Abstract
Introduction
Congenital dislocation of the patella and recurrent symptomatic dislocation in adolescents are difficult pathologies to treat. Stanisavljevic described an extensive release procedure essentially involving medializing the entire lateral quadriceps and medial soft tissue stabilization. There are no significant series reporting the success of this method. This procedure has been performed in our institution over several years and we report our results.
Method
Retrospective case series. Between 1990 and 2007, 20 knees in 13 children and adolescents (mean age 12.8 years; 4–17, 7 female) with recurrent or congenital dislocation of the patella (8 knees) underwent this procedure after failed conservative treatment (mean follow-up 7.5 years; 4–16). All were immobilized in a long leg cast for 6 weeks.
Results
Five knees in five patients (20 %, 1 congenital dislocation) reported their knees as improved without further dislocations. Out of the 15 knees with failures (80 %) 12 in six patients (60 %) were revised due to redislocation. Three knees in two patients (15 %) still had dislocations or subluxations, but any revision was refused. Three knees in three patients caused pain and discomfort during daily activity. Redislocation first developed after a mean of 21.3 months (4–72) postoperatively. Only one patient had returned to sport at the 12-month follow-up.
Discussion
The Stanisavljevic procedure produces a mediocre success rate with our long-term follow-up series showing a failure rate up to 80 %. We therefore recommend more specific procedures dealing with the anatomical deformity such as trochleaplasty to produce superior success rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patello-femoral instability represents a difficult problem to treat both conservatively and operatively, and there is no general consensus in the literature as to the best management [1]. The incidence of patella dislocation ranges from 6 per 100,000 in the adult population to 43 per 100,000 in the pediatric population [2]. Recurrent symptomatic subluxation and dislocation of the patella occurs commonly in adolescents who are otherwise well, but also in patients with predisposing diagnoses such as ligamentous laxity, muscular hypotonia or Down syndrome [3]. Various surgical procedures have been described to manage patello-femoral instability, but none has proven superior or is universally accepted [4].
The pathomechanisms of patello-femoral instability are complex and multifactorial, including the osseous anatomy of the entire femur, in both torsion and trochlea shape, the rotation of the tibia, ligamentous stability of the medial and posterolateral knee, and the shape and relative position of the patella itself. However, even if the pathology includes an osseous component, osteotomies must not be performed in skeletally immature patients, which places soft tissue balancing in the center of attention.
One of the most commonly used terms in patello-femoral disorders is the Q-angle, consisting of the patella at the vertex and an upper ray to the anterior superior iliac spine and a lower ray to the tibial tuberosity. Early treatment options of patello-femoral instability included primarily distal realignment procedures aiming at correction of the Q-angle. The oldest procedures known include the tubercle transfer suggested by Roux in 1887 or soft tissue realignment by transfer of the lateral half of the patellar tendon to the pes anserine as suggested by Goldthwait. However, the clinical effect of these procedures aiming at the lower ray of the Q-angle is limited and modifications and improvements were sought after. Lateral release and medial plication are being used to improve the effect of distal realignment procedures by correcting both the lower ray and the vertex of the Q-angle, but their clinical impact is still lacking [1].
In 1976, Stanko Stanisavljevic described an extensive soft tissue procedure, which addresses the lower ray, vertex and upper ray of the Q-angle by combining a patella tendon transfer with a lateral release and medial plication and an extensive, subperiosteal medialization of the entire lateral quadriceps [5]. While the theory behind this procedure is at least interesting and trigonometrically plausible, there have been no clinical series to systematically study the outcome of this method. The aim of this study is to determine whether the Stanisavljevic procedure is able to achieve patellar stability in long term in a cohort of 20 skeletally immature patients.
Methods
Study design
This study was designed as a retrospective cohort of skeletally immature patients undergoing the Stanisavljevic procedure for patello-femoral instability. The local ethics committee approved the protocol. All identified patients were available for follow-up with an effective attrition rate of 0 %.
We retrospectively reviewed all patients who had undergone the Stanisavljevic procedure between 1990 and 2007. The case records of all patients were reviewed. All patients were clinically examined by a board-certified orthopedic surgeon with a pediatric specialization on an individual basis and any level of persisting patellar instability after the Stanisavljevic procedure was assessed and documented.
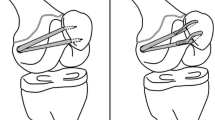
Surgical procedure (see Fig. 1a–g)
In all cases, the operation and postoperative rehabilitation were performed according to the original description by Stanisavljevic [5]:
Operative description for the Stanisavljevic procedure (details see “Methods”). a Skin incision; b excision of fascia lata; c elevation of vastus lateralis with periosteum; d suturing of periosteum more medially to the femur; e splitting of patella tendon; f placing patella tendon as far medially as possible; g drawing the capsule laterally over patella
A skin incision is made from ~4 cm below the greater trochanter, extending on the lateral aspect of the thigh, curving superiorly over the lateral femoral condyle and finishing medially four to five cm below the medial condyle (Fig. 1a). The lateral, anterior and medial aspects of the knee including the pes anserine are exposed. A strip of fascia lata is excised and the lateral septum is identified (Fig. 1b). The vastus lateralis is elevated off the septum in its entirety from the lateral septum and the periosteum on the lateral aspect of the femur is visualized. The periosteum is incised down to bone just anterior to the lateral septum. The knee capsule is incised laterally to the patella and along the lateral edge of the patellar tendon to the tibial tuberosity. Using sharp periosteal elevators, all of the quadriceps is subperiosteally elevated, rotated medially and the periosteum is sutured to the bone as medial as possible (Fig. 1c, d). The patella tendon is also split and the lateral half is divided distally and placed under the medial portion of the tendon and then sutured as far medially as possible on the tibia in the region of the tibial attachment of the medial collateral ligament (Fig. 1e, f). This part of the procedure is similar to that described by Goldthwait [6].
A medial parapatellar incision of the capsule is also made and the patella is delivered medially under this capsule and sutured medially (Fig. 1g). The capsule is drawn laterally over the patella and sutured to the lateral edge of the patella securing its reduction. The gap on the lateral aspect of the knee is then covered by the fascia lata, which was excised earlier.
Postoperatively, a long leg cast is applied with the knee flexed 5°–10° for 6 weeks. After cast removal, physical therapy with active and passive range-of-motion exercises of the knee is initiated.
Outcome assessment
The knee evaluation consisted of subjective assessment (pain, patellar stability, overall activity level) and objective measures (recurrence of patellar dislocation and radiographic assessment including sulcus angle and patella height by the Caton–Deschamps index), and complaints referable to sports activity. Patients operated bilaterally were asked to rate each affected knee separately. All further patella realignment surgeries were recorded. Additional diagnoses associated with hyperlaxity and joint instability e.g., Down syndrome were specifically noted.
Statistical evaluation
Quantitative continuous data were tested for normality using the Kolmorogov/Smirnov statistic and no transformation was needed. Outcomes are reported as mean ± SD with the 95 % confidence interval (95 % CI) [7]. Binary data (stability yes/no, recurrence yes/no) are given as percentage with 95 % CI. Data collection and statistical analysis were done with intercooled Stata 11 (StataCorp LP, College Station, TX).
Results
Patient demographics
Between 1990 and 2007, a total of 20 knees (10 right, 10 left) in 13 patients (7 females and 6 males, mean age 12.8 years, range [4–17] ) with symptomatic recurrent (12 knees) or congenital dislocation (8 knees) of the patella were treated. All patients had been subjected to a prolonged period of conservative treatment which had failed. Eight knees in five patients had congenital permanent dislocations of patella. Follow-up was a mean of 7.5 years (range 4–16 years). Two patients had prior procedures to the knee, namely a femoral and tibial osteotomy bilaterally prior to the Stanisavljevic procedure for a congenital patellar dislocation, the second a lateral release and a medial plication. In two knees, the Stanisavljevic procedure was combined with an Elmslie-Trillat operation [8], one with a femoral osteotomy for correction of valgus.
Subjective assessment
Five knees in five patients (20 %) were reported as improved or much improved. Two patients in this group still complained of patello-femoral pain during high-demand sporting activities such as football or skiing. One further patient in this group complained of a subjective feeling of instability although no true subluxations or dislocations of the patella occurred.
Clinical assessment
15 knees in eight patients (80 %) had further dislocations after the Stanisavljevic procedure after a mean of 21.3 months (range 4–72 months). All these patients described their operated knee as the same as before or worse after the Stanisavljevic procedure. Twelve of these knees in six patients underwent revision procedures, usually trochleaplasty and/or additional soft tissue procedures such as the Insall procedure or the Emslie Trillat [8, 9]. Three more knees in two patients still continued to have patellar dislocation or subluxation, but declined any further surgical intervention. Three knees in three patients in the failed group also complained of pain and discomfort during activities of daily living in addition to the instability. All knees had congenital dislocation but one (seven knees in four patients) had again dislocations of patella after a mean of 24 months (4–72). Six knees out of eight knees in five patients with an underlying diagnosis relevant to hyperlaxity and joint instability (trisomy and hypotone cerebral palsy) had further dislocations.
Radiographic assessment
The postoperative assessment at maximum follow-up revealed an interesting trend to patella bacha deformities. The mean Caton–Deschamps index was 0.85 ± 0.15 (95 % CI 0.78–0.93), i.e., in the low or low-normal range. The mean sulcus angle was 158° ± 5° (95 % 148°–167°). Given the high rate of recurrent dislocation, measurement of the congruence angle was not attempted.
Table 1 demonstrates the demographic details and underlying diagnoses, if present, in the successful and failed groups, respectively.
Discussion
Stanko Stanisavljevic in 1976 described a surgical procedure to treat congenital, irreducible, permanent lateral dislocation of the patella. He reported success using this procedure in six cases at 2 years of follow-up [5]. While this procedure or similar ones (lateral release, medial plication) are widely used, there are no large long-term series in the literature reporting the results of this most extensive lateral release method.
Marumo described the use of the Stanisavljevic procedure for patellar instability in one patient with nail–patella syndrome combined with a medial translocation of the tibial tuberosity [10]. Relative success was described in terms of re-alignment of the quadriceps but the patient had a significant extensor lag of 30° due to lengthening of the extensor mechanism. It is important to note that this was of a combination of procedures and not a Stanisavljevic alone. Ceynowa described a case where the procedure was done in a 4-month-old with Rubinstein–Taybi syndrome with success [11]. Other authors have suggested that successful results were obtained when the operation was performed in younger children [12]. They commented that other procedures, such as the semitendinosus tenodesis or tendon transfer, should be combined to achieve better patellar stability with flexion in older children. Many of these studies are limited by the short-term follow-up (<2 years) and our study clearly demonstrates that failure with further subluxations can occur at a late stage. Indeed, one patient did not ‘fail’ until 6 years after the index procedure [13, 14]. As most of these patients are skeletally immature at diagnosis, it is imperative that follow-up continues until growth is finished as the natural history of the condition could well come to light again with growth.
We describe the largest series to date of 20 knees in 13 patients with a mean follow-up of over 7.5 years. We widened the indication for the Stanisavljevic procedure to beyond congenital patellar dislocation as it is well known that more limited procedures such as the lateral release alone have an extremely high failure rate [15]. However, even with extensive soft tissue realignment like the Stanisavljevic procedure, the failure rate is still as high as 80 %. Radiographical assessment revealed only slight trochlea dysplasia with a mean sulcus angle of 158° ± 5°, however, there was a concerning trend to patella bacha deformity.
The large majority of these patients underwent further surgical interventions and the remaining were left with a significant morbidity related to the knee. While many of the patients in the failed group had additional diagnoses with a higher risk of joint instability, many had simple idiopathic patellar instability that also went on to failure of the procedure.
The original procedure was recommended for the treatment of irreducible congenital patellar dislocation, but in our series only one of the five patients with this diagnosis had a successful outcome in the long term with redislocation occurring at an average of 24 months. Green described success in a series of four patients with congenital dislocation of the patella using a very similar procedure to that described by Stanisavljevic [12]. He suggests that treatment at an early age is important for a successful outcome and indeed recommends surgery prior to the age of 1 year. This theory is borne out by our results where the only successful reduction of a congenital dislocation had the procedure at the age of 4 years and was up to 9 years follow-up with no symptoms. The other congenitally dislocated patella in our series had the surgery in their teens and all failed.
Gordon and Schoenecker described a soft tissue procedure for patellar instability again similar to that of Stanisavljevic. Importantly, however, this was also combined with a tibial tuberosity transfer in the skeletally mature and full patellar tendon transfer in the skeletally immature [16]. With this approach, a reasonable success rate was obtained with one redislocation in 17 knees. They emphasized the importance of fully understanding the pathological anatomy of the condition in each patient and with early surgical intervention, addressing each of these pathologies in turn.
It is well known that patellar dislocation in Down’s syndrome (trisomy 21) is a difficult problem to deal with [3] and again our series shows a high failure rate in this patient group with two knees out of seven having a successful outcome with the Stanisavljevic procedure. This demonstrates that a soft tissue procedure, even as extensive as the Stanisavljevic, will likely eventually succumb to the pathological process, namely ligamentous laxity associated with Downs. A bony procedure such a trochleaplasty or Elmslie is likely to give more reliable success rates, but the limitation of skeletal maturity has to be adhered to when considering such interventions [9, 17, 18]. But even the combination of Stanisavljevic with an Elmslie procedure could not prevent the dislocation.
In reviewing the results of this procedure over the long term, the depressing reality of patellar instability and the difficulty of this condition to treat were all too evident. We think that the Stanisavljevic procedure, which essentially describes an extensive lateral release combined with a medial ‘tightening’, is unreliable when performed alone. Where possible early intervention should be contemplated and indeed in congenital dislocations or ligamentous laxity diseases this should be at as young an age if possible, essentially at the point of diagnosis. In these the procedure as described by Green is likely to be of benefit. We have also seen some early success with the reconstruction of the medial patello-femoral ligament in cases of traumatic or idiopathic patello-femoral instability [19, 20]. If early intervention is not possible and symptoms have become long standing, then we believe it is necessary to add a bony procedure usually in the form of a trochleaplasty to secure stability [21, 22]. The patient should have reached or almost reached skeletal maturity to undergo such an intervention. Clearly, to support these theories, long-term follow-up of these interventions is required and we will report on this in due course.
References
Vavken P, Wimmer MD, Camathias C, Quidde J (2013) Treating patella instability in skeletally immature patients. Arthroscopy 29(8):1410–1422
Nietosvaara Y, Paukku R, Palmu S, Donell ST (2009) Acute patellar dislocation in children and adolescents. Surgical technique. J Bone Jt Surg 91:139–145. doi:10.2106/JBJS.H.01289
Bettuzzi C, Lampasi M, Magnani M, Donzelli O (2008) Surgical treatment of patellar dislocation in children with Down syndrome: a 3- to 11-year follow-up study. Knee Surg Sports Traumatol Arthrosc 17:334–340. doi:10.1007/s00167-008-0652-5
Lim AKS, Chang HC, Hui JHP (2008) Recurrent patellar dislocation: reappraising our approach to surgery. Ann Acad Med Singap 37:320–323
Stanisavljevic S, Zemenick G, Miller D (1976) Congenital, irreducible, permanent lateral dislocation of the patella. Clin Orthop Relat Res 116:190–199
Goldthwait JE (1903) Slipping or recurrent dislocation of the patella. With the report of eleven cases. Am J Orthop Surg 1:293–308
Vavken P, Heinrich KM, Koppelhuber C et al (2009) The use of confidence intervals in reporting orthopaedic research findings. Clin Orthop Relat Res 467(12):3334–3339. doi:10.1007/s11999-009-0817-7
Cox JS (1982) Evaluation of the Roux-Elmslie-Trillat procedure for knee extensor realignment. Am J Sports Med 10:303–310
Trillat A, Dejour H, Couette A (1964) Diagnosis and treatment of recurrent dislocations of the patella. Rev Chir Orthop Réparatrice Appar Mot 50:813–824
Marumo K, Fujii K, Tanaka T, Takeuchi H (1999) Surgical management of congenital permanent dislocation of the patella in nail patella syndrome by Stanisavljevic procedure. J Orthop Sci 4(6):446–449
Ceynowa M, Mazurek T (2009) Congenital patella dislocation in a child with Rubinstein-Taybi syndrome. J Pediatr Orthop B 18:47–50. doi:10.1097/BPB.0b013e3283157ef8
Green JP, Waugh W, Wood H (1968) Congenital lateral dislocation of the patella. J Bone Jt Surg Br 50:285–289
Joo SY, Park KB, Kim BR et al (2007) The “four-in-one” procedure for habitual dislocation of the patella in children: early results in patients with severe generalised ligamentous laxity and aplasis of the trochlear groove. J Bone Jt Surg Br 89:1645–1649. doi:10.1302/0301-620X.89B12.19398
Letts RM, Davidson D, Beaule P (1999) Semitendinosus tenodesis for repair of recurrent dislocation of the patella in children. J Pediatr Orthop 19:742–747
Muhr G, Knopp W, Neumann K (1989) Dislocation and subluxation of the patella. Orthopade 18:294–301
Gordon JE, Schoenecker PL (1999) Surgical treatment of congenital dislocation of the patella. J Pediatr Orthop 19:260–264
Shelbourne KD, Porter DA, Rozzi W (1994) Use of a modified Elmslie-Trillat procedure to improve abnormal patellar congruence angle. Am J Sports Med 22:318–323
Endres S, Wilke A (2011) A 10 year follow-up study after Roux-Elmslie-Trillat treatment for cases of patellar instability. BMC Musculoskelet Disord 12:48. doi:10.1186/1471-2474-12-48
Shea KG, Nilsson K, Belzer J (2006) Patellar dislocation in skeletally immature athletes. Oper Tech Sports Med 14:188–196
Nomura E, Inoue M (2003) Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy 19:E47. doi:10.1053/jars.2003.50167
Dejour H, Walch G, Neyret P, Adeleine P (1990) Dysplasia of the femoral trochlea. Rev Chir Orthop Réparatrice Appar Mot 76:45–54
von Knoch F, Böhm T, Bürgi ML et al (2006) Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Jt Surg Br 88:1331–1335. doi:10.1302/0301-620X.88B10.17834
Conflict of interest
There are no conflicts of interests in all authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Camathias, C., Rutz, E., Götze, M. et al. Poor outcome at 7.5 years after Stanisavljevic quadriceps transposition for patello-femoral instability. Arch Orthop Trauma Surg 134, 473–478 (2014). https://doi.org/10.1007/s00402-014-1947-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-1947-2