Abstract
Purpose
To present the technique of free-hand subaxial cervical pedicle screw (CPS) placement without using intra-operative navigating devices, and to investigate the crucial factors for safe placement and avoidance of lateral pedicle wall perforation, by measuring and classifying perforations with postoperative computed tomography (CT) scan.
Summary of background data
The placement of CPS has generally been considered as technically demanding and associated with considerable lateral wall perforation rate. For surgeons without access to navigation systems, experience of safe free-hand technique for subaxial CPS placement is especially valuable.
Materials and methods
A total of 214 consecutive traumatic or degenerative patients with 1,024 CPS placement using the free-hand technique were enrolled. In the operative process, the lateral mass surface was decorticated. Then a small curette was used to identify the pedicle entrance by touching the cortical bone of the medial pedicle wall. It was crucial to keep the transverse angle and make appropriate adjustment with guidance of the resistance of the thick medial cortical bone. The hand drill should be redirected once soft tissue breach was palpated by a slim ball-tip prober. With proper trajectory, tapping, repeated palpation, the 26–30 mm screw could be placed. After the procedure, the transverse angle of CPS trajectory was measured, and perforation of the lateral wall was classified by CT scan: grade 1, perforation of pedicle wall by screw placement, with the external edge of screw deviating out of the lateral pedicle wall equal to or less than 2 mm and grade 2, critical perforation of pedicle wall by screw placement, large than 2 mm.
Results
A total of 129 screws (12.64 %) were demonstrated as lateral pedicle wall perforation, of which 101 screws (9.86 %) were classified as grade 1, whereas 28 screws (2.73 %) as grade 2. Among the segments involved, C3 showed an obviously higher perforating rate than other (P < 0.05). The difference between the anatomical pedicle transverse angle and the screw trajectory angle was higher in patients of grade 2 perforation than the others. In the 28 screws of grade 2 perforation verified by axial CT, 26 screws had been palpated as abnormal during operation. However, only 19 out of the 101 screws of grade 1 perforation had shown palpation alarming signs during operation. The average follow-up was 36.8 months (range 5–65 months). There was no symptom and sign of neurovascular injuries. Two screws (0.20 %) were broken, and one screw (0.10 %) loosen.
Conclusion
Placement of screw through a correct trajectory may lead to grade 1 perforation, which suggests transversal expansion and breakage of the thinner lateral cortex, probably caused by mismatching of the diameter of 3.5 mm screws and the tiny cancellous bone cavity of pedicle. Grade 1 perforation is deemed as relatively safe to the vertebral artery. Grade 2 perforation means obvious deviation of the trajectory angle of hand drill, which directly penetrates into the transverse foramen, and the risk of vertebral artery injury (VAI) or development of thrombi caused by the irregular blood flow would be much greater compared to grade 1 perforation. Moreover, there are two crucial maneuvers for increasing accuracy of screw placement: identifying the precise entry point using a curette or hand drill to touch the true entrance of the canal after decortication, and guiding CPS trajectory on axial plane by the resistant of thick medial wall.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the cervical pedicle screw (CPS) can provide more reliable biomechanical stability than the lateral mass screw or transarticular screw [1, 2], the CPS system has been increasingly and widely accepted by surgeons for the treatment of a variety of unstable cervical spine conditions [3]. The subaxial CPS can be used to effectively treat traumatic and nontraumatic conditions as well as kyphosis correction and destructive spondyloarthropathy, as it allows for shorter instrumentation with improved spinal alignment [4].
CPS placement is generally considered to be technically demanding. The pedicle is much smaller in the cervical spine than in the thoracic or lumbar spine, and the anatomy varies between individuals. The reported rate of pedicle wall perforation with CPS placement varies from 3.7 to 21 % [3, 5, 6], with lateral wall perforation being the most common. To increase the accuracy of CPS placement, intra-operative image assistant techniques were recommended [7]. However, CPS malposition causing vertebral artery injury (VAI) or neurological complications has also been reported even when using navigation system [8]. Moreover, for surgeons without access to navigation systems, experience of safe free-hand technique (particularly regarding the axial trajectory of the cervical pedicle) for subaxial CPS placement is especially valuable. Such experience is particularly beneficial when reliable stabilization anchors are needed, such as in deformity correction or posterior revision procedures.
Postoperative axial CT scan to assess the accuracy of pedicle screw placement is widespread. Several studies have detected perforations after CPS placement using CT scans, and researchers tended to grade the breaches by referring the screw diameter, to acquire precise and convenient evaluations [9, 10]. However, the relationship between different grades of perforation and the risk of VAI has not been clarified.
The purpose of this study was to present our method of free-hand subaxial CPS placement technique which does not use intra-operative navigation device, and to investigate the crucial factors for safe placement and avoidance of lateral pedicle wall perforation, by measuring and classifying perforations using postoperative computed tomography (CT) scans.
Materials and methods
Patient data
This study involved 214 consecutive patients who had undergone C3–C7 CPS placement (with all together 1,024 screws) by a single surgeon (Jingming Xie) using the free-hand technique from July 2004 to July 2009 (detailed in Table 1). The average age of the patients was 47.7 years (range 9–73 years). Pedicle morphology was fully evaluated preoperatively by radiographs and reconstructed CT scans. The angles of each pedicle trajectory on the axial plane were measured. Pedicles with a diameter of less than 3.5 mm were excluded from this study.
Neurological and vascular complications were assessed though preoperative, immediate postoperative, and the final follow-up physical examination and clinical notes. Instrumentation and bone union status at the final follow-up were reviewed using radiographs and CT scans.
Surgical technique
Patients were placed on a prone position under general anesthesia. Intra-operative fluoroscopy was used only for locating the relevant vertebrae, or for showing sagittal alignment of the cervical spine, if necessary. A long straight posterior midline incision was made between the spinous processes of C2 and C7. The vertebrae being planned to insert screws were identified and the lateral masses were exposed until reached to their lateral margins. The cortex of the lateral mass on the lateral and superior quadrant was partly removed with a high-speed burr. Then an osseous hole of 3.5 mm depth was created. We used a small curette to gently scrape off the cancellous bone through the bottom of the hole and towards the interior side, until the cortical bone of the medial pedicle wall was touched. Our method for identifying the pedicle entrance was similar to Karaikovic reported “funnel technique” [11]. In some cases, the screw insertion point was directly observable at the bottom of the osseous hole, as a round area of cancellous bone surrounded by solid cortical bone. After that, a 2-mm hand drill was put into the track to probe the cortical resistance again.
The hand drill was held at a transverse angle of approximately 35–45° (not solely dependent on the data measured for each pedicle on the CT scan) and was gradually drilled deeper using a smooth rotational motion. The trajectory of the CPS track on the axial plane was guided by the resistance of the medial cortical bone, and appropriate adjustment of the transverse angle was made when needed. It was necessary to ensure that the tip of the hand drill proceeded smoothly in the cancellous tunnel without any sudden advancement.
Palpation of the pedicle track with a slim ball-tip probe was performed if any abnormalities were felt while drilling, to identify the floor and the walls of the pedicle track and the intra-osseous borders. Particular attention was paid to the first 15–18 mm of the track, as the distance from the posterior projection points of the pedicle axis on the lateral mass to the junction of the vertebral body and pedicle [12]. If a soft tissue breach was palpated, the hand drill was carefully redirected and bone wax was placed in the pedicle track. After tapping and repeated exploration in the correct trajectory direction, screws with 3.5–4.0 mm diameter and 26–30 mm length were placed (Figs. 1, 2).
Operation schema of the CPS free-hand technique: decorticating on the lateral and superior quadrant area of the lateral mass, to create a bone hole (a); using a curette to scrape off the cancellous bone though bottom side of the hole and touch the interior side of medial pedicle wall (b); inserting 2-mm hand drill and feeling the cortical resistance of medial wall, making appropriate adjustment of the transverse angle (c); the hand drill proceeding smoothly in the cancellous tunnel and building the primary trajectory (d); identifying the integrity of the floor and four walls of the pedicle track by a slim probe, particularly for the first 15–18 mm (e); screw being inserted (f)
Due to differences of the pedicle entrance, the transverse angle of the hand drill may deviate the truly pedicle transverse angle, and its trajectory may be still within the cortical bone of the cervical pedicle (a, b). We emphasized that the hand drill was guided by the resistance of the medial cortical bone in our free-hand technique. Axial CT scan on C4 in which both side CPS were placed without perforation also revealed the difference of the transverse angle: left of patient 46.6°, right of patient 29.6° (c)
Evaluation of screw position
The integrity of the floor and four walls of the pedicle track were cautiously examined by using a ball-tip probe (or a tip bended 1-mm K-wire) after the drilling procedure or trajectory adjustment, as well as before screw insertion. All abnormal soft tissue breaches were recorded.
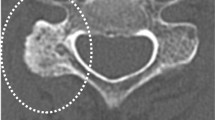
Postoperatively, superior or inferior pedicle wall perforation was assessed using left and right oblique radiographs; medial or lateral wall perforation and anterior vertebral perforation were assessed using axial CT scans with 1-mm slices to minimize the influence of boundary artifacts, and with sagittal and coronal two-dimensional CT reconstruction for detailed assessment. The transverse angle of the CPS trajectory was measured. The position of the CPS was assessed by two blinded spinal surgeons. Perforation of the lateral wall was classified according to the following definitions: grade 1, burst of pedicle wall by screw placement, with the external edge of the screw deviated out of the lateral pedicle by ≤2 mm; or grade 2, critical perforation of the pedicle wall by screw placement, with the screw deviated >2 mm out of the lateral pedicle (Fig. 3). Postoperatively, several patients with demonstrated pedicle perforation were nonrandomly selected for angiography under three-dimensional CT reconstruction, to investigate the changes of the blood flow of the vertebral artery.
Perforation of the lateral wall: grade 1, the external edge of the screw (right of patient) deviating out of the lateral pedicle by ≤2 mm (a, b); grade 2, with the screw (left of patient) deviating >2 mm out of the lateral pedicle (c, d). Postoperative CT angiography of the grade 2 perforation at left C4 demonstrated normal diameter of the left vertebral artery (e)
Statistical analysis
Measured data were analyzed using SPSS software version 17.0. Kappa statistics were applied to test the inter-rater reliability of the classification of the grade of pedicle perforation. Groups were compared using the Pearson χ2 test for categorical data. P values less than 0.05 were considered statistically significant.
Results
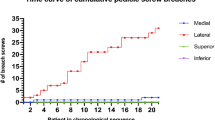
Among the 1,024 screws placed, 129 screws (12.64 %) breached the lateral pedicle wall, of which 101 (9.86 %) were classified as a grade 1 perforation (burst of pedicle wall) and 28 (2.73 %) as a grade 2 perforation (critical perforation). The inter-observer agreement rate was 87 % for the grade of pedicle perforation (mean kappa = 0.74) and intra-observer agreement rate was 93 % (mean kappa = 0.82), indicating good agreement for both inter-observer and intra-observer analyses. The general information involved patient demographics, screw placement results and breach rate of lateral pedicle wall are described in Table 1.
The incidence of lateral wall breaches in C3–C7 is described in Table 2, and breach of the lateral wall was significantly more frequent in C3 than in the other vertebrae (P < 0.05). Moreover, preoperative and postoperative axial CT measurements showed that the difference between the pedicle transverse angle and the screw trajectory angle was higher in the group with grade 2 perforations (18.15º ± 7.89º) than in grade 1 perforations (10.23º ± 6.17º). Twelve screws (1.17 %) also perforated the inferior cervical pedicle wall. No screws were observed to breach the medial or superior cervical pedicle walls.
Seven planned screw placements were aborted or changed to lateral mass screws during operation, because >2 mm of soft tissue was palpated on the lateral side during the hand drilling procedure. Of the 1,024 screws inserted, lateral soft tissue breach was palpated in 82 pedicles (8.01 %) during hand drilling. After bone wax insertion and trajectory adjustment, a tiny lateral wall perforation could still be detected in 56 pedicles (5.47 %). If a soft tissue breach occurred in the first 15–18 mm of the track and was less than 1 mm, all intra-osseous borders were carefully identified, and then tapping and screw placement was performed. Among the 28 screws with grade 2 perforation detected by axial CT scan, intra-operative abnormalities had been detected in 26 screws. However, intra-operative abnormalities had been detected in only 19 out of the 101 screws with grade 1 perforation. In addition, there were 37 screws encountered soft tissue breach but without CT-detected perforation.
The average follow-up time was 36.8 months (range 5–65 months). No patient showed symptom or sign of neurovascular injury related to CPS placement. Two screws (0.20 %) broke due to failed union in a trauma patient, but there was no subsequent deformity or neurological dysfunction secondary to removal of the screw and rod system. One screw (0.10 %) loosened in another patient who remains under observation and is asymptomatic.
Discussion
Perforation of the lateral pedicle wall in the cervical spine has been regarded as strongly associated with VAI. In our series of patients, a total of 101 screws were found to be grade 1 perforation (<2 mm) on postoperative CT scan, without clinical signs of VAI. Only in 19 of them intra-operative alarm signs were detected through palpation. We speculated that the reasons for this are as follows. First, anatomical data indicate that even though the outer diameter of the cervical pedicle is usually >3.5 mm, the actual width of the cancellous bone cavity (inner diameter) is usually <3.5 mm [13]. The cervical pedicle has a tear drop shape, with the inner height larger than the width and the medial cortex significantly thicker than the lateral cortex. When a 3.5 mm screw is placed in the correct trajectory, there may encounter transverse expansion and burst of the lateral cortex. Second, it should be noted that such injuries to the integrity of the lateral wall are difficult to palpate, as there are frequently fragments of pedicle cortex on the outside of the screw pathway, between the screw and the vertebral artery. For a 3.5-mm screw, grade 1 perforation is defined as a <2 mm breach, indicating deviation of nearly half of the screw diameter. It was indicated that the center axis of the trajectory tends to be in the cancellous bone cavity close to the original lateral cortical wall. The summation of the radius of screw and the thickness of lateral cortex was approximately equal to 2 mm. In other words, CPS placement in a correct trajectory may, therefore, lead to grade 1 perforation which is deemed as relatively safe to the vertebral artery, because of protectiveness from the fragment between the screw and the vertebral artery.
In our research, a total of 28 screws (2.73 %) showed grade 2 perforation, and no patient presented with symptoms indicating vascular injury or embolism, such as cerebral infarction. The term of “safe zone” concerning pedicle screws was claimed not only in thoracic spine, but also in cervical spine [14]. It describes the distance to which a CPS can potentially perforate the cervical pedicle laterally without causing vertebral artery injury in the cervical segment. Considering both the occupation rate and the safe zone, Tomasino et al. [14] calculated a theoretical distance of 2.5 mm that the CPS can shift the vertebral artery laterally without causing vascular injury. In addition, Sanelli et al. [15]reported significant variations in the size of the vertebral artery relative to the size of the transverse foramen, with the vertebral artery occupying 8–85 % of the foramen (occupation rate), and being precisely in the middle of the foramen in only 34 % of cases. It seemed that grade 2 perforation may not always directly damage the vertebral artery, for the fortunate distance between artery and pedicle wall. Moreover, lack of the clinical clues of VAI can attribute to compensation from opposite side vertebral artery, although one side VAI related to grade 2 perforation has been entercountered. However, our study found that a pedicle breach of more than 2 mm (grade 2 perforation) indicated that the trajectory angle of the hand drill had deviated (by an average of 18.15°) and had directly penetrated into the transverse foramen, which would greatly increase the risk of VAI or thrombus development caused by irregular blood flow compared to a grade 1 perforation (Fig. 4). Vertebral artery irregularities, such as tortuous or split arteries should also be considered, because of their lower tolerance for grade 2 perforations. In addition, the biomechanical strength of screws with a grade 2 perforation would obviously be reduced. It must be noted that the primary concern during CPS placement was the prevention of grade 2 perforations.
Axial CT scan on C5 detected lateral wall perforation of both sides: grade 1 on right and grade 2 on left (a). Interruption of the left vertebral artery was detected by postoperative CT angiography, though the patient showed no symptoms of vascular injury or embolism (b). Grade 2 perforation greatly increased the risk of VAI
Among the 28 grade 2 perforations, abnormalities were palpated during placement of 26 screws. During hand drilling, tapping, and partial screw insertion, the four walls and the floor of the pedicle track should be carefully palpated, with particular attention being paid to the first 15–18 mm of the track and the lateral wall. The surgeon always retreated and repeated palpation when an abnormal feeling was encountered, to get sufficient information about the pedicle walls for decisions of adjustment or abortion. Most grade 2 perforations were detected, and redirection was attempted. This could cause partial overlap between the original and redirected tracks, since adjustment of the hand drill trajectory within the narrow space of the cervical pedicle canal was very difficult, once the breach had occurred. Based on our experiences, we recommended changing to lateral mass screws once rebuilt CPS track has been shown difficult or demonstrated failure.
Among all the vertebrae involved in this study, C3 showed a higher frequency of breach of the lateral wall than others. In our opinion, this was not because of the small size of the C3 pedicle, but because of limited soft tissue exposure due to a desire to avoid C2 involvement, since extensive intra-operative soft tissue exposure was needed to achieve the correct trajectory angle. Besides, two techniques were crucial to increase the accuracy of screw placement. First, the ideal entry point cannot be determined based on posterior landmarks. According to morphometric studies, the location of the pedicle entrance on the posterior surface is unique to each level of the cervical vertebrae, and there may be large variations among individuals even at the same vertebral level [16]. We recommended identification of the precise entry point using a curette or hand drill, after the lateral mass being decorticated under proper exposure. Second, the trajectory of the CPS track on the axial plane should be guided by the thick medial wall. The resistance of the medial cortex should be carefully felt by the surgeon, and the tip of the hand drill should be adjacent to the medial wall and slowly advanced through the cancellous bone. Perforation of the medial pedicle wall did not occur in our series. We stress that carefully feeling the advancement of the pedicle screw is important to ensure safe free-hand CPS placement, which eliminates undetected medial wall perforation. According to our experience, these two techniques are especially helpful in degenerative patients with excessive osteophyte formation and osteoporosis, which was why in this study the perforation rate was nearly equal between patients with degenerative disease and trauma.
Abumi et al. [17] reported that their perforation rate during CPS placement was 6.7 % (45/669). In this study, 129 of 1,024 screws (12.64 %) showed lateral pedicle wall perforation, not including seven aborted pedicle screws. This rate seemed unacceptably high compared with previous reports, but if grade 1 perforations were excluded from the calculation, the results of the free-hand technique were good. We agreed that the assistance of navigation system can improve the accuracy of CPS placement, and it played a key role in pedicles with no medullary cavity or an extremely small medullary cavity. Richter et al. [18] compared the perforation rate between CPS placement assisted by lateral fluoroscopy or by a navigation system, and found a significant difference of 8.6 % (8/93) versus 3.0 % (5/167). Recently, Ishikawa et al. [8] reported a series of CPS placements using either three-dimensional fluoroscopy based navigation or conventional fluoroscopy. They found that the navigation system improved the accuracy of CPS placement, but the incidence of perforation when using the navigation system was 18.7 % (28/150), and severe CPS malposition causing VAI or neurological complications occurred even when using the navigation system. We could not perform a comparison between our free-hand technique and placement assisted by navigation system. However, we emphasize that the safe and successful application of modern technology must be based on having experience with careful palpation by hand feeling.
Due to the various pathologies and ages of the patients in this study, learning curve analysis of our CPS placement method could not be performed. However, we believe that CPS placement using our free-hand technique is technically demanding, and that there must be a remarkably learning curve for this method, as has been indicated by similar studies [9, 10]. Surgeons should be fully aware of the risks of CPS placement and should promptly review their experience after each unsatisfactory screw placement, to improve the accuracy and safety of their techniques.
References
Kotani Y, Cunningham BW, Abumi K, McAfee PC (1994) Biomechanical analysis of cervical stabilization systems: an assessment of transpedicular screw fixation in the cervical spine. Spine 19(22):2529–2539
Jones EL, Heller JG, Silcox DH, Hutton WC (1997) Cervical pedicle screws versus lateral mass screws: anatomic feasibility and biomechanical comparison. Spine 22(9):977–982
Abumi K, Itoh H, Taneichi H, Kaneda K (1994) Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord 7(1):19–28
Abumi K, Ito M, Sudo H (2012) Reconstruction of the subaxial cervical spine using pedicle screw instrumentation. Spine 37(5):E349–E356
Zheng X, Chaudhari R, Wu C, Mehbod AA, Transfeldt EE (2010) Subaxial cervical pedicle screw insertion with newly defined entry point and trajectory: accuracy evaluation in cadavers. Eur Spine J 19(1):105–112
Kast E, Morh K, Richter HP, Börm W (2006) Complications of transpedicular screw fixation in the cervical spine. Eur Spine J 15(3):327–334
Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, Ploumis A, Xenakis TA (2012) Accuracy of pedicle screw placement- a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation. Eur Spine J 21(2):247–255
Ishikawa Y, Kanemura T, Yoshida G, Ito Z, Muramoto A, Ohno S (2010) Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: a retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine 13(5):606–611
Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Kanno T, Masuda T (2009) Clinical accuracy of cervical pedicle screw insertion using lateral fluoroscopy: a radiographic analysis of the learning curve. Eur Spine J 18(9):1326–1334
Lee SH, Kim KT, Abumi K, Suk KS, Lee JH, Park KJ (2012) Cervical pedicle screw placement using the “Key slot technique”.The feasibility and learning curve. J Spinal Disord Tech (Epub Ahead of Print)
Karaikovic EE, Yingsakmongkol W, Gaines RW Jr (2001) Accuracy of cervical pedicle screw placement using the funnel technique. Spine 26(22):2456–2462
Jingmign Xie, Zhang Yangjie Lu, Ning Liu Zhongliang, Yingsong Wang, Ying Zhang (2006) Transpedicular screw fixation for the lower cervical spine: anatomical measurement. J Spinal Surg 4(6):354–358 (CHN)
Zhu RF, Yang HL, Hu XY, He XS, Tang TS, Chen L, Li XG (2008) CT evaluation of cervical pedicle in a Chinese population for surgical application of transpedicular screw placement. Surg Radiol Anat 30(5):389–396
Tomasino A, Parikh K, Koller H, Zink W, Tsiouris J, Steinberger J, Hartl R (2010) The vertebral artery and the cervical pedicle: morphometric analysis of a critical neighborhood. J Neurosurg Spine 13(1):52–60
Sanelli PC, Tong S, Gonzalez G, Eskey CJ (2002) Normal variation of vertebral artery on CT angiography and its implications for diagnosis of acquired pathology. J Comput Assist Tomogr 26(3):462–470
Karaikovic EE, Kunakornsawat S, Daubs MD, Madsen TW, Gaines RW Jr (2000) Surgical anatomy of the cervical pedicles: landmarks for posterior cervical pedicle entrance localization. J Spinal Disord 13(1):63–72
Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K (2000) Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine 25(8):962–969
Richter M, Wilke HJ, Kluger P, Neller S, Claes L, Puhl W (2000) Biomechanical evaluation of a new modular rod-screw implant system for posterior instrumentation of the occipito-cervical spine: in vitro comparison with two established implant systems. Eur Spine J 9(5):417–425
Acknowledgments
The authors thank Mr. Kazuki Kawakami and Mr. Dmitri Kim for the assistance of grammatical modification in the language performance.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Y., Xie, J., Yang, Z. et al. Computed tomography assessment of lateral pedicle wall perforation by free-hand subaxial cervical pedicle screw placement. Arch Orthop Trauma Surg 133, 901–909 (2013). https://doi.org/10.1007/s00402-013-1752-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1752-3