Abstract
Study design
Retrospective review of prospectively collected data.
Objective
To investigate the incidence of hip dislocation 90 days after total hip arthroplasty in relation to time after surgery, mechanism of dislocation and predisposing factors.
Methods
Prospective data on preoperative patient characteristics from six Danish arthroplasty departments with similar fast-track approaches were cross-referenced with the Danish National Patient Registry for complete 90-day follow-up on readmissions, including emergency-room contacts. Complete patient files and postoperative radiographs were reviewed in case of dislocations. Unadjusted comparisons were made using t test/Chi-square analyses, while evaluation of risk factors potentially predisposing to dislocations was done using uni- and multivariate regression analysis.
Results
A total of 2,734 consecutive unselected procedures were available for analysis, of which 65 (2.4 %) had dislocations. Of these, eight were during index admission and five were treated and discharged from the emergency room. Mechanisms of dislocation were most often movement while supine or sitting for the first 30 days and due to squatting/bending from day 31 to 90. The 65 patients with dislocations had suboptimal cup placement in 34 (52.3 %), and a femoral head size of <36 mm in 20 (30.8 %) cases. Predisposing factors of dislocation were age ≥75 [OR:1.96 (1.18–3.38)], pharmacologically treated psychiatric disease [OR:2.37 (1.29–4.36)] and department of surgery [OR:2.27 (1.31–3.40)] but not hospital stay of <4 days. Departments with recommendations for activity restrictions had fewer dislocations than a department without restrictions.
Conclusions
Patients ≥75 years and with pharmacologically treated psychiatric disease may be at increased risk of dislocations after fast-track total hip arthroplasty. Further studies including detailed information on patient and prosthesis characteristics, and activity restrictions are needed to reduce the risk of dislocation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip dislocation (HD) is one of the most common “surgical” complications after total hip arthroplasty (THA), and accounts for 12–22 % of all reoperations after primary THA in Scandinavia [1–3]. The risk of HD is thought to be influenced by surgical factors, e.g. surgical approach [4–6] and femoral head size [2, 4, 7], as well as patient characteristics such as age and various comorbidities [4, 8–10]. However, most studies on HD are based on large national registers [2, 4] with limited information on perioperative treatment and patient comorbidity as well as potential incomplete registration on dislocations treated with reduction in the emergency room, or single-centre studies with limited sample sizes [11–13] and long study periods [5, 14]. Thus, detailed interpretation regarding pathogenic mechanisms and preventive strategies is problematic. This may be especially important considering the implementation of enhanced perioperative care protocols, so called “fast-track” surgery, which has resulted in enhanced recovery with decreased postoperative morbidity and consequently reduced length of hospital stay (LOS) [15, 16]. Early mobilization is a cornerstone in fast-track surgery [15, 17], but could potentially influence the rate of early HD as patients are both mobilized and returning to a higher level of activity earlier. Also, the reduction in LOS has led to concerns about a potential increase in fatal complications occurring after discharge [18] and although general morbidity has been reduced [19–21] there is limited knowledge about specific aspects of patient safety in fast-track THA.
The objectives of the present hypothesis generating observational study were (1) to report the incidence, timing and mechanisms of HD during the first 90 days after surgery, (2) to investigate patient-related factors potentially disposing to HD, and (3) to describe head size, cup placement and postoperative restriction guidelines in the patients who had HD.
Patients and methods
All patients having elective unilateral fast-track THA in six centres participating in the Lundbeck Centre for Fast-track Hip and Knee Replacement Collaboration database (LCDB) between Jan 1st 2010 and Dec 1st 2011 were included in this study. Patients were excluded in case of age <18, no Danish social security number, other major joint arthroplasty or orthopaedic surgery on the lower extremity <3 months previously and THA planned as non-elective procedure (Fig. 1) [20]. The present study is based on a study registry intended for studies of patient-related risk factors and safety outcomes after THA and TKA and registered on ClinicalTrials.org (ID: NCT01515670). All participating centres are “high volume” centres performing >250 procedures yearly with a median LOS of 2–3 days. The posterolateral approach was used in all patients, while choice of prosthesis components was at the discretion of the attending surgeon. Cemented or uncemented concepts were used according to the usual practice of the departments. The centres all have a similar standardized fast-track perioperative setup, including spinal anaesthesia, fluid plans, multimodal opioid-sparing analgesia, early mobilization and standardized discharge criteria with discharge to own home [22]. General postoperative restrictions for the first 3 months were used as the standard in five of six departments (no flexion of the hip beyond 90°, no leg crossing, no internal rotation, and mandatory use of aids (e.g. elevated toilet)).
The LCDB includes preoperative information on patient-related factors such as living alone/with others and medical comorbidity. These data are prospectively collected using a patient-reported questionnaire with staff available for clarifications and are subsequently entered in the LCDB which has a data completeness of >95 % [20]. Data on psychiatric disease were further validated using the Danish National Database on Reimbursed Prescriptions which records any prescription with reimbursement dispensed at any Danish pharmacy [23]. Information on LOS, readmissions and emergency-room contacts within 90 days postoperatively, and mortality was registered through the DNPR, hereby assuring complete follow-up [24]. LOS was calculated as number of postoperative nights spent in hospital until discharge, including transferrals between wards. A LOS of >4 days was considered as “prolonged” admission and the discharge papers were investigated to determine the cause. In patients with HD the entire medical record was reviewed to verify and determine the mechanism of HD. All readmissions and emergency-room contacts were investigated to determine potential relation to surgery, as described in a previous study including some of the present procedures [20]. Readmissions were calculated on a “per procedure” basis with only readmissions considered surgery-related and with overnight stay in hospital being included. In case of HD details on the index surgical procedure and prosthesis components as well as the entire medical record of the admission were reviewed to elucidate the mechanisms of HD. In case of multiple HD only the first occurrence was evaluated. We also reviewed the medical records of any patient with possible HD unmentioned in the discharge papers (falls and other reoperations) to avoid overlooking any HD.
Patients identified as having HD had their early postoperative and post-dislocation radiographs reviewed by two senior orthopaedic consultants specialized in THA (SS and PKA). Cup placement was deemed “sub-optimal” (SOP) if outside 36–60° inclination in the anterior–posterior plane and/or without anteversion in the lateral plane, defined as a position of the cup more retroverted than the optimal 10–15° of anteversion [25]. Cups with anteversion of more than 15° were also deemed suboptimal. No attempt to judge the position (ante- or retroversion) of femoral component was performed. Radiographs were evaluated using “clinical judgement” as no standardization of radiographs between departments had been possible due to the retrospective nature of this study, and no specific radiographic evaluation tools were available (i.e. Martell Hip Analysis Suite).
Statistical analysis
Data were evaluated for normality distribution using Kolomogorov–Smirnoff test. For continuous non-parametric data Mann–Whitney U test was used and Chi-square and Fishers exact test were used for comparisons of proportions. In case of multiple group-comparisons’ proportions we used z test with Bonferroni correction for proportions and Kruskall–Wallis test for continuous data. In analyses of risk factors of HD the following variables were investigated with unadjusted logistic regression analysis: age ≥75 years, female gender, obesity (BMI > 30) and >2 units of alcohol/day. These were chosen based on previous association with HD [9, 26, 27]. Additionally, we investigated preoperative use of walking aid, and pharmacologically treated psychiatric disease, department of surgery and LOS >4 days. For analysis between-department differences, we initially did unadjusted analysis of all departments using the department with fewest HD as reference. Then, we dichotomized departments into those with significantly more HD than the reference department vs. the remaining departments and redid the unadjusted analysis. A significance level of ≤0.25 was used in the unadjusted analysis to avoid excluding potential relevant variables. Finally we constructed a multiple logistic regression model using backwards stepwise multiple regression [28]. We tested the effect of LOS <4 days (excluding HD during primary admission to avoid bias) in an adjusted multivariate analysis regardless of unadjusted results, as this was a study outcome. Results are given as odds ratios (OR) with 95 % confidence intervals (CI) and a significance level of p ≤ 0.05.
Results
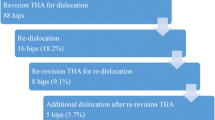
A total of 2,734 primary elective unilateral THA were included. The median LOS was 2 days (IQR: 2–3) with a 6.7 % 90 days readmission rate and 0.2 % surgically related mortality (Table 1). We found 65 (2.4 %) procedures with one or more HD ≤90 days after surgery [median time to HD: 16 days (IQR: 7–47.5)], of which 43 (66.2 %) were ≤30 days (Fig. 2). Multiple HD occurred after 17 procedures.
In 57 (87.7 %) of the HD patients the indication for THA was osteoarthritis, while four were due to previous hip fractures (6.2 %) and two (3.1 %) due to femoral head necrosis or hip dysplasia, respectively. Median age of patients with HD was 70 years (63-79) with 55.4 % women and a median LOS of 3 days (IQR: 2–4) (Table 1). Seven patients were revised ≤90 days due to HD (0.26 % of all patients), of which five had ≥2 displacements. In eight (12.3 %) patients HD occurred during index hospitalization, while 52 (80.0 %) were after discharge with admission to a regular ward and 5 (7.7 %) were after discharge with reduction and subsequent discharge from the ER.
Details of mechanisms of HD were found in the medical records in 62/65 HD. These were divided into five groups: falls (13/62), “in bed” (inappropriate movement) (13/62), “sitting” (sitting/rising from chair/toilet) (18/62), bending/squatting (15/62) and related to “suboptimal” positioning of patients immediately after surgery (3/62). Eleven of the 15 HD due to bending/squatting occurred more than 30 days after surgery, in contrast to HD due to falls (4/13), “in bed” (2/13) and “sitting” (5/18) (p < 0.01). We found an overall difference in median time to HD between groups (p = 0.003), specifically according to whether HD was due to bending/squatting (day 57 (IQR: 25–68) days after surgery) compared to in “in bed” [day 7 (IQR: 8–24.5); p = 0.002] or “sitting” [day 13 (IQR: 6.5–31); p = 0.003]. HD due to falls occurred, median day 14 (IQR: 5.5–54); and not different from the “bending/squatting” group (p = 0.128), the three HDs with no information on mechanisms all occurred ≤30 days after surgery (Fig. 3).
Femoral head size in HD was <36 mm in 20/65, and 13/43 of HD ≤30 days after surgery had femoral head size <36 mm, not different from femoral head size ≥36 mm (OR: 1.08 CI: 0.36–3.26 p = 0.896). Neither was there any difference in median time to dislocation according to femoral head size [19 (IQR: 4–50) vs. 16 days (IQR: 7–47.5) p = 0.696; respectively].
Review of the postoperative radiographs in HD revealed SOP in 34/65. HD ≤30 days after surgery was not more frequent in patients with SOP (24/43; OR: 1.52 CI: 0.54–4.26, p = 0.429), and with no difference in median time to dislocation [16.5 days (IQR: 6.5–41.5) vs. 15 days (IQR: 7–55), respectively, p = 0.550]. Neither was the risk of multiple dislocations increased in patients with SOP (6/34 vs. 11/31, OR: 0.39, CI: 0.12–1.23; p = 0.102). SOP was found in 5/15 of the “bending/squatting” group, 10/13 of the “in bed” group, 8/18 of the “sitting/raising” group, 7/13 of those with falls and 2/3 with HD due to “suboptimal” layering. The differences in fraction of procedures with SOP were only statistically significant between the “in bed” and the bending/squatting” groups (p = 0.021).
The rate of HD was increased in department 6 (4.2 % CI: 2.7–6.4) compared to the rest (2.0 % CI: 1.5–2.7, p = 0.005) (Table 2). However, in department 6 the proportion of patients living alone (40.7 vs. 31.7 % p < 0.001) and with alcohol use >2 units/day (10.8 vs. 6.6 % p = 0.003) was significantly higher compared to the other departments. Also, smaller heads were more common in the patients with HD (45.0 vs. 24.4 %) (Table 2).
Unadjusted analysis of patient characteristics found age ≥75 years, preoperative use of walking aids, psychiatric disease and department of surgery to be associated with HD at a significance level of <0.25. LOS ≤ 4 days was not associated with an increased risk of HD in either unadjusted or adjusted analyses (Table 3). In the stepwise multiple regression analysis, preoperative use of walking aids ceased to be associated with HD after adjusting for age and psychiatric disease, and consequently the variables included in the final adjusted analysis were age ≥75 years, pharmacologically treated psychiatric disease and department of surgery (Table 3).
Discussion
It is generally agreed that HD is due to multiple factors, such as surgical technique, choice of prosthesis, and patient-related factors, while the influence of postoperative activity restrictions is debateable [29]. This detailed prospective study on HD in 2,734 fast-track primary THA demonstrated HD in 2.4 % of procedures at 90-day follow-up in line with previous reports [30–32]. There were different circumstances leading to HD in the early and the late postoperative period, with HD due to “bending/squatting” occurring later than those related to being “in bed” or “sitting”. This is not surprising as the patients improve mobility and spend less time being supine or sitting.
We have previously found that falls within 30 days of surgery often result in severe complications such as HD or fractures [10]. The present study is in accordance with this, as two-thirds of HD due to falls are ≤30 days after surgery. This implies that future strategies for prevention of HD should consider preventive strategies for early falls [10].
Increased age was, as previously described [27], a risk factor for HD and likely related to decreased muscle control/strength and increased risk of falling in the elderly [8, 10]. Pharmacologically treated psychiatric disease also increased the risk of HD. This has not been described previously and deserves further investigation, although potentially related to increased risk of falling in elderly patients with depression, regardless of psychotropic treatment [33].
SOP has previously been associated with HD [31, 34] and we found that more than 50 % of HD patients had SOP. The interpretation of this finding however is difficult, as no comparison with patients without HD was performed, and a previous study has found an accuracy of about 50 % to place the cup in the safe zone in all patients—regardless of subsequent HD or not [35]. Furthermore, definitions and equipment for measuring cup “safe zones” differ [25, 36], and evaluation of radiographs may benefit from advanced digital analyses [37]. In the present retrospective study we had to evaluate non-standardized radiographs obtained from different departments which induce a risk of misinterpretation. However, this is how positioning of prosthetic implants is evaluated in daily clinical practice, and thus our results reflect “real life” clinical evaluation. Nonetheless, given the mentioned limitations, we can only conclude that careful attention to cup placement should be included in future studies.
We did not find an increased number of 30-day HD with smaller femoral head size, although about one-third of patients with HD had a femoral head size of <36 mm. Previous studies have found a beneficial effect of larger femoral heads [2, 4, 5], and our study is limited by no data on femoral head size in patients without HD. Thus, further controlled large-scale studies including data on SOP and femoral head size as well as patient characteristics are needed to determine the role of these factors on HD after fast-track THA.
No effect of postoperative restrictions when using an anterolateral approach has been found [29], but this has not been investigated when using a posterior approach, as in our study. A recent non-randomized study on 365 patients from another Danish department using both a fast-track protocol and a posterior approach found a non-significant increase in number of HD (2.7 vs. 1.3 %) in the 219 patients with no postoperative activity restrictions [38]. In our study, we found an increased risk of HD in the one department without postoperative restrictions compared to the remaining five departments. We believe that our observations together with those of Mikkelsen et al. call for further studies on the potential role of restrictions for HD; preferably with details on type of restriction regimen, patient information and compliance.
There are difficulties when comparing the dislocation rate in our study with previous reports, as we focused on the immediate postoperative period (90 days) and included all HD, including those being treated in the emergency room. Most national registers report only HD being treated by surgical procedures with change of components [1–3], and the dislocation rates reported from the registers are probably too low. The HD rate in our study is comparable to a previous single-centre study with a fast-track setup from one of the participating departments [32] and to what was found by Biedermann and colleagues (2005) (≈2.2 % for primary THA) within 1 year. Although having a longer follow-up period, 119/137 HD occurred within the first 12 weeks which is similar to our follow-up period [31]. Another study found 1.1 % HD within 1 year, but with 75 % of HD occurring within the first 3 months and using an anterolateral surgical approach [14]. However, both studies only included HD treated at their own facility, thus potentially having incomplete registration. The strength of our study is a complete 90-day follow-up through the DNPR, hereby ensuring that all admissions (both hospitalizations and ER visits, regardless of location) within 90 days are captured [24]. This is in contrast to previous studies which only include admissions to the hospital of primary surgery [14, 31, 39]. Furthermore, we investigated the medical charts of all admissions, regardless of diagnosis codes, hereby further ensuring that no HDs were overlooked.
The weaknesses of our study were the lack of detailed registration of patient compliance to restrictions, retrospective analysis of radiographs and no information on the femoral head size in patients without HD. Finally, the analyses need to be considered in relation to the relatively few HD, thus potentially limiting the study power. On the other hand, we had a large study cohort with prospective recording of comorbidities and complete follow-up through the DNPR and medical files, thus enabling detailed information on preoperative patient characteristics and limiting the risk of overlooking any HD.
Conclusion
The risk of HD was about 2.5 % within 90 days after fast-track THA and related to age ≥75 years and pharmacologically treated psychiatric disease, but not to LOS ≤ 4 days. The roles of postoperative activity restrictions, suboptimal cup placement and femoral head size need further investigation. Multimodal preventive strategies should include attention to the different mechanisms causing HD before and after 30 days postoperatively.
References
The Danish Hip Arthroplasty Registry (2013) Danish Hip Arthroplasty Registry, annual report 2013. http://www.dhr.dk/Ny%20mappe/rapporter/DHR%20årsrapport%202013_full%20versionfinal_.pdf. Accessed 13 Nov 2013
Kostensalo I, Junnila M, Virolainen P, Remes V, Matilainen M, Vahlberg T, Pulkkinen P, Eskelinen A, Makela KT (2013) Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: a population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register. Acta Orthop 84:342–347
The Swedish Hip Arthroplasty Registry (2012) Swedish Hip Arthroplasty Register, annual report 2011. http://www.shpr.se/Files/Årsrapport%202011%20(eng)%20webb.pdf. Accessed 13 Nov 2013
Hailer NP, Weiss RJ, Stark A, Karrholm J (2012) The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. An analysis of 78,098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop 83:442–448
Berry DJ, Von KM, Schleck CD, Harmsen WS (2005) Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am 87:2456–2463
Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ (2006) Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res 447:34–38
Howie DW, Holubowycz OT, Middleton R (2012) Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 94:1095–1102
Patel PD, Potts A, Froimson MI (2007) The dislocating hip arthroplasty: prevention and treatment. J Arthroplasty 22:86–90
Brooks PJ (2013) Dislocation following total hip replacement: causes and cures. Bone Joint J 95-B(11 Suppl A):67–69
Jorgensen CC, Kehlet H (2013) Fall-related admissions after fast-track total hip and knee arthroplasty—cause of concern or consequence of success? Clin Interv Aging 8:1569–1577
Lachiewicz PF, Soileau ES (2006) Dislocation of primary total hip arthroplasty with 36 and 40-mm femoral heads. Clin Orthop Relat Res 453:153–155
Lachiewicz PF, Soileau ES (2013) Low early and late dislocation rates with 36- and 40-mm heads in patients at high risk for dislocation. Clin Orthop Relat Res 471:439–443
Chiu FY, Chen CM, Chung TY, Lo WH, Chen TH (2000) The effect of posterior capsulorrhaphy in primary total hip arthroplasty: a prospective randomized study. J Arthroplasty 15:194–199
Leichtle UG, Leichtle CI, Taslaci F, Reize P, Wunschel M (2013) Dislocation after total hip arthroplasty: risk factors and treatment options. Acta Orthop Traumatol Turc 47:96–103
Kehlet H (2013) Fast-track hip and knee arthroplasty. Lancet 381:1600–1602
Husted H (2012) Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop Suppl 83:1–39
Ansari D, Gianotti L, Schroder J, Andersson R (2013) Fast-track surgery: procedure-specific aspects and future direction. Langenbecks Arch Surg 398:29–37
Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH (2007) Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am 89:27–32
Malviya A, Martin K, Harper I, Muller SD, Emmerson KP, Partington PF, Reed MR (2011) Enhanced recovery program for hip and knee replacement reduces death rate. Acta Orthop 82:577–581
Jorgensen CC, Kehlet H (2013) Role of patient characteristics for fast-track hip and knee arthroplasty. Br J Anaesth 110:972–980
den Hartog YM, Mathijssen NM, Vehmeijer SB (2013) Reduced length of hospital stay after the introduction of a rapid recovery protocol for primary THA procedures. Acta Orthop 84:444–447
Husted H, Solgaard S, Hansen TB, Soballe K, Kehlet H (2010) Care principles at four fast-track arthroplasty departments in Denmark. Dan Med Bull 57(7):A4166
Johannesdottir SA, Horváth-Puhó E, Schmidt M, Ehrenstein V, Pedersen L, Sørensen HT (2012) Existing data sources for clinical epidemiology: the Danish National Database of Reimbursed Prescriptions. Clin Epidemiol 4:1–11
Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH (1999) The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 46:263–268
Dorr LD, Wan Z (1998) Causes of and treatment protocol for instability of total hip replacement. Clin Orthop Relat Res 355:144–151
Plate JF, Seyler TM, Stroh DA, Issa K, Akbar M, Mont MA (2012) Risk of dislocation using large- vs. small-diameter femoral heads in total hip arthroplasty. BMC Res Notes 5:553
Lachiewicz PF, Soileau ES (2002) Stability of total hip arthroplasty in patients 75 years or older. Clin Orthop Relat Res 405:65–69
Hosmer DW, Lemenshow S (eds) (2000) Applied logistic regression. John Wiley & Sons, New York
Sharma V, Morgan PM, Cheng EY (2009) Factors influencing early rehabilitation after THA: a systematic review. Clin Orthop Relat Res 467:1400–1411
Phillips CB, Barrett JA, Losina E, Mahomed NN, Lingard EA, Guadagnoli E, Baron JA, Harris WH, Poss R, Katz JN (2003) Incidence rates of dislocation, pulmonary embolism, and deep infection during the first 6 months after elective total hip replacement. J Bone Joint Surg Am 85-A(1):20–26
Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B (2005) Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br 87:762–769
Husted H, Otte KS, Kristensen BB, Orsnes T, Kehlet H (2010) Readmissions after fast-track hip and knee arthroplasty. Arch Orthop Trauma Surg 130:1185–1191
Darowski A, Chambers SA, Chambers DJ (2009) Antidepressants and falls in the elderly. Drugs Aging 26:381–394
He RX, Yan SG, Wu LD, Wang XH, Dai XS (2007) Position of the prosthesis and the incidence of dislocation following total hip replacement. Chin Med J Eng 120:1140–1144
Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H (2011) The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res 469:319–329
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60:217–220
Choi HR, Anderson D, Foster S, Beal M, Lee JA, Barr C, Malchau H, McCarthy J, Kwon YM (2013) Acetabular cup positioning in revision total hip arthroplasty with Paprosky type III acetabular defects: martell radiographic analysis. Int Orthop 37:1905–1910
Mikkelsen LR, Petersen MK, Soballe K, Mikkelsen S, Mechlenburg I (2014) Does reduced movement restrictions and use of assistive devices affect rehabilitation outcome after total hip replacement? A non-randomized, controlled study. Eur J Phys Rehabil Med [Epub ahead of print]
Goldstein WM, Gleason TF, Kopplin M, Branson JJ (2001) Prevalence of dislocation after total hip arthroplasty through a posterolateral approach with partial capsulotomy and capsulorrhaphy. J Bone Joint Surg Am 83-A Suppl 2:2–7
Conflict of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative Group are given in the Appendix.
Appendix: Members of the Lundbeck Foundation Centre for Fast-track Hip and Knee replacement
Appendix: Members of the Lundbeck Foundation Centre for Fast-track Hip and Knee replacement
Henrik Husted, Orthopedic Department, Hvidovre, Denmark.
Kjeld Soeballe, Department of Orthopedics, Aarhus, Denmark.
Lars T. Hansen, MD, Orthopedic Department, Grindsted, Denmark.
Mogens B. Laursen, Orthopedic Division, Aalborg, Denmark.
Torben B. Hansen, Department of Orthopedics, Holstebro, Denmark.
Rights and permissions
About this article
Cite this article
Jørgensen, C.C., Kjaersgaard-Andersen, P., Solgaard, S. et al. Hip dislocations after 2,734 elective unilateral fast-track total hip arthroplasties: incidence, circumstances and predisposing factors. Arch Orthop Trauma Surg 134, 1615–1622 (2014). https://doi.org/10.1007/s00402-014-2051-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2051-3