefits of surgical parameters and quality of life still remain unproved from the existing data. More independent high-quality RCTs with long-term outcomes are needed to strengthen the quality of evidence and contribute information to complement the findings.
Conclusion
In summary, our meta-analysis revealed that CDA demonstrated superiorities in better neurological success, greater motion preservation at the operated level, lower rate of adverse events and fewer secondary surgical procedures compared with ACDF. However, the outcomes of blood loss, lengths of hospital stay, neck and arm pain functional recovery are equivalent to the ACDF group. The studies with high methodologic quality and long-term follow-up periods are needed for updated meta-analyses to better evaluate the two procedures for treatment of symptomatic cervical disc disease.
References
Moon HJ, Kim JH, Kim JH et al (2011) The effects of anterior cervical discectomy and fusion with stand-alone cages at two contiguous levels on cervical alignment and outcomes. Acta Neurochir (Wien) 153(3):559–565
Lied B, Roenning PA, Sundseth J et al (2010) Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg 10:10
Xu R, Bydon M, Macki M et al (2014) Adjacent segment disease after anterior cervical discectomy and fusion: clinical outcomes after first repeat surgery versus second repeat surgery. Spine (Phila Pa 1976) 39(2):120–126
Chung JY, Kim SK, Jung ST et al (2014) Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J 14:2290–2298
Li Z, Yu S, Zhao Y et al (2014) Clinical and radiologic comparison of dynamic cervical implant arthroplasty versus anterior cervical discectomy and fusion for the treatment of cervical degenerative disc disease. J Clin Neurosci 21:942–948
Demetriades AK, Ringel F, Meyer B (2014) Cervical disc arthroplasty: a critical review and appraisal of the latest available evidence. Adv Tech Stand Neurosurg 41:107–129
Khong P, Bogduk N, Ghahreman A et al (2013) Cervical disc arthroplasty for the treatment of spondylotic myelopathy and radiculopathy. J Clin Neurosci 20(10):1411–1416
Moatz B, Tortolani PJ (2012) Cervical disc arthroplasty: pros and cons. Surg Neurol Int 3(Suppl 3):S216–S224
Yin S, Yu X, Zhou S et al (2013) Is cervical disc arthroplasty superior to fusion for treatment of symptomatic cervical disc disease? A meta-analysis. Clin Orthop Relat Res 471(6):1904–1919
Xing D, Ma XL, Ma JX et al (2013) A meta-analysis of cervical arthroplasty compared to anterior cervical discectomy and fusion for single-level cervical disc disease. J Clin Neurosci 20(7):970–978
Gao Y, Liu M, Li T et al (2013) A meta-analysis comparing the results of cervical disc arthroplasty with anterior cervical discectomy and fusion (ACDF) for the treatment of symptomatic cervical disc disease. J Bone Joint Surg Am 95(6):555–561
Jiang H, Zhu Z, Qiu Y et al (2012) Cervical disc arthroplasty versus fusion for single-level symptomatic cervical disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 132(2):141–151
Oremus M, Wolfson C, Perrault A et al (2001) Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord 12(3):232–236
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Zigler JE, Delamarter R, Murrey D et al (2013) ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine (Phila Pa 1976) 38(3):203–209
Phillips FM, Lee JY, Geisler FH et al (2013) A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. 2-year results from the US FDA IDE clinical trial. Spine Phila Pa (1976) 38(15):E907–E918
Davis RJ, Kim KD, Hisey MS et al (2013) Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial: clinical article. J Neurosurg Spine 19(5):532–545
Coric D, Kim PK, Clemente JD et al (2013) Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. J Neurosurg Spine 18(1):36–42
Zhang X, Zhang X, Chen C et al (2012) Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China. Spine (Phila Pa 1976) 37(6):433–438
Murrey D, Janssen M, Delamarter R et al (2009) Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 9(4):275–286
Sasso RC, Smucker JD, Hacker RJ et al (2007) Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective, randomized, controlled, multicenter trial with 24-month follow-up. J Spinal Disord Tech 20(7):481–491
Steinmetz MP, Patel R, Traynelis V et al (2008) Cervical disc arthroplasty compared with fusion in a workers’ compensation population. Neurosurgery 63(4):741–747
Wang Y, Cai B, Zhang XS et al (2008) Clinical outcomes of single level Bryan cervical disc arthroplasty: a prospective controlled study. Zhonghua Wai Ke Za Zhi 46(5):328–332
Burkus JK, Haid RW, Traynelis VC et al (2010) Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 13(3):308–318
Heller JG, Sasso RC, Papadopoulos SM et al (2009) Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 34(2):101–107
Coric D, Cassis J, Carew JD et al (2010) Prospective study of cervical arthroplasty in 98 patients involved in 1 of 3 separate investigational device exemption studies from a single investigational site with a minimum 2-year follow-up. Clinical article. J Neurosurg Spine 13(6):715–721
Mummaneni PV, Burkus JK, Haid RW et al (2007) Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 6(3):198–209
Cheng L, Nie L, Li M et al (2011) Superiority of the Bryan((R)) disc prosthesis for cervical myelopathy: a randomized study with 3-year follow up. Clin Orthop Relat Res 469(12):3408–3414
Coric D, Nunley PD, Guyer RD et al (2011) Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 15(4):348–358
Garrido BJ, Taha TA, Sasso RC (2010) Clinical outcomes of Bryan cervical disc arthroplasty a prospective, randomized, controlled, single site trial with 48-month follow-up. J Spinal Disord Tech 23(6):367–371
Cheng L, Nie L, Zhang L et al (2009) Fusion versus Bryan Cervical Disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop 33(5):1347–1351
Sasso RC, Anderson PA, Riew KD et al (2011) Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am 93(18):1684–1692
Brenke C, Dostal M, Carolus A et al (2014) Clinical relevance of neuroforaminal patency after anterior cervical discectomy and fusion. Acta Neurochir (Wien) 156:1197–1203
Dagli M, Er U, Simsek S et al (2013) Late results of anterior cervical discectomy and fusion with interbody cages. Asian Spine J 7(1):34–38
Xu R, Bydon M, Macki M et al (2014) Adjacent segment disease after anterior cervical discectomy and fusion: clinical outcomes after first repeat surgery versus second repeat surgery. Spine Phila Pa (1976) 39(2):120–126
Bydon M, Xu R, Macki M et al (2014) Adjacent segment disease after anterior cervical discectomy and fusion in a large series. Neurosurgery 74(2):139–146
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4(6 Suppl):190S–194S
Aghayev K, Doulgeris JJ, Gonzalez-Blohm SA et al (2014) Biomechanical comparison of a two-level anterior discectomy and a one-level corpectomy, combined with fusion and anterior plate reconstruction in the cervical spine. Clin Biomech (Bristol, Avon) 29(1):21–25
Fay LY, Huang WC, Tsai TY et al (2014) Differences between arthroplasty and anterior cervical fusion in two-level cervical degenerative disc disease. Eur Spine J 23(3):627–634
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rao, MJ., Nie, SP., Xiao, BW. et al. Cervical disc arthroplasty versus anterior cervical discectomy and fusion for treatment of symptomatic cervical disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 135, 19–28 (2015). https://doi.org/10.1007/s00402-014-2122-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2122-5