Abstract
Objective
The growing demand for total knee arthroplasty (TKA) associated with the efforts to contain healthcare expenditure by advanced economies necessitates the use of economically effective technologies in TKA. The present analysis based on activity-based costing (ABC) model was carried out to estimate the economic value of patient-matched instrumentation (PMI) compared to standard surgical instrumentation in TKA.
Methodology
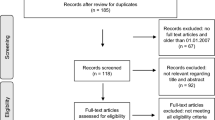
The costs of the two approaches, PMI and standard instrumentation in TKA, were determined by the use of ABC which measures the cost of a particular procedure by determining the activities involved and adding the cost of each activity. Improvement in productivity due to increased operating room (OR) turn-around times was determined and potential additional revenue to the hospital by the efficient utilization of gained OR time was estimated.
Results
Increased efficiency in the usage of OR and utilization of surgical trays were noted with patient-specific approach. Potential revenues to the hospital were estimated with the use of PMI by efficient utilization of time saved in OR. Additional revenues of €78,240 per year were estimated considering utilization of gained OR time to perform surgeries other than TKA.
Conclusions
The analysis suggests that use of PMI in TKA is economically effective when compared to standard instrumentation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal disorders are group of conditions which are reported to be one of the important causes of pain and disability around the world. They decrease quality of life as they affect social functioning and mental health. They contribute to 2 % of the global economic disease burden [1]. The prevalence increases considerably with age [2]. Knee osteoarthritis is the most common arthropathy affecting the knee [3, 4] and is an important cause of disability in older people [5, 6]. Osteoarthritis might become the fourth leading cause of disability by 2020 which is attributable to the increased life expectancy and ageing [7].
An increasing trend is being observed in healthcare costs in the United States and Europe for the past several decades. The rises in healthcare costs are due to the advances in technology, progressive health awareness among people and ageing population [8]. There are continued pressures in all advanced economies to contain the growth in healthcare expenditure. In addition, deteriorating financial position of healthcare providers is leading to an emphasis on cost reduction for economic survival. In this context of financial constraints faced by many health systems, demonstration of value for money or economic efficiency of healthcare interventions has become an absolute necessity [9].
Total knee arthroplasty (TKA) is the frequently performed procedure which effectively relieves pain and restores functional status in patients with advanced knee osteoarthritis. A recent survey conducted in 18 countries with a total population of 755 million observed a substantial rise in demand for TKA over the past decade with compound annual growth rate ranging from 5.3 to 17 % among different countries [10]. Ageing population, more active lifestyle of the elderly, the increase in prevalence of obesity, demographical changes and substantial advances in the implant preparation and surgical procedure are few factors which contribute to the increase in demand for TKA [11]. It is anticipated that there will be a substantial increase in the demand for primary TKA among patients over 65 years of age with the greatest growth being in the 45–54-year age category [12]. If the number of procedures performed continues at the current rate, the demand for primary TKA in United States is expected to reach 3.48 million procedures by 2030 from 450,000 procedures in 2005 indicating a growth of 673 % [13].
With the growing demand for TKA and associated increase in the annual volume of TKA procedures, considerable pressure is expected to build on hospitals and surgeons to contain costs in the coming years [14]. These mounting cost pressures may impose the need for interventions, which improve efficiency and effectiveness by reducing operative time, duration of hospital stay, and equipment inventory thereby leading to increase in frequency with which the procedure is performed [15].
Recently, attention has been focused on a relatively new arthroplasty technology called patient-matched instrumentation (PMI) which is intended to improve surgical precision and may lead to improved clinical outcomes. This technology involves design of patient-specific cutting blocks based on patient’s anatomy using data obtained from preoperative magnetic resonance imaging (MRI) of the patient’s knee and a full length X-ray of the leg. The customized cutting blocks help the surgeon to position the knee implant in optimal mechanical alignment through precise bone cuts [16]. It has been reported that PMI minimizes tissue loss, decreases operating time and increases operating room (OR) efficiency by reducing instrument inventory [15, 16]. Additionally, PMI potentially decreases storage and loaner costs of instruments for medical device companies which could lead to an economic benefit as well. Therefore it might contribute to lower implant and instrument prices.
Based on prospective pricing system implemented in many economies, hospital cases are classified into diagnosis-related groups (DRG). Hospitals are paid a fixed price for each inpatient case, based on the patient’s DRG. If the costs incurred by the hospital on a particular patient are less than DRG price, hospital retains the difference. Hospital needs to absorb the loss if its costs are higher than DRG price [17]. Thus, improving efficiency in commonly performed surgeries like TKA will help to improve the hospital economics to a great extent.
In this context, we have carried out an activity-based costing (ABC) analysis in a midsize hospital in Germany with the objective to compare economic impact of PMI when compared to standard instrumentation in TKA, from the perspective of the hospital.
Materials and methods
The costs of the two approaches, PMI (VISIONAIRE™ patient-matched TKA instrumentation, Smith & Nephew, Inc., Memphis, TN, USA) and standard instrumentation in TKA, were determined using ABC. This methodology identifies the activities in a procedure and assigns the cost of a particular procedure by adding the cost of each activity. It assigns costs to activities based on their use of resources, rather than products or services. This enables resources and other associated costs to be more accurately attributed to the procedure which they use. The ABC model is advantageous as it improves the accuracy of treatment costing, provides timely cost information suitable for decision making and allows more detailed tracking of cost per activity [18].
Procedure-related practices specific to standard instrumentation and PMI were identified and all potential cost factors were included into the ABC model. The factors include activities in policlinic, diagnostics involved, OR time, surgical tray utilization, blood transfusion, physiotherapy treatment, quality control, hospital stay and complications associated with TKA (Table 1). The analysis aimed to compare all costs associated with the TKA. However, overhead or indirect costs were not included in the model.
In addition to the costs, possible improvements in efficiency due to factors like reduction of OR time and less tray utilization were also determined. It was hypothesized that time and resources saved due to enhancement of efficiency of the procedure can be utilized to generate additional revenue for the hospital. Costs and improvement in efficiency in all activities from first contact of the patient until discharge were considered for the analysis. For each activity, parameters which were considered include the average number of times an activity was performed, percentage of patients in whom the activity was performed, by whom the activity was performed and the use of resources during that activity.
The costs of each defined parameter (Table 1) and resources utilized were estimated based on field research as well as from internal database of a health-economic consultancy company (Assist Zorgverbetering, Netherlands). ABC model for the TKA procedure was checked and validated by the senior author of this manuscript. It was conservatively assumed that clinical utility of comparators was equivalent. The technology which is economically beneficial while achieving the same outcome will be the ‘cost-effective’ technology.
The number of TKAs performed in the base case was 350 per year (seven surgeries within 3 days a week). The standard costs associated with each defined activity were established. Average cost per day of hospital stay was established as €245. Cost per hour of orthopedic OR time (including the cost of personnel involved) was established as €888. Processing cost per surgical tray for preparation and sterilization was €40. DRG reimbursement for a TKA case was €7,100. The price of knee prosthesis was €2,000 while the purchase price of patient-matched cutting block was €700 (Table 1).
The gross OR time for a TKA, defined as the sum of the surgery time and the preparation time, was estimated to be 100 min and it was assumed that time saved will lead to gains in the efficiency of the procedure as well as allow the hospital to carry out additional surgeries. The OR times required for other procedures were as follows: total hip arthroplasty, 80 min; minor orthopedic surgical procedure, 50 min and arthroscopy, 30 min.
Sensitivity analysis was carried out to determine the effect of OR time difference and number of surgeries per year on the incremental gross margin per week.
Results
The overall costs associated with hospital stay, physiotherapy treatment, blood transfusion and quality control were assumed to be equal among standard instrumentation and PMI as we do not have any other evidence-based information. No noticeable difference was observed in immediate clinical outcome between standard treatment and treatment with patient-matched cutting blocks in patients who underwent arthroplasty.
Remarkable difference in utilization of resources was observed in OR time and surgical tray utilization between the two procedures (Tables 2, 3). A decrease of 10 min in cutting time per procedure was noticed with PMI. In addition, a difference of 20 min was observed in the preparation of OR time when compared to standard treatment (Table 2). Surgery with PMI also led to utilization of four less surgical trays (Table 3). The reduction in total OR time will lead to realization of savings of €553 per TKA procedure to the hospital. The reduction in surgical tray utilization could result in potential cost savings of €160 per case (Table 4).
A small difference (€10) in Policlinic cost was observed as some of the preoperative work could be done by personnel other than the surgeon. Diagnostics reflects the costs of all preoperative diagnostic examinations. It was assumed that the out of all standard patients, 50 % require a knee thorax X-ray, 50 % a total leg X-ray, 100 % a knee or lower leg X-ray, 50 % a pelvis and hip joint X-ray, and 20 % of these patients require an MRI. In PMI, 50 % of the patients may require a knee thorax, 100 % a total leg X-ray, 50 % a knee and/or lower leg X-ray and 50 % a pelvis or hip joint X-ray for producing the blocks and 100 % of the patients require an MRI. The difference of €82 in diagnostics in PMI results out of the requirement for additional MRI and X-ray. The overall cost associated with both standard instrumentation and PMI was found to be almost equivalent with PMI costing just €59 more (Table 4).
For seven TKA procedures which are estimated to be performed in a week in our hospital, 210 min could be saved utilizing PMI (Table 2). By assuming that the saved time was utilized to perform procedures other than TKA (Table 5), the potential gross margin per week was found to be €1,630. This will result in additional revenue of €78,240 per year to the hospital considering 10,500 min time saved for 350 procedures (Table 6).
To assess the robustness of the conclusions, a sensitivity analysis was performed to demonstrate the effects of OR time difference and number of surgeries on gross margin. Figure 1 presents the sensitivity analysis in which the total OR time difference in minutes is varied on the x-axis and the incremental gross margin per week in Euros is varied across the y-axis.
Figure 2 presents the sensitivity analysis in which the number of surgeries is varied on the x-axis and the incremental gross margin per week in Euros is varied across the y-axis.
Discussion
Patient-matched instrumentation is intended to increase the efficiency of TKA and reduce hospital resource use during TKA. However, limited studies were available which demonstrate the cost effectiveness of TKA with PMI compared to standard instrumentation. The present analysis aims to determine the value associated with the use of PMI in TKA compared to standard TKA.
Additional costs incurred with PMI include cost of cutting blocks of €700 and cost of diagnostics of €82 (Table 4). The MRI needed for PMI is not a diagnostic MRI known for other procedures. The MRI needed for PMI is a kind of a technical MRI which is done within half of the time needed for a diagnostic MRI and additionally no diagnosis of the radiologist is needed. Therefore, the actual estimated MRI costs for PMI were €92.50. As some of the patients treated with standard instrumentation also need an MRI, the cost difference for diagnostics between the two treatments was €82.
The additional costs associated with PMI were offset by increase in the efficiency of the procedure which led to cost savings due to reduction in OR time and reduced surgical tray utilization. Thus, the overall costs associated with both standard instrumentation and PMI were almost identical with PMI costing just €59 more.
It was reported that room and board, OR time, and supply costs (medical, surgical and implants) represent approximately 73 % of hospital expenses for a primary TKA [19]. Therefore, decreasing OR time and surgical tray utilization may be considered key factors in reducing hospital expenses. The use of PMI was found to reduce the number of surgical trays. This could be attributed to the fewer instruments required due to the elimination of steps such as intraoperative sizing and intramedullary alignment guide placement. Less tray openings could potentially decrease the costs associated with maintenance, storage and sterilization and contribute to cost savings. It was observed that PMI led to utilization of four trays less (Table 3) compared to standard instrumentation which could result in cost savings of €160 per procedure (Table 4). This in turn may improve the overall productivity as a result of increased operating room turn-around time.
Patient-specific approach has the potential to improve productivity as a result of less room set-up and cleanup time, resulting in improved turnover time. The difference in preparation requirements between patient-specific TKA and conventional TKA was found to decrease OR turnover time by 20 min. In addition, reduction in cutting time was found to be 10 min (Table 2). Reduction in operative time is achieved using the implant guide as a consequence of reduced time for determination of the size of the implant during a procedure and intramedullary pin placement. Decreased OR operational costs of PMI due to the reduction in OR time could result in cost savings of €553 per TKA procedure. However, the benefits of gained OR time extend beyond these cost savings as hospital can generate additional revenue by utilizing this time to perform additional minor surgeries.
It was observed from the ABC model that 10,500 min could be saved in OR annually using PMI (Table 2). The cumulative OR time gained per intervention may be used to increase case load in a particular day while utilizing similar total resources. This could lead to increase in efficiency and overall revenue to the institution and also might accommodate the increasing demand for TKA. The time can also be efficiently used to perform additional procedures such as minor orthopedic surgical procedure and arthroscopy which require considerably less OR time compared to TKA (Table 5). Additional gross margin per year by utilizing gained OR time to perform surgeries other than TKA was estimated to be €78,240 from the ABC model (Table 6). Figure 2 demonstrates that gross margin for the hospital can be improved remarkably by performing additional surgeries.
The reduction in OR time, surgical tray utilization and the potential economical benefits correlate favorably with previous findings. In a study by Watters et al. [16] the patient-specific approach was found to reduce the preparation and operative times and saved additional 28 min of OR time per intervention compared to conventional methods and an additional 67 min compared to computer navigation. The authors reported that these time savings might provide a greater economic impact to the health care system than implant-related cost savings. In another single center, prospective, randomized clinical study by Noble et al. [15] statistically significant reductions in skin-to-skin operative time (mean 121.4 vs. 128.1 min; p = 0.048) and surgical tray utilization (mean 4.3 vs. 7.5 trays; p < 0.0001) were found with PMI compared to standard surgical instrumentation.
In health economic approach, it is widely advocated to take as broad a perspective as possible [20]. Economic analysis which focuses on the overall cost of treatment rather than on immediate cost of a device or product might provide valuable insights into the cost effectiveness of a particular treatment. PMI might be economically effective to a hospital by reducing the overall costs associated with TKA despite the higher costs associated with cutting blocks and diagnostics. Health economics helps in the decision making of health systems by providing the information needed, rather than dictating a decision [20]. Hospitals should evaluate all possible factors associated with PMI before implementing the technology.
Limitations
This study has a few limitations. Factors such as patient characteristics, operating room efficiency, cost allocations, labor costs, implant selection, and surgical technique may vary by hospital and country. Further, the study assumes that the PMI is comparable to SSI in long-term clinical effectiveness. Though long-term data are unavailable, preliminary results indicate that PMI might be clinically more effective in the long term [21].
Models have several strengths and weaknesses. The veracity of the model depends on the accuracy of the assumptions made within the model. As it is impossible to get all parameters out of one source, different sources were used in the model. Therefore, the validity of the outcome depends on the accuracy of these values. However, models like this can be adapted all the time, can easily incorporate multiple end points, and can be extended to reflect actual clinical practice.
Conclusions
The results of the present analysis suggest that PMI is an economically effective method in TKA. The use of PMI can lead to incremental revenue to the hospital but it is conditional on that time savings are effectively used to perform additional procedures. Additional revenue will probably offset the higher costs associated with cutting blocks and diagnostics. These economical benefits along with the previously reported clinical benefits support the increasing use of PMI in TKA. However, further large-scale and long-term clinical outcome studies evaluating the cost effectiveness of PMI are warranted.
References
Theofilou P, Panagiotaki H (2012) The association between musculoskeletal disorders and quality of life. J Trauma Treatment 1:e101
Brooks PM (2006) The burden of musculoskeletal disease—a global perspective. Clin Rheumatol 25(6):778–781
Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM (1995) Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum 38:1134–1141
Andrianakos AA, Kontelis LK, Karamitsos DG, Aslanidis SI, Georgountzos AI, Kaziolas GO, Pantelidou KV, Vafiadou EV, Dantis PC, ESORDIG Study Group (2006) Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece.The ESORDIG study. J Rheumatol 33:2507–2513
Martin J, Meltzer H, Elliot D (1988) OPCS surveys of disability in Great Britain. Report 1. The prevalence of disability among adults. Wiley, Office of Population Censuses and Surveys, Social Survey Division, London
Dillon CF, Rasch EK, Gu Q, Hirsch R (2006) Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol 33(11):2271–2279
Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81(9):646–656
Goyen M, Debatin JF (2009) Healthcare costs for new technologies. Eur J Nucl Med Mol Imaging 36(Suppl 1):S139–S143
Drummond M (2006) Pharmacoeconomics: friend or Foe? Ann Rheum Dis 65(Suppl 3):iii44–iii47
Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gómez-Barrena E, de Pina Mde F, Manno V, Torre M, Walter WL, de Steiger R, Geesink RG, Peltola M, Röder C (2011) International survey of primary and revision total knee replacement. Int Orthop 35(12):1783–1789
Otten R, van Roermund PM, Picavet HS (2010) Trends in the number of knee and hip arthroplasties: considerably more knee and hip prostheses due to osteoarthritis in 2030. Ned Tijdschr Geneeskd 154:A1534
Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ (2009) Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 467(10):2606–2612
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
King JC, Manner PA, Stamper DL, Schaad DC, Leopold SS (2011) Is minimally invasive total knee arthroplasty associated with lower costs than traditional TKA? Clin Orthop Relat Res 469(6):1716–1720
Noble JW Jr, Moore CA, Liu N (2012) The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty 27(1):153–155
Watters TS, Mather RC 3rd, Browne JA, Berend KR, Lombardi AV Jr, Bolognesi MP (2011) Analysis of procedure-related costs and proposed benefits of using patient-specific approach in total knee arthroplasty. J Surg Orthop Adv 20(2):112–116
Lewis S (1984) Prospective pricing and DRGs. West J Med 140:123–128
Ben-Arieh D, Qian L (2003) Activity-based cost management for design and development stage. Int. J. Prod Econ 83:169–183
Healy WL, Rana AJ, Iorio R (2011) Hospital economics of primary total knee arthroplasty at a teaching hospital. Clin Orthop Relat Res 469(1):87–94
Goodacre S, McCabe C (2002) An introduction to economic evaluation. Emerg Med J 19:198–201
Lombardi AV, Berend KR, Adams JB (2008) Patient-specific approach in total knee arthroplasty. Orthopedics 31:927–930
Conflict of interest
Carsten O. Tibesku is a consultant for Smith& Nephew Orthopaedics AG, Baar, Switzerland. No financial support was received for preparation of this manuscript. Pamela Hofer, Wesley Portegies and Peter Fennema were employed by Smith & Nephew during the development of the ABC model. No other conflicts of interest are declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tibesku, C.O., Hofer, P., Portegies, W. et al. Benefits of using customized instrumentation in total knee arthroplasty: results from an activity-based costing model. Arch Orthop Trauma Surg 133, 405–411 (2013). https://doi.org/10.1007/s00402-012-1667-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1667-4