Abstract
Background
Although the validity of the “lateral gutter drive-through” (LGDT) test has been proved to offer high sensitivity and specificity in diagnosing the posterolateral rotational instability of knee joints, the real mechanism on how the injury pattern of individual posterolateral knee structure triggers the positive LGDT sign still remains unknown.
Hypothesis
A certain amount of popliteus tendon (POP-T) laxity resulted from specific injury patterns of individual posterolateral knee structure or some degree of medial structural injury will lead to positive LGDT sign.
Study design
Controlled laboratory study.
Methods
Seven non-paired intact cadaveric knees were divided into four groups and tested under unique sequential sectioning sequences including: (1) distal POP-T and popliteofibular ligament (PFL) (n = 2); (2) PFL and distal POP-T (n = 3); (3) lateral collateral ligament (LCL), distal POP-T and PFL (n = 1); (4) superficial medial collateral ligament (sMCL), deep MCL, posterior oblique ligament (POL), anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) (n = 1). The LGDT tests and the measurements of external tibial rotational angle (ETRA) were first performed on all the intact knees and then at each time point when an additional structure was sectioned. Results of each LGDT test and the absolute value of increased ETRA compared with the intact knee were recorded. Each knee was tested at 30° of flexion. A navigation system was used to measure motion changes of the tibia with respect to the femur.
Results
Initially, the LGDT tests all showed negative on each of the intact knee. Isolated sectioning of the distal POP-T, PFL or the LCL produced increased but insignificant ETRA with the LGDT tests still negative. However, simultaneous sectioning of the distal POP-T and PFL produced significantly increased ETRA with the LGDT tests changed to positive. In addition, for the knee with medial structural injuries, the LGDT test could also be positive only when the posteromedial structures (sMCL, deep MCL, POL) and the cruciate ligaments (ACL and PCL) were all sectioned.
Conclusion
In this cadaveric sequential sectioning study, the LGDT test showed positive merely at the following two situations: (1) the distal POP-T and PFL were both sectioned; (2) the posteromedial structures (sMCL, deep MCL and POL) and the cruciate ligaments (ACL and PCL) were all sectioned.
Clinical relevance
Accuracy of the LGDT test in diagnosing acute or chronic posterolateral corner (PLC) injuries will improve with the information in this study. It was the combined POP-T and PFL injuries that finally led to a positive LGDT sign. However, one should be cautious to use the LGDT test in diagnosing the PLC injuries when posteromedial structures and cruciate ligaments were all involved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The posterolateral corner (PLC) and posterolateral rotational instability (PLRI) of the knee have received ever-increasing attentions in the literature, particularly when an injury to this structure occurs in combination with posterior cruciate ligament (PCL) deficiency [1–4]. The complex anatomy and variable injury patterns of the PLC has resulted in controversy and confusion for the diagnosis of PLC injuries.
According to the literature, the most commonly used diagnostic methods of PLC injuries were comprehensive physical examinations, including the dial test, the reverse pivot-shift test, the external rotational recurvatum test and the posterolateral drawer test [5]. Although accuracy of these tests might prevent knee surgeons from missing the combined PLRI that should be corrected in a PCL deficient knee, they were somewhat subjective tests which relied on subtleties in the physical examinations, especially when one was facing acute, concurrent multi-ligament injuries [6–9]. Recently, it was reported that the “lateral gutter drive-through” (LGDT) test was effective in identifying the femoral “peel-off” lesions as well as the chronic PLRI [10]. The positive LGDT, which was defined as the arthroscope could pass into the posterolateral compartment through the interval between the popliteus tendon (POP-T) and the lateral femoral condyle at 30° of knee flexion, indicated the PLRI of knee joints.
Although validity of the LGDT test has been proved to offer high sensitivity and specificity, the true mechanism needs to be further clarified in favor of its adequate applications. The major limitations of the previous studies were that the clinical interpretations of LGDT test were actually based on the excessive external tibial rotational angle (ETRA) rather than the individual posterolateral knee structures such as the POP-T or the popliteofibular ligament (PFL) [11, 12]. It was well understandable that the proximal POP-T injury described as “peel-off” lesion by Shen et al. [12] could trigger positive LGDT sign. However, in terms of the distal PLC injury patterns, which were clinically more common and might also be diagnosed by the LGDT test, the real mechanism still remained unknown.
Moreover, in the study of Shen et al. [12], the medial structural injuries of knee joints were entirely excluded due to their potential influences to the final results and, therefore, the degree on how the medial structural injuries would affect the performance of LGDT test was not mentioned.
The main purposes of this study were: (1) to investigate the effect of distal individual structures of PLC on this novel arthroscopic test for the diagnosis of PLRI and (2) to identify the extent of medial structural injuries that could induce the positive LGDT sign. We hypothesized that a certain amount of POP-T laxity resulted from specific injury patterns of individual posterolateral knee structure or some degree of medial structural injury will lead to positive LGDT sign.
Materials and methods
Specimen preparation
This study used seven non-paired fresh-frozen human cadaveric knees. Approval of the study was obtained through the institutional review board at Peking University Fourth School of Clinical Medicine (Beijing Jishuitan Hospital). The mean age of the specimens was 38.3 ± 11.4 years (range 25–52 years). All specimens indicated no evidence of injury or instability by physical examination. The specimens were stored at −20 °C and thawed overnight before testing. The hip was disarticulated, and the foot was kept intact to simulate a dial test. The skin and subcutaneous fat were removed from the knees, leaving the superficial fascia intact. The posterolateral knee was exposed to the superficial crural fascia layer, and all individual posterolateral structures were left intact.
Study design
This was a sequential sectioning cadaveric study. All the seven specimens were divided into four groups. Four sequential sectioning sequences were performed involving sectioning of (1) the POP-T; (2) the PFL; (3) the lateral collateral ligament (LCL); (4) the posteromedial structures including the superficial medial collateral ligament (sMCL), the deep MCL and the posterior oblique ligament (POL); (5) the cruciate ligaments including the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) (Fig. 1). The detailed sectioning sequences are displayed in Fig. 2. Surgical exposure to the posterolateral and posteromedial structures of the knee was previously described by LaPrade et al. [13, 14]. The POP-T was initially sectioned at the popliteus musculotendinous junction, distal to the PFL, to ensure the integrity of the PFL function. The PFL was sectioned at its fibular insertion site.
Diagrams of sequential sectioning techniques. a The popliteus tendon (POP-T) was sectioned at the popliteus musculotendinous junction, distal to the popliteofibular ligament (PFL) (black arrow), to ensure the integrity of the PFL function. b The PFL was sectioned at its fibular insertion site (black arrow). c The lateral collateral ligament (LCL) was sectioned at its mid-substance portion (black arrow). d The posteromedial structures and both the cruciate ligaments were all sectioned (black arrow)
The LGDT tests and the measurements of ETRA were first performed on all the intact knees and then at each time point when an additional structure was sectioned. For each of the sectioned state, the measurements of ETRA were performed five times and the mean values were recorded as the final results.
The description of LGDT test
A standard 5.5 mm diameter arthroscope was placed in the lateral gutter through an anterolateral portal with the knee at 30° of flexion with neutral tibial rotation. First, the lateral femoral condyle and femoral insertion of the POP-T at the lateral gutter of the knee were indentified. Then the surgeon tried to insert the arthroscope through the interval between the POP-T and the lateral femoral condyle into the posterolateral compartment of the knee without any varus or valgus stress applied to the tibia (Fig. 3). The LGDT test was defined as positive if the arthroscope passed through the interval and entered the posterolateral compartment. If the arthroscope could not pass through the interval, the LGDT test was defined as negative.
Diagram of the “lateral gutter drive through” (LGDT) test. A standard 5.5-mm diameter arthroscope was placed in the anterolateral portal with the knee at 30° of flexion. First, the lateral condyle and femoral insertion of the popliteus tendon (POP-T) at the lateral gutter of the knee were identified. Then, the surgeon tried to insert the arthroscope through the interval between the POP-T and the lateral condyle into the posterolateral compartment of the knee
The measurement of ETRA
An intraoperative navigation system (Brainlab, Feldkirchen, Germany) was used for measurement of the ETRA. The specimens were placed on a custom-made testing apparatus in which the femoral head was rigidly held and was allowed free movement for calibration of the navigation. Two 4.5-mm Schanz screws were inserted into the anteromedial aspect of the tibia for anchoring the tibial trackers of the navigation system (Fig. 4). Another two parallel 4.5-mm Schanz screws were inserted into the anterolateral aspect of the femur for anchoring the femoral trackers of the navigation system. A 5-Nm torque was applied to the tibia for application of external rotation torque during the measurement. Each knee was measured at 30° of flexion.
Biomechanical test of a left knee with the navigation system. Two trackers were fixed to the femur and tibia, which were tracked by the navigation system. The real-time changes of flexion and external rotation angle of the knee were calculated by the computer. A 5 Nm torque was applied to the tibia for application of external rotation torque during the test
Statistical analysis
Results of the LGDT tests were first systematically recorded on the intact knees and then at each sectioned state within the four groups. In addition, the paired t tests were used to determine the increased mean ETRA between the intact and all sectioned states at 30° of flexion. A significant difference was determined to be P < 0.05.
Results
Sequential sectioning effect on LGDT tests
Initially, the LGDT tests showed negative on all the intact knees. In group 1 and group 2, isolated sectioning of the distal POP-T or the PFL (first section) still resulted in negative LGDT tests. However, additional sectioning of the PFL or the distal POP-T (second section) both resulted in positive LGDT tests. In group 3, the LGDT test finally showed positive until the LCL, distal POP-T and the PFL were all sectioned.
In group 4, isolated sectioning of the posteromedial structures (sMCL, deep MCL and POL) resulted in negative LGDT test. However, additional sectioning of both the cruciate ligaments (ACL and PCL) finally changed the LGDT test into positive (Fig. 5).
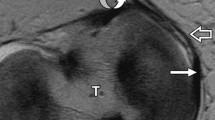
Arthroscopic view of the “lateral gutter drive through” (LGDT) test in a left knee. a The surgeon tried to insert the arthroscope through the interval between the popliteus tendon (POP-T) and the lateral femoral condyle. However, the arthroscope could not enter the interval, indicating a negative LGDT test. b The arthroscope could enter the interval between the POP-T and the lateral femoral condyle. The laxity of POP-T finally resulted in a positive LGDT test. F femoral condyle, POP-T popliteus tendon)
Sequential sectioning effect on increased ETRA
The mean ETRA at 30° of flexion in the intact knee was 13.4° ± 3.4°. In group 1 and group 2, isolated sectioning of the distal POP-T or the PFL (first section) resulted in increases in mean ETRA of 1.3° and 2.0°, respectively. These changes were not statistically significant (P > 0.05). Additional sectioning of the PFL or the distal POP-T (second section) resulted in a greater increase in mean ETRA of 2.8° and 2.8°, respectively. This increase, although small, was statistically significant (P = 0.03). In group 3, isolated sectioning of the LCL resulted in increases in mean ETRA of 2.0°, which was not statistically significant (P > 0.05). Additional sectioning of the distal POP-T and the PFL resulted in a greater increase in mean ETRA of 2.8°, which was statistically significant (P = 0.03).
In group 4, initial sectioning of the posteromedial structures (sMCL, deep MCL and POL) produced a slight increase in mean ETRA of 2.0°, which was not statistically significant (P > 0.05). However, subsequent sectioning of both the cruciate ligaments (ACL and PCL) led to a statistically significant increase in mean ETRA of 20.0° (P = 0.001) (Table 1).
Discussion
The most important findings of this cadaveric study were the LGDT tests showed positive merely at the following two situations: (1) the distal POP-T and the PFL were both sectioned; (2) the posteromedial structures (sMCL, deep MCL and POL) and the cruciate ligaments (ACL and PCL) were all sectioned.
Results of the present study showed that individual sectioning of any single structure of the PLC could not lead to positive LGDT sign, whereas sectioning of both distal POP-T and PFL could decrease the tension of the proximal POP-T to a certain amount, enlarge the interval between the POP-T and lateral femoral condyle and subsequently lead to positive LGDT sign.
To quantify the extent of proximal POP-T laxity that was adequate to trigger the positive LGDT sign, the parameter of increased ETRA measured by a navigation system was used for assessments. As a result, a 2.8° of the mean ETRA increase was identified to be the threshold of positive LGDT sign. This result was comparable to a recent cadaveric study conducted by Zhang et al. [15], who concluded that after sectioning both the POP-T and PFL, the mean ETRA significantly increased by 2.8° at 30° of knee flexion, whereas sectioning of either one of these two structures alone produced smaller mean ETRA increases (0.5° and 2.0°) that were not statistically significant. In another clinical study conducted by Shen et al. [12], the sensitivity of LGDT test was found to be correlated with the extent of the tibial external rotational instability and was significantly higher in patients with a side-to-side increase in ETRA by more than 10°. The difference of the threshold in ETRA might be due to the baseline injury patterns between the studies. In the study of Shen et al. [12], all the patients enrolled in the study group were diagnosed with combined injuries of PLC and PCL which contributed much more increase to the ETRA, whereas in the present cadaveric study as well as the one conducted by Zhang et al. [15], isolated PLC injury models were created without violating the PCL during the ETRA measurements. This finding clarified that it was the laxity of proximal POP-T, rather than the mean ETRA increase that was emphasized by Shen et al. [12], could be the real mechanism of positive LGDT sign.
In the present study, the LCL was not found to be contributed to the positive LGDT sign. During the study, we arthroscopically observed the lateral gutter of tested knee joint and confirmed the negative effect of LCL on the enlargement of interval between the POP-T and lateral femoral condyle. Our results further supported the finding of Shen et al. [12] that the LGDT test indicated external rotation instability regardless of the LCL involved or not.
In addition, the results of our study demonstrated that influence of the medial structures on positive LGDT sign was limited. Isolated sectioning of the posteromedial structures (sMCL, deep MCL and POL) could not produce positive LGDT sign. Subsequent sectioning of both the cruciate ligaments (ACL and PCL) triggered medial subluxation of the knee joint and finally led to positive LGDT sign. This finding could be explained by the mechanism that sufficient change of anatomical congruence between the knee joints caused pseudo-laxity of the proximal POP-T in reference to the lateral femoral condyle, which could be regarded as another mechanism of positive LGDT sign.
Strengths and limitations
The present study offers two advantages. First, this is the first study to investigate the real mechanism of the positive LGDT sign based on the individual posterolateral knee structures rather than the posterolateral rotational instability, which provided valuable information in improving the accuracy of the LGDT test in diagnosing the PLC injuries. Second, quantification of the ETRA was accomplished with the help of the navigation system, which was more accurate and convincing than the previous studies.
One limitation of this study was that we failed to create an injury model of combined PLC and medial structures. Therefore, it was still not able to exclude the contributing effect of the concomitant medial side injuries on the diagnosis of PLC injuries by the LGDT test. Despite that, we recommended to use the LGDT test cautiously in patients with combined PLC and medial side injuries. In addition, the number of specimen was relatively small in quantifying the increased mean ETRA. Alternatively, we performed five measurements on each of the sectioned state and recorded the mean values as the final results to minimize the accidental errors within the study.
Conclusion
In this cadaveric sequential sectioning study, the LGDT test showed positive merely at the following two situations: (1) the distal POP-T and PFL were both sectioned; (2) the posteromedial structures (sMCL, deep MCL and POL) and the cruciate ligaments (ACL and PCL) were all sectioned.
References
Lunden JB, Bzdusek PJ, Monson JK, Malcomson KW, Laprade RF (2010) Current concepts in the recognition and treatment of posterolateral corner injuries of the knee. J Orthop Sports Phys Ther 40(8):502–516
Levy BA, Stuart MJ, Whelan DB (2010) Posterolateral instability of the knee: evaluation, treatment, results. Sports Med Arthrosc 18(4):254–262
Laprade RF, Griffith CJ, Coobs BR, Geeslin AG, Johansen S, Engebretsen L (2014) Improving outcomes for posterolateral knee injuries. J Orthop Res 32(4):485–491
Levy BA, Boyd JL, Stuart MJ (2011) Surgical treatment of acute and chronic anterior and posterior cruciate ligament and lateral side injuries of the knee. Sports Med Arthrosc 19(2):110–119
Lee HJ, Park YB, Ko YB, Kim SH, Kwon HB, Yu DS et al (2014) The necessity of clinical application of tibial reduction for detection of underestimated posterolateral rotatory instability in combined posterior cruciate ligament and posterolateral corner deficient knee. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3138-7
Feng H, Hong L, Geng XS, Zhang H, Wang XS, Zhang J (2009) Posterolateral sling reconstruction of the popliteus tendon: an all-arthroscopic technique. Arthroscopy 25(7):800–805
Zhang H, Feng H, Hong L, Wang XS, Zhang J (2009) Popliteofibular ligament reconstruction for posterolateral external rotation instability of the knee. Knee Surg Sports Traumatol Arthrosc 17(9):1070–1077
Zhang J, Feng H, Hong L, Wang XS, Zhang H (2011) “Floating popliteus tendon injury” in a multiple-ligament knee injury: one case report and arthroscopy-assisted reconstruction. Chin Med J (Engl) 124(23):4099–4101
Zhang H, Hong L, Wang XS, Zhang J, Liu X, Feng H (2011) All-arthroscopic repair of arcuate avulsion fracture with suture anchor. Arthroscopy 27(5):728–734
Feng H, Zhang H, Hong L, Wang XS, Zhang J (2009) The “lateral gutter drive-through” sign: an arthroscopic indicator of acute femoral avulsion of the popliteus tendon in knee joints. Arthroscopy 25(12):1496–1499
Feng H, Zhang H, Hong L, Wang XS, Cheng KB, Zhang J (2011) Femoral peel-off lesions in acute posterolateral corner injuries: incidence, classification, and clinical characteristics. Arthroscopy 27(7):951–958
Shen J, Zhang H, Lv Y, Hong L, Wang X, Zhang J et al (2013) Validity of a novel arthroscopic test to diagnose posterolateral rotational instability of the knee joint: the lateral gutter drive-through test. Arthroscopy 29(4):695–700
Griffith CJ, LaPrade RF, Johansen S, Armitage B, Wijdicks C, Engebretsen L (2009) Medial knee injury: part 1, static function of the individual components of the main medial knee structures. Am J Sports Med 37(9):1762–1770
LaPrade RF, Bollom TS, Wentorf FA, Wills NJ, Meister K (2005) Mechanical properties of the posterolateral structures of the knee. Am J Sports Med 33(9):1386–1391
Zhang H, Zhang J, Liu X, Shen JW, Hong L, Wang XS et al (2013) In vitro comparison of popliteus tendon and popliteofibular ligament reconstruction in an external rotation injury model of the knee: a cadaveric study evaluated by a navigation system. Am J Sports Med 41(9):2136–2142
Conflict of interest
One or more of the authors (JWS) have received funding from the National Natural Science Foundation of China (81101397).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feng, H., Song, Gy., Shen, Jw. et al. The “lateral gutter drive-through” sign revisited: a cadaveric study exploring its real mechanism based on the individual posterolateral structure of knee joints. Arch Orthop Trauma Surg 134, 1745–1751 (2014). https://doi.org/10.1007/s00402-014-2100-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2100-y