Abstract
Background
Morel-Lavallee lesion (MLL) of the peri-pelvic region is less common and various treatments have been introduced to manage the lesion. No standard treatment is recommended. We performed a systematic review of literature to (1) identify the classification of peri-pelvic MLL; (2) review the treatments of the lesion and their complications; (3) define the optimal treatment of peri-pelvic MLL.
Methods
A systematic search was performed via PubMed, ISI Web of Knowledge, and Embase for English abstract articles from 1966 to 2012. We identified 21 articles detailing 153 patients with peri-pelvic MLL, most of which were level IV studies. The treatments and clinical results were reviewed.
Results
For peri-pelvic MLL patients, surgical intervention was better than conservative therapy. Sclerhodesis method is attended with good outcome in the symptomatic MLL patients without fractures. Patients with peri-pelvic fractures could be managed with local suction drainage or open debridement with dead space closure technique during fracture fixation. The delayed-diagnosis cases might be treated with mass resection when fibrosis capsule was obtained in magnetic resonance imaging.
Conclusions
Peri-pelvic MLL can be treated with various surgical methods depending on the formation of fibrosis capsule and associated injuries. Dead space closure technique is emphasized in the treatment of MLL. Higher quality of literature is required to prove this result in future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morel-Lavallee lesion (MLL), which is known as “internal degloving injury,” is a result of subcutaneous fatty tissue that has been separated from the surface of the fascia by a shearing force [1]. A closed space is then formed between the subcutaneous layer and fascia layer, which is filled with hemotoma and necrosis tissues. The patient who suffers from MLL might present with fluctuant swelling at the injury site and the sensation of the site might be abnormal. This lesion occurs so infrequently that the patients might be misdiagnosed [2, 3].
The diagnosis of MLL may be assessed by clinical examination and radiological evidence. Magnetic resonance imaging (MRI) and ultrasound have great effect in the diagnosis of MLL [4]. However, MLL can remain undetected when a patient does not present with a history of fracture [2, 3, 5–7]. As a result delayed diagnosis makes later treatment much more difficult. Moreover, the treatment of delayed-diagnosis MLL might be different from that of acute MLL.
Various methods of management of MLL have been introduced in the past decades [8–11]. However, the efficacy of MLL treatment is still controversial. The aim of the current study was to review the literature focused on the clinical interventions and their results of peri-pelvic MLL. We therefore performed the present study regarding the treatment of MLL to (1) determine whether these interventions are effective; (2) identify complications associated with these interventions; and (3) define the optimal treatments of peri-pelvic MLL.
Methods
Eligibility criteria
We performed a comprehensive search via PubMed, EMBASE, and ISI databases for abstracts of articles that were published between January 1966 and October 2012. We used the following keywords: Morel–Lavallee lesion, Morel–Lavallee effusion, soft tissue injuries, and fat necrosis. All the articles relevant to the subject were collected and their references were also reviewed. The search was limited to articles which provided English-language full-text.
All the studies were reviewed by two independent investigators for content (CS and JPP). The site of MLL was limited to the peri-pelvic region. Any study that did not mention intervention and clinical outcome was excluded from the current study. Studies which reviewed the imaging of MLL were also excluded from further review.
Statistics
The unpaired t test and Fisher exact test were used in assessing the difference between the results from the articles. The level of statistical significance was defined as any p values > 0.05.
Result
A total of 21 studies published between 1997 and 2012 were found to be eligible for inclusion in our review and the full text of each article was obtained. The information from each article was reviewed independently by the two authors mentioned above. If the information from the same article was controversial, then a third senior author (XDC) was consulted. The references of each article were also reviewed. The studies detailed the cases of 153 patients who suffered from MLL in the peri-pelvic region. Gender was described in 141 patients; 91 were male and 50 were female. The characteristics of the studies included in present review were listed in Table 1.
Classification of MLL
In the reviewed literature, there was no standard classification of MLL. Of all the studies included in our review, only two publications introduced their own categories. Hak et al. [12] reviewed 24 cases and divided the patients into two groups (open type and closed type) depended upon whether the wound was open or closed. Carlson et al. [13] divided MLL into acute type (treatment performed fewer than 3 weeks after injury) and chronic type (treatment performed 3 weeks or more after injury). However, all the patients in their studies received the same treatment and thus the definition they used had no relevance to the management of MLL.
Conservative versus surgical treatment
Among the studies included, 13 patients in five studies underwent conservative treatment [3, 7, 10, 14, 15]. The healing rate of conservative treatment of MLL was less than 50 %. Seven of these patients failed in conservative treatment and five of them took later surgical treatment. The other two patients refused to take surgical intervention and the lesion became chronic. Imaging indicated that local lesions presented as fibrous organization tissue in final follow-up in these two patients. All the data suggested that conservative treatment was less effective in the management of MLL.
A total of 140 patients underwent various kinds of surgical interventions. Although the patient might receive several surgeries and suffered from several complications, such as deep infection or disorder of the surgical wound, 133 patients mentioned in 16 studies had a satisfactory clinical result at final follow-up. The difference in the healing rate between conservative and surgical treatment was statistically significant (p < 0.05).
Compressive bandage application
In 8 of 13 patients who received conservative treatment, compressive bandages were applied. Of these, three failed conservative treatment and all of them took further surgical interventions. All of the cases that did not receive compressive bandage application failed conservative treatment. The results suggested that compressive bandage application had an important role in the conservative treatment of MLL. Moreover, several authors emphasized the use of compressive bandages after surgical intervention with sclerodhesis method [9, 16].
Local aspiration
In the patients who underwent surgical treatment of MLL, there were five cases that underwent isolated local aspiration treatment, with four cases experiencing failure. Vico et al. [2] reported that one patient received aspiration treatment frequently for 5 months. However, the patient still had an obvious thigh deformity and MRI examination suggested a lipoma that was formed after 18 months. Luria et al. [17] also reported two cases that failed in aspiration of MLL and were later managed with talc sclerodhesis technique.
Open debridement
Four studies reported using open debridement of MLL in 70 cases. All of the authors recommended thorough debridement of the necrotic tissue of MLL. However, there was disagreement on the time needed for wound closure. Hak et al. [12] reported on 24 patients who were treated for MLL. All patients received open debridement and dressing for second intention healing. Six of these had delayed wound closure after several debridement surgeries and three patients needed skin grafting or flap. However, Steiner et al. [10] reported 19 cases of MLL who were treated using open debridement with primary or delayed closure of the wound. In their study, 5 of 11 cases were treated with primary wound closure and suffered from different complications (three with reoccurrence of MLL and two with soft tissue necrosis). There were also three cases which had complications with delayed wound closure (one soft tissue necrosis and two infections). Carlson et al. [13] reported on 22 cases of debridement and dead space closure treatment. In their study, all the patients were cured with primary wound closure and no infections or re-accumulations of fluid were obtained. Only flap marginal necrosis was mentioned in two cases. The results indicated that open debridement combined with dead space closure might have an encouraging outcome in MLL patients.
Local drainage
Forty-six cases received wound drainage treatment with 34 of them using post-operative suction drainage or vacuum suction [11, 18–20]. In the patients who received normal drainage treatment, 7 of 12 cases had a reoccurrence of MLL. In the patients with suction drainage or vacuum suction, there were seven cases of infection and only one case with a reoccurrence of MLL. The total complication rate using wound drainage was 30.4 % and there was a significant difference in the complication rate between normal drainage and drainage with suction (7/12 versus 8/34, p < 0.05).
Sclerodhesis of MLL
Luria et al. [17] reported four cases that were managed with a talc sclerodhesis technique after prior failed puncture or drainage. All the patients were treated with suction drainage and later talc injection. Only one patient suffered from infection. Demirel et al. [16] reported on five patients with seven acute cases of MLL. All the patients healed without any complications. Bansal et al. [9] reported on the treatment of 13 patients using doxycycline sclerodhesis. Only one patient without application of a compressive bandage failed after 12 weeks. All authors who used the sclerodhesis technique emphasized the importance of concurrent compressive bandage application. Penaud et al. [8] reported on the management of five patients who had persistent MLL for 3 months using both a compressive bandage and the alcohol sclerodhesis method. The total success rate of sclerodhesis in the treatment of MLL was 95.7 %. Nevertheless, all the patients who underwent a sclerodhesis treatment were not associated with any fractures.
Hematoma resection
Five studies focused on five cases that used resection of the lesion. All the cases were chronic MLL with a fibrous capsule formed in radiological evidence [2, 5–7, 21]. Two cases had post-operative complications. Kalaci et al. [5] reported on a 56-year-old male patient with chronic MLL 4 years after injury. The resection of the mass was performed with primary closure of the wound and suction drainage. However, the mass recurred 1 month after the surgery but healed 6 months later after the final drainage. Tran et al. [21] reported on a 29-year-old male patient who suffered from post-operative bleeding after resection of the chronic MLL mass. The patient underwent immediate wound exploration and transfused blood. After thorough irrigation of the dead space, the wound was closed and the patient healed 6 months later.
Complications
The complications of MLL treatment included infection, skin necrosis, and reoccurrence of MLL. Out of the 153 patients who were included in our review, 29 were infected or culture-positive [10–13, 17, 19, 20, 22]. Most of the infections were managed by application of antibiotic. The microorganisms detected in the lesion site included Enterobacter cloacae, Acinobacter baumannii, Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus epidermidis, and Staphylococcus aureus. Skin necrosis was more common in debridement patients and sometimes soft tissue grafting was needed.
Discussion
MLL was first described in 1853 and subsequently diagnosed in acetabular fracture patients by Letournel and Judet [1]. It is more common in peri-pelvic fracture patients with high-impact trauma. Nevertheless, some publications reported that such lesion was not always associated with fractures and thus made the diagnosis and treatment difficult [2, 3, 7]. Treatments of MLL vary in the literature and no standard treatments are recommended. Controversy still exists about the optimal treatment of MLL. Therefore we performed present study to review the results of various treatments in peri-pelvic MLL.
Our results suggested surgical intervention had better outcomes than conservative treatment in the management of peri-pelvic MLL, especially open debridement with primary dead space closure technique. In isolated MLL patients without fracture, sclerodhesis after local drainage might be the best choice. In chronic MLL cases, resection of the lesion mass was the only method of treatment after a fibrosis capsule formed. Attention should be paid to post-operative complications after surgery.
There is no well-accepted classification of MLL. A useful classification should be easily understood and helpful in the treatment of MLL. In the literature reviewed in this study, we found two classification systems of MLL. These categories were easy to comprehend but not helpful to the treatment. Mellado’s classification of MLL depended on the MRI results with corresponding histopathology [4]. However, their classification had no relation to the clinical outcome or treatment of MLL. Based on the results of our literature review, we thought that MLL could be categorized into acute and chronic types depending on the occurrence of a thick fibrous capsule. Once the occurrence of fibrous capsule was obtained, the only treatment was mass resection. However, this type of classification needs to be further verified.
Harma et al. [14] identified a conservative approach to closed MLL. The lesion sites were applied with elastic bandages or corsets and all lesions healed within a mean of 6.8 ± 3.96 weeks. However, the authors also mentioned that there were two patients who suffered from sacral decubitus and recurrence of the lesion, with later surgical intervention. In all patients with MLL who received conservative treatment, the healing rate is lower than those with surgical treatment. Other case reports also mentioned failure of conservative treatment of MLL [2, 3, 7]. Thus, the conservative treatment is less recommended now in the treatment of peri-pelvic MLL.
Local drainage and open debridement seem to be the most popular surgical treatments of peri-pelvic MLL. The difference of the total complication rate between these methods was not significant (13/70 versus 14/46, p > 0.05). Local drainage removes necrosis tissue with less invasive surgery and thus minimized the risk of skin necrosis. Open debridement surgery thoroughly removes the hemotoma and necrosis tissue and decreases the possibility of recurrence of the lesion (4.2 versus 17.4 %) and rate of infection (7.1 versus 15.2 %). However, the difference between the infection or recurrence rate between local drainage and open debridement was not statistically significant.
Carlson et al. [13]. reported satisfactory result with all the patients treated with open debridement and dead space closure technique. In their study, all the patients had healing of the lesion without any infection or recurrence of the lesion. Furthermore, sclerodhesis treatment closed the dead space in MLL with a low complication rate [16, 17]. Parra et al. [3] also mentioned a patient who failed in conservative treatment healed after irrigation and dead space closure. Thus, we emphasized the importance of dead space closure in the treatment of peri-pelvic MLL.
Our review has some limitations. One limitation is due to the level of evidence of the literature in our review, which were case series and review articles. A second limitation is that there have been few reports on the treatment of long-standing MLL. A third limitation is that most of the literature did not describe the use of antibiotics in detail. Further studies should be focused on the comparison of different treatments of MLL and the management of the lesion should be described in greater detail.
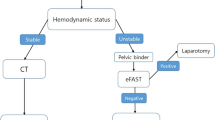
In conclusion, we suggested an algorithmic approach to the management of peri-pelvic MLL depending on the image and associated injury (Fig. 1). Surgical intervention was recommended with symptomatic MLL. MLL with fibrous capsule could be treated with mass section. Isolated MLL could be managed with sclerodhesis treatment.
References
Morel-Lavallee (1863) Decollements traumatiques de la peau et des couches sous-jacentes. Arch Gen Med (1):20-38, 172-200, 300–332
Vico PG (2000) Morel-Lavallee syndrome. Eur J Plast Surg 23(1):45–48
Parra JA, Fernandez MA, Encinas B, Rico M (1997) Morel-Lavallee effusions in the thigh. Skelet Radiol 26(4):239–241
Mellado JM, Bencardino JT (2005) Morel-Lavallee lesion: review with emphasis on MR imaging. Magn Reson Imaging Clin N Am 13(4):775–782
Kalaci A, Karazincir S, Yanat AN (2007) Long-standing Morel-Lavallee lesion of the thigh simulating a neoplasm. Clin Imaging 31(4):287–291
Puig J, Pelaez I, Banos J, Balliu E, Casas M, Maroto A, Pedraza S (2006) Long-standing Morel-Lavallee lesion in the proximal thigh: ultrasound and MR findings with surgical and histopathological correlation. Australas Radiol 50(6):594–597
Mellado JM, Perez del Palomar L, Diaz L, Ramos A, Sauri A (2004) Long-standing Morel-Lavallee lesions of the trochanteric region and proximal thigh: MRI features in five patients. AJR Am J Roentgenol 182(5):1289–1294
Penaud A, Quignon R, Danin A, Bahe L, Zakine G (2011) Alcohol sclerodhesis: an innovative treatment for chronic Morel-Lavallee lesions. J plast, Reconstr Aesthet surg : JPRAS 64(10):e262–264
Bansal A, Bhatia N, Singh A, Singh AK (2013) Doxycycline sclerodesis as a treatment option for persistent Morel-Lavallee lesions. Injury 44(1):66–69
Steiner CL, Trentz O, Labler L (2008) Management of Morel-Lavallee lesion associated with pelvic and/or acetabular fractures. Eur J Trauma Emerg Surg 34(6):554–560
Tseng S, Tornetta P 3rd (2006) Percutaneous management of Morel-Lavallee lesions. J Bone Jt Surg Am 88(1):92–96
Hak DJ, Olson SA, Matta JM (1997) Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallee lesion. J Trauma 42(6):1046–1051
Carlson DA, Simmons J, Sando W, Weber T, Clements B (2007) Morel-lavalee lesions treated with debridement and meticulous dead space closure: surgical technique. J Orthop Trauma 21(2):140–144
Harma A, Inan M, Ertem K (2004) The Morel-Lavallee lesion: a conservative approach to closed degloving injuries. Acta Orthop Traumatol Turc 38(4):270–273
Mukherjee K, Perrin SM, Hughes PM (2007) Morel-Lavallee lesion in an adolescent with ultrasound and MRI correlation. Skelet Radiol 36(Suppl 1):S43–45
Demirel M, Dereboy F, Ozturk A, Turhan E, Yazar T (2007) Morel-Lavallee lesion. Results of surgical drainage with the use of synthetic glue. Saudi Med J 28(1):65–67
Luria S, Applbaum Y, Weil Y, Liebergall M, Peyser A (2006) Talc sclerodhesis of persistent Morel-Lavallee lesions (posttraumatic pseudocysts): case report of 4 patients. J Orthop Trauma 20(6):435–438
Labler L, Trentz O (2007) The use of vacuum assisted closure (VAC) in soft tissue injuries after high energy pelvic trauma. Langenbecks Arch Surg 392(5):601–609
Kohler D, Pohlemann T (2011) Operative treatment of the peri-pelvic Morel-Lavallee lesion. Oper Orthop Traumatol 23(1):15–20
Phillips TJ, Jeffcote B, Collopy D (2008) Bilateral Morel-Lavallee lesions after complex pelvic trauma: a case report. J Trauma 65(3):708–711
Tran W, Foran J, Wang M, Schwartz A (2008) Postsurgical bleeding following treatment of a chronic Morel-Lavallee lesion. Orthopedics 31(8):814
Suzuki T, Hak DJ, Ziran BH, Adams SA, Stahel PF, Morgan SJ, Smith WR (2009) Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury 40(4):405–409
Acknowledgments
This study was supported by the National Natural Science Foundation of China (81101379, 81171705) and Natural Science Fund of Shanghai Jiao Tong University School of medicine (11XJ21022).
Conflict of interest
The author(s) declare that they have no competing interests
Author information
Authors and Affiliations
Corresponding author
Additional information
Chao Shen and Jian-Ping Peng contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Shen, C., Peng, JP. & Chen, XD. Efficacy of treatment in peri-pelvic Morel–Lavallee lesion: a systematic review of the literature. Arch Orthop Trauma Surg 133, 635–640 (2013). https://doi.org/10.1007/s00402-013-1703-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1703-z