Abstract
Introduction
Conventional cementless total hip arthroplasty already shows very good clinical results. Nevertheless, implant revision is often accompanied by massive bone loss. The new shorter GTS™ stem has been introduced to conserve femoral bone stock. However, no long-term clinical results were available for this implant. A biomechanical comparison of the GTS™ stem with the clinically well-established CLS® stem was therefore preformed to investigate the targeted stem philosophy.
Materials and methods
Four GTS™ stems and four CLS® stems were implanted in a standardized manner in eight synthetic femurs. A high-precision measuring device was used to determine micromotions of the stem and bone during different load applications. Calculation of relative micromotions at the bone–implant interface allowed the rotational implant stability and the bending behavior of the stem to be determined.
Results
Lowest relative micromotions were detected near the lesser trochanter within the proximal part of both stems. Maximum relative micromotions were measured near the distal tip of the stems, indicating a proximal fixation of both stems. For the varus–valgus–torque application, a comparable stem bending behavior was shown for both stems.
Conclusion
Both stems seem to provide a comparable and adequate primary stability. The shortened GTS™ design has a comparable rotational stability and bone–implant flexibility compared to a conventional stem. This study demonstrates that the CLS® stem and the GTS™ stem exhibit similar biomechanical behavior. However, a clinical confirmation of these experimental results is still required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conventional cementless total hip arthroplasty (THA) already shows very good clinical results [1–3]. However, patients are getting younger and more active and so increasing demands are being placed on the implant. As implant revision surgery is a complex procedure, methods to enhance long-term survival and simplify revision were further developed (e.g., changing from cemented to cementless fixation) [4]. Shorter primary hip stems were also developed to prevent the loss of bone stock. However, the shorter stem design may include a change in the implant–bone fixation [5], an important factor for the long-term success of the implant [6, 7].
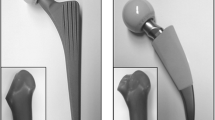
One of these shorter implants is the cementless GTS™ stem (Biomet GmbH, Berlin, Germany) (Fig. 1a). The manufacturer promotes the stem as a tissue- and bone-sparing system [8]. The GTS™ stem design is based on the three-dimensional tapered stem philosophy, similar to the cementless CLS® stem (Zimmer GmbH, Winterthur, Switzerland) (Fig. 1b). Compaction of the bone combined with the tapered body and longitudinal fins along the entire length of the implant should mainly provide a proximal fixation and avoid a distal cortical canal fit and fill. The reduced implant length and reduced lateral shoulder should support the option of minimal invasive surgery.
However, no long-term clinical results are available for this new implant design. A long-term fixation is based on osseointegration of the implant over time and requires an adequate initial implant fixation (primary stability) during surgery [7]. Obviously, osseointegration can hardly be studied in vitro. However, the initial implant–bone fixation can be biomechanically measured. We have already characterized and compared the initial fixation pattern of multiple implant designs in vitro [9–11]. Clinical observations (e.g., bone remodeling or radiographic implant fit) confirmed the results of our experimental studies [9, 12, 13].
Therefore, the promoted objectives of the GTS™ stem should be biomechanically validated with regards to the initial implant stability and bending behavior of the implanted stem. A comparison of the GTS™ stem to the clinically well-established CLS® stem should demonstrate whether the targeted stem philosophy is similar. Determination of the specific implant stability and the bending behavior of the stems can provide answers to questions like: is the initial fixation (in terms of low micromotions) adequate for an osseointegration, is a proximal fixation achieved or does the reduced length have an effect on stem-to-bone flexibility?
Materials and methods
Four GTS™ standard femoral stems (Offset 133°, size +3) and four CLS® stems (Offset 125°, size 12.5) were implanted by an experienced surgeon in a standardized manner in eight synthetic femurs [composite bone 4th generation (size large, left #3406), Sawbones® Europe, Malmö, Sweden] after femoral neck resection. Both implants were made out of a titanium-based alloy with similar material properties (GTS™: titanium 6-aluminum 4-vanadium according to ISO 5832-3 and CLS®: titanium 6-aluminum 7-niobium according to ISO 5832-11). To imitate the in vivo achieved press fit during hip surgery [14], a material testing device (Frank-Universalprüfmaschine 81816/B, Karl Frank GmbH, Weinheim-Birkenau, Germany) was used that applied standardized cyclic loads of 25 × 2 kN followed by 25 × 4 kN. The loads were applied with an impaction speed of 2.5 mm/min. These utilities and methods reduced implantation variability and served as a basis for a comparative measurement. Radiography and post-measuring dye test proofed implant fit and sizing.
The stem–bone compound was mounted in a well-established implant stability-measuring device [9–11]. Linear actuators were used to apply forces at the lever arm (Fig. 2). A rope system was used to reduce counteractions and to allow the implant–bone compound to define its own axis of rotation. The lever arm was adapted to the implant and the bone was fixed distally. Two different cyclic load situations were applied, based on different load situations occurring on the hip stem in vivo during normal daily activities: (a) Axial torque of ±7 Nm around the longitudinal stem axis to determine the rotational implant stability (Fig. 3a). (b) Varus–valgus–torque of ±3.5 Nm to determine the bending behavior of the stem (Fig. 3b). Bending behavior of the stem in relation to bending of the bone could influence stress distribution at the bone (Fig. 4). Applied loads were downscaled from maximum occurring in vivo load situations [15] to enable non-destructive testing.
A two-parted cube system was attached to the implant proximally and to each separate measuring point (Fig. 2). Six linear variable differential transformers (LVDT, Type P2010, Mahr GmbH, Göttingen, Germany) were used to measure the micromotions of the stem (measuring points #1 and #2) and of the bone (#0 and #3–5) at different sites (Fig. 5). The LVDTs were arranged in a 3-2-1 configuration to determine the three-dimensional motion of each measuring point [9–11] (Fig. 2). Comparing the motions at different sites during axial torque application allowed the calculation of relative micromotions at the bone–implant interface so that conclusions about rotational implant stability could be drawn. Comparing the absolute micromotions of the stem at different sites (measuring points #1 and #2) referred to trochanter minor during varus–valgus–torque application with respect to their magnitude and direction (medial or lateral) allowed the calculation of the specific implant flexibility so that conclusions about the bending behavior of the stem could be drawn. A factor for bending behavior was defined as \( f = m_{\text{p}} + m_{\text{d}} . \) With f: value of flexibility; m p: measured micromotion at the proximal end of the implant; m d: measured micromotion at the distal end of the implant. More detailed formulas and method descriptions could be found in Nägerl et al. [16] and Görtz et al. [9].
Statistics
Data were expressed as mean ± standard deviation (SD). Based on previous studies [9–11] and the highly standardized materials and methods, an amount of n = 4 tests per implant was chosen. The main fixation of both implants was characterized and these were compared to each other with analyses of variance. A “least significant difference” test (LSD) was calculated as a post hoc test. The flexibility of both implants was calculated and compared with a Student’s t test. All statistical tests were two-tailed, and a p value <0.05 was considered significant. SPSS® version 20.0 (SPSS Inc., Chicago, IL, USA) was used for statistical data analysis.
Results
Rotational torque around the stem axis: rotational primary stability
In Fig. 6, the micromotions are compared for both designs during rotational torque application. In relation to the absolute motions of the implant (continuous line) and the bone (dashed line), relative micromotions at the implant–bone interface were displayed with arrows at each specific site (proximal stem shoulder, trochanter minor and distal tip of the stem) along the longitudinal axis of the implant.
No significant differences were observed with respect to the fixation characteristic of both stems (p = 0.76). Lowest relative micromotions were detected near the lesser trochanter within the proximal part of both stems (GTS™ 8.00 ± 0.95 mdeg/Nm vs. CLS® 6.49 ± 0.87 mdeg/Nm; p = 0.26). Largest relative micromotions were measured close to the distal tip of the stem for both designs (GTS™ 12.88 ± 0.89 mdeg/Nm vs. CLS® 12.32 ± 3.68 mdeg/Nm; p = 0.67).
However, significant differences were observed for the measuring sites of each separate stem. The micromotions at the distal tip of the stem of both designs differed compared to all other measuring points (GTS™ distal vs. proximal p < 0.01, vs. minor p < 0.01; CLS® distal vs. proximal p < 0.01, vs. minor p < 0.01) indicating a proximal fixation of both stems.
Varus–valgus–torque: bending behavior of the stem
In Fig. 7, the micromotions are compared for both designs during varus–valgus–torque application. The measured directions of micromotions at the proximal stem shoulder and the distal stem tip characterized the bending behavior of the stems. Similar to the CLS®, proximal and distal motions of the GTS™ stem were directed medially. Both stems seemed to behave flexibly, following the motion of the bone instead of a more rigid like ‘tilting’. However, no difference in flexibility (magnitude) between the two types of stem was found (GTS™ 0.60 ± 0.59 mdeg/Nm vs. CLS® 0.95 ± 0.31 mdeg/Nm; p = 0.35).
Discussion
We were aware of some limitations of this study. Most of them refer to the debate on fundamental principles of combining a standardized comparable in vitro test and clinical practice in vivo. We tried to conclude on secondary stability influences based on primary stability measurements. Comparable in vivo tests including osseointegration were almost impossible. Although human specimens would reflect the in vivo behavior of the femur in a better way, synthetic bones were known to offer a standardized way of measuring and comparing different implants. Although higher sample sizes were desirable, a sample size of n = 4 appeared to be sufficient based on the experience of previous studies [9–11] and the standardization of materials and methods. Current results of the CLS® stem were comparable to former measurements, even though a past generation of synthetic bones was used [9], proving the high standardization of these measurements. However, an 100 % standardization was impossible due to the human factor within rasping. Another limiting point was the offset angle difference of the implants. Even though Fottner et al. [17] denied an influence of different offsets on primary stability using physiological loading conditions in case of the CLS®, an impact of different offsets in our study is unknown. The presence of drilling holes on the one side and the low number of implant measuring points on the other side is another study limitation. Past measurements showed that an increased number of drilling holes and measuring points did not improve the results. Drilling holes are essential to have an access to the implant surface, although they are weakening the bone. The chosen number of drilling holes and measurement points is, therefore, a compromise between these two aspects and is based on our experience in previous studies [9–11]. The inclusion of bone flexibility within the implant–bone interface micromotions is another study limitation. However, this seemed to have a minor influence on the results. In vitro observed implant behavior, measured with this method [9] has been verified clinically (e.g., CLS [2] and Alloclassic [3]).
Despite the current trend towards cementless hip arthroplasty [18], implant fixation is a crucial factor in THA. A physiological force transmission from the implant to the bone with low micromotions is essential for osseous secondary fixation for a satisfactory long-term survival of the implant to be achieved [7]. Quantity and quality of the remaining bone stock influence the surgeon’s choice for the type of implant, e.g., short stem, conventional stem or revision stem. However, each single implant has its own characteristic fixation behavior, which could be classified and compared to other implants [9, 19]. Obviously extended bone defects are accompanied by revision and tumor systems that fixate distally in the diaphyseal cortical bone. However, smaller bone defect situations with intact metaphyseal parts enable a proximally supported fixation. Conventional cementless primary hip stems often combine a metaphyseal and diaphyseal fit, although the specific fixation characteristic might change depending on implant geometry [19]. Both proximal fixation (e.g., CLS® stem; e.g., 94 % survival rate after 12 years [2]) and distal fixation (e.g., Zimmer Alloclassic® stem; e.g., 98 % survival rate after 15 years [3]) might result in good long-term survival. However, a “non-physiological” distal load transfer might result in problems such as thigh pain [20] or stress shielding [5, 21], which might lead to loosening of the stem followed by implant revision [22]. The short-stem philosophy has now been introduced, aimed at avoiding stress shielding and conserving proximal bone stock by proximal metaphyseal load transfer. Chechik et al. [18] reported about a growing interest on the use of minimal invasive approaches within a survey of current trends and common practices in THA.
The targeted proximal fixation of the new shortened GTS™ stem in the proximal femoral diaphysis could be confirmed in this experimental study. Compared to short stems, the mainly proximal fixation was additionally distal guided by diaphyseal cortical contact. These results are further supported by excellent first clinical results with a survival rate of 100 % at a follow-up of 16 months [23]. However, these are only early results that still have to be confirmed.
With reference to previous studies [9–11], the low relative micromotions of both groups seem to indicate an adequate primary stability of the stems. The GTS™ stem and the CLS® stem both revealed a proximally located main fixation of the stem, confirming the promoted fixation characteristic. Based on our results, the proximal fixation may be assigned to different reasons: compaction of the bone, the tapered body or the longitudinal fins. The GTS™ stem has fins along the entire length of the stem, unlike the CLS® stem with fins only in the proximal part of the stem. This might indicate a lower importance of the longitudinal fins in the distal region of the GTS™ stem. Compaction of the bone or the three-dimensional tapered design might be more important for proximal fixation. With regards to the increased micromotions in the distal part of the stems, the aim of avoiding a distal cortical canal fit and fill seems to be confirmed. The shortened GTS™ design appears to have a comparable rotational stability compared to a conventional stem. Also the stem elasticity during varus–valgus–torque application was comparable. Both stems seem to follow the bending of the bone instead of ‘tilting’ within the femur.
Several studies focused on implant fixation of shorter or short-stem designs. However, as different methods were used, the comparison of these results is limited and a global statement on implant fixation is difficult to be drawn. Depending on study type (e.g., bone density analysis [24], migration measurement with roentgen stereometry analysis [25], loosening determination with vibrational techniques [26, 27], finite element modeling [28, 29], cortical stress measurement with strain gauges [30] or measurement of interface motions [31–33], fixation characteristics have been determined. Assumed interactions between, e.g., interface motions, fixation characteristic or bone reaction help to draw conclusions (e.g., low distal interface motions > distal diaphyseal fixation or distal cortical hypertrophy > proximal stress shielding > proximal atrophy). Kress et al. [24] reported about decrease of proximal metaphyseal bone density after 7 years follow-up of the C.F.P. stem. The promoted metaphyseal fixation of this short stem seemed to turn out to be at least partly diaphyseal fixating similar to the measured GTS™ stem. One out of 49 stems had to be revised due to aseptic loosening. Santori et al. [5] observed 50 % proximal bone resorption and 15 % distal cortical hypertrophy within a mean of 8 years follow-up after implantation of a short-stem design in 131 cases. These findings might include a partly diaphyseal fixation as well. However, no stem had to be revised. Fottner et al. [34] concluded on high risks for stress shielding for the biomechanically tested short stems, Metha and Mayo. Clinically, the Mayo stem revealed good mid-term outcome (e.g., 97.5 % survivorship after a mean of 4.7 years [35]. Bieger et al. [36] experimentally compared the short Mayo stem, the shortened Fitmore™ stem and the standard CLS® stem regarding primary stability and strain distribution. They concluded the short stem not to be inferior regarding primary stability. In addition, the shortened Fitmore™ design seemed to reveal a lower tendency of stress shielding. However, distal cortical hypertrophies were observed clinically after implantation of the shortened Fitmore™ design [37]. Westphal et al. [31] revealed lower micromotions of the tested Proxima™ short stem compared to two conventional stems. Early clinical results reported of an increased bone density 1 year after surgery [38], as well as of a decreased bone density after mean follow-up of 1.7 years [39] with this short-stem design. However, long-term survival of these short stems and shorter conventional stems is not well supported.
To conclude, this study demonstrated that the CLS® stem and the GTS™ stem exhibit similar biomechanical behavior. However, a clinical confirmation of these experimental results is still required.
References
Garellick G, Kaerrholm J, Rogmark C, Rolfson O, Herberts P (2012) Swedish hip arthroplasty register: annual report 2011
Streit M, Schröder K, Körber M, Merle C, Gotterbarm T, Ewerbeck V, Aldinger P (2012) High survival in young patients using a second generation uncemented total hip replacement. Int Orthop (SICOT) 36(6):1129–1136. doi:10.1007/s00264-011-1399-z
Suckel A, Geiger F, Kinzl L, Wulker N, Garbrecht M (2009) Long-term results for the uncemented zweymuller/alloclassic hip endoprosthesis: a 15-year minimum follow-up of 320 hip operations. J Arthroplasty 24(6):846–853. doi:10.1016/j.arth.2008.03.021
Troelsen A, Malchau E, Sillesen N, Malchau H (2013) A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res 471(7):2052–2059. doi:10.1007/s11999-013-2941-7
Santori FS, Santori N (2010) Mid-term results of a custom-made short proximal loading femoral component. J Bone Joint Surg 92B(9):1231–1237. doi:10.1302/0301-620x.92b9.24605
Steinhauser E (2006) Biomechanische Grundlagen der Implantatverankerung. In: Ossäre integration. Springer, Heidelberg, pp 16–23. doi:10.1007/978-3-540-35687-5_2
Bensmann G (1999) Cementless fixation of endoprostheses. Biomed Eng 35(s3):44–47. doi:10.1515/bmte.1990.35.s3.44
Biomet (2012) GTS (global tissue sparring) femoral hip system. GTS brochure
Gortz W, Nagerl UV, Nagerl H, Thomsen M (2002) Spatial micromovements of uncemented femoral components after torsional loads. J Biomech Eng Trans Asme 124(6):706–713. doi:10.1115/1.1517565
Jakubowitz E, Bitsch RG, Heisel C, Lee C, Kretzer JP, Thomsen MN (2008) Primary rotational stability of cylindrical and conical revision hip stems as a function of femoral bone defects: an in vitro comparison. J Biomech 41(14):3078–3084. doi:10.1016/j.jbiomech.2008.06.002
Jakubowitz E, Kinkel S, Nadorf J, Heisel C, Kretzer JP, Thomsen MN (2011) The effect of multifilaments and monofilaments on cementless femoral revision hip components: an experimental study. Clin Biomech 26(3):257–261. doi:10.1016/j.clinbiomech.2010.11.004
Dohle J, Becker W, Braun M (2001) Radiologische Analyse der ossären Integration nach Implantation der Alloclassic-Zweymüller-Hüft-TEP (Radiological analysis of osseointegration after implantation of the zweymüller-alloclassic total hip system). Z Orthop Ihre Grenzgeb 319(06):517–524. doi:10.1055/s-2001-19234
Brodner W, Bitzan P, Lomoschitz F, Krepler P, Jankovsky R, Lehr S, Kainberger F, Gottsauner-Wolf F (2004) Changes in bone mineral density in the proximal femur after cementless total hip arthroplasty: a five-year longitudinal study. J Bone Joint Surg, Br 86B(1):20–26. doi:10.1302/0301-620x.86b1.14637
Schmidbauer U, Brendel T, Kunze KG, Nietert M, Ecke H (1993) Dynamische Kräftemessung bei der Implantation von Total-Endoprothesen des Hüftgelenkes (Dynamic force measurement in implantation of total endoprostheses of the hip joint). Unfallchirurgie 19(1):11–15. doi:10.1007/bf02588222
Bergmann G, Graichen F, Rohlmann A (1993) Hip joint loading during walking and running, measured in two patients. J Biomech 26(8):969–990. doi:10.1016/0021-9290(93)90058-M
Nägerl H, Kubein-Meesenburg D, Schäfer W, Cotta H, Thomsen M, Strachwitz B, Fanghänel J (1996) Messung der räumlichen Mikrobewegung des Femurschaftes von Endoprothesen in Abhängigkeit des räumlichen Kraftsystems (Measurement of the spatial micromovement of hip endoprostheses as a function of the spatial force system. a pilot study). Z Orthop Unfall 134(02):99–110. doi:10.1055/s-2008-1039780
Fottner A, Peter CV, Schmidutz F, Wanke-Jellinek L, Schröder C, Mazoochian F, Jansson V (2011) Biomechanical evaluation of different offset versions of a cementless hip prosthesis by 3-dimensional measurement of micromotions. Clin Biomech 26(8):830–835. doi:10.1016/j.clinbiomech.2011.04.001
Chechik O, Khashan M, Lador R, Salai M, Amar E (2013) Surgical approach and prosthesis fixation in hip arthroplasty world wide. Arch Orthop Trauma Surg 133(11):1595–1600. doi:10.1007/s00402-013-1828-0
Khanuja HS, Vakil JJ, Goddard MS, Mont MA (2011) Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg 93(5):500–509. doi:10.2106/jbjs.j.00774
Cinotti G, Della Rocca A, Sessa P, Ripani FR, Giannicola G (2013) Thigh pain, subsidence and survival using a short cementless femoral stem with pure metaphyseal fixation at minimum 9-year follow-up. Orthop Traumatol Surg Res 99(1):30–36. doi:10.1016/j.otsr.2012.09.016
Huiskes R, Weinans H, Vanrietbergen B (1992) The relationship between stress shielding and bone-resorption around total hip stems and effects of flexible materials. Clin Orthop Relat Res 274:124–134
Prokopetz J, Losina E, Bliss R, Wright J, Baron J, Katz J (2012) Risk factors for revision of primary total hip arthroplasty: a systematic review. BMC Musculoskelet Disord 13(1):251
Morales de Cano J, Gordo C, Illobre J (2013) Early clinical results of a new conservative hip stem. Eur J Orthop Surg Traumatol 1–5. doi:10.1007/s00590-013-1198-x
Kress A, Schmidt R, Nowak T, Nowak M, Haeberle L, Forst R, Mueller L (2012) Stress-related femoral cortical and cancellous bone density loss after collum femoris preserving uncemented total hip arthroplasty: a prospective 7-year follow-up with quantitative computed tomography. Arch Orthop Trauma Surg 132(8):1111–1119. doi:10.1007/s00402-012-1537-0
Karrholm J, Borssen B, Lowenhielm G, Snorrason F (1994) Does early micromotion of femoral stem prostheses matter? 4–7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg 76B(6):912–917
Kim S-J, Kim M-R, Rim J-S, Chung S-M, Shin S-W (2010) Comparison of implant stability after different implant surface treatments in dog bone. J Appl Oral Sci 18:415–420
Rieger JS, Jaeger S, Schuld C, Kretzer JP, Bitsch RG (2013) A vibrational technique for diagnosing loosened total hip endoprostheses: an experimental sawbone study. Med Eng Phys 35(3):329–337. doi:10.1016/j.medengphy.2012.05.007
Abdul-Kadir MR, Hansen U, Klabunde R, Lucas D, Amis A (2008) Finite element modelling of primary hip stem stability: the effect of interference fit. J Biomech 41(3):587–594. doi:10.1016/j.jbiomech.2007.10.009
Pettersen SH, Wik TS, Skallerud B (2009) Subject specific finite element analysis of implant stability for a cementless femoral stem. Clin Biomech 24(6):480–487. doi:10.1016/j.clinbiomech.2009.03.009
Umeda N, Saito M, Sugano N, Ohzono K, Nishii T, Sakai T, Yoshikawa H, Ikeda D, Murakami A (2003) Correlation between femoral neck version and strain on the femur after insertion of femoral prosthesis. J Orthop Sci 8(3):381–386. doi:10.1007/s10776-002-0635-2
Westphal FM, Bishop N, Honl M, Hille E, Püschel K, Morlock MM (2006) Migration and cyclic motion of a new short-stemmed hip prosthesis: a biomechanical in vitro study. Clin Biomech 21(8):834–840. doi:10.1016/j.clinbiomech.2006.04.004
Decking J, Gerber A, Kränzlein J, Meurer A, Böhm B, Plitz W (2004) Die Primärstabilität von manuell und roboterassistiert implantierten Hüftendoprothesenstielen: eine biomechanische Untersuchung an Kunstfemora (A biomechanical study on the initial stability of thr stems after manual and robot-assisted implantation in synthetic femora). Z Orthop Ihre Grenzgeb 12(03):309–313. doi:10.1055/s-2004-822794
Østbyhaug PO, Klaksvik J, Romundstad P, Aamodt A (2010) Primary stability of custom and anatomical uncemented femoral stems: a method for three-dimensional in vitro measurement of implant stability. Clin Biomech 25(4):318–324. doi:10.1016/j.clinbiomech.2009.12.012
Fottner A, Schmid M, Birkenmaier C, Mazoochian F, Plitz W, Volkmar J (2009) Biomechanical evaluation of two types of short-stemmed hip prostheses compared to the trust plate prosthesis by three-dimensional measurement of micromotions. Clin Biomech 24(5):429–434. doi:10.1016/j.clinbiomech.2009.02.007
Falez F, Casella F, Panegrossi G, Favetti F, Barresi C (2008) Perspectives on metaphyseal conservative stems. J Orthopaed Traumatol 9(1):49–54. doi:10.1007/s10195-008-0105-4
Bieger R, Ignatius A, Decking R, Claes L, Reichel H, Dürselen L (2012) Primary stability and strain distribution of cementless hip stems as a function of implant design. Clin Biomech 27(2):158–164. doi:10.1016/j.clinbiomech.2011.08.004
Gustke K (2012) Short stems for total hip arthroplasty: Initial experience with the Fitmore™ stem. J Bone Joint Surg 94B(11 suppl A):47–51. doi:10.1302/0301-620x.94b11.30677
Logroscino G, Ciriello V, DŒAntonio E (2011) Bone integration of new stemless hip implants (proxima vs. nanos). A DXA study: preliminary results. Int J Immunopathol Pharmacol 24:113–116
Ghera S, Pavan L (2009) The DePuy Proxima hip: a short stem for total hip arthroplasty. Early experience and technical considerations. Hip Int 19(3):215–220
Conflict of interest
This work was performed at the Laboratory of Biomechanics and Implant Research, Department of Orthopedics and Traumatology, University Hospital Heidelberg, Heidelberg, Germany. The work was partly funded through Biomet GmbH. The funding party had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors have declared that no competing interests exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nadorf, J., Thomsen, M., Gantz, S. et al. Fixation of the shorter cementless GTS™ stem: biomechanical comparison between a conventional and an innovative implant design. Arch Orthop Trauma Surg 134, 719–726 (2014). https://doi.org/10.1007/s00402-014-1946-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-1946-3