Abstract
Introduction
The purpose of this study was to evaluate the clinical effect of medial patellar retinaculum plasty for children and adolescent patients with patellar dislocation.
Materials and methods
A prospective study was performed between October 2005 and December 2009. Sixty-one cases of children and adolescent patients with patellar dislocation were admitted to our study. Twenty-nine patients received medial capsule reefing, of which 13 patients also received lateral retinacular release (LRR) (Group I). Thirty-two patients received medial patellar retinaculum plasty, of which 12 patients also received LRR (Group II). Preoperatively, all patients received magnetic resonance imaging (MRI) to evaluate the injury of medial patellofemoral ligament. And all patients received computed tomography (CT) scans on which the congruence angle (CA) and patellar lateral shift (PLS) could be evaluated with 30° knee flexion. Physical apprehension tests were examined and the redislocation was recorded. In addition, knee function was evaluated using the Kujala score and subjective questionnaires.
Results
Patients were followed up for a mean period of 50 months (25–75 months). For the comparison between the preoperative and postoperative results, the Kujala score improved significantly from 52.3 ± 2.9 to 78.1 ± 3.6 in Group I and from 53.5 ± 3.4 to 82.2 ± 3.4 in Group II (P < 0.05). There was significant difference of CA on CT scans and PLS with a statistical difference between the two groups (P < 0.05). Results of the apprehension test showed that nine patients had patellar lateral shift exceeding 1.5 cm with a soft end point in Group I and two patients had patellar lateral shift exceeding 1.5 cm with a hard end point in Group II (P < 0.05). Moreover, the subjective questionnaire revealed a significant difference of subjective effects between two groups (P < 0.05), including 7 excellent, 10 good and 12 fair in Group I and 18 excellent, 9 good, and 5 fair in Group II.
Conclusion
The medial retinaculum plasty was better than medial capsule reefing in improving the subjective effects and decreasing the rate of patellar instability postoperatively in children and adolescent patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Habitual or recurrent dislocation of patella was common in children and adolescents [1, 3–5, 11, 16, 26], and the reported incidence of this disease was 43 per 100,000 [16]. In the long run, patellar dislocation might result in severe pain, recurrent patellar instability, and even patellofemoral osteoarthritis [1]. Patellar dislocation and recurrent instability were attributed to a series of factors, including genu valgum, hypoplasia of the lateral femoral condyle, patella alta, contracture of the lateral patellar soft tissues, ligament laxity, a laterally located tibial tubercle, abnormal attachment of the iliotibial tract, and vastus medialis (VM) insufficiency [10, 22]. Besides, anatomic and biomechanical study showed that the medial patellofemoral ligament (MPFL) was an important structure as a passive check rein at 20° knee flexion, providing 53–67 % of the medial soft tissue restraint to prevent lateral displacement of the patella and control its tracking [5, 6]. Surgical techniques for the treatment of patellar dislocation could be grouped broadly classified to bony or soft-tissue balancing methods. In children and adolescents with open growth plates, bony procedures were not recommended by most scholars because of the damage to the growth plate and the subsequent deformity. Therefore, medial capsule reefing, as a traditional method of soft-tissue procedures was a widely accepted surgery for children and adolescents with patellar dislocation. However, the medial capsule reefing only fixed the imbrication of the medial capsule to medial patella. A retrospective study by Matthias Buchner et al. [15] reported a rather high recurrent instability rate of 27 % after medial capsule reefing. Patellar dislocation was often accompanied by the MPFL injury in children and adolescents [2]. Although tears of the MPFL which was adjacent to the patellar insertion or in the midsubstance of the medial retinacular complex have been described previously, recent studies have reported that the MPFL injury site was always at or close to its femoral attachment site or there was more than one site of injury [7, 12, 13, 18, 19, 21, 23–25, 27]. The traditional medial capsule reefing could not repair the MPFL injury of its femoral attachment site and midsubstance. MPFL reconstruction was considered as an important technique for patellar dislocation, and there was a low rate of recurrence and good clinical outcome after MPFL reconstruction [7, 12, 17, 23, 24]. However, the MPFL reconstruction was not suitable for children and adolescents because of their open growth plates. In this study, we performed the related anatomical, biomechanical, and magnetic resonance imaging (MRI) research on the basis of the advantages of traditional medial capsule reefing and MPFL reconstruction, and finally designed a new surgery technique—medial patellar retinaculum plasty. This method might decrease the rate of patellar instability postoperatively in children and adolescents, achieving a good clinical effect.
Materials and methods
In this study, patients were selected on the basis of the following: (1) patellar lateral shift exceeding 1.5 cm with a soft end point by the apprehension test; (2) patellar instability were confirmed through measuring the patellar tilt angle (PTA) and the congruence angle (CA) on computed tomography (CT) scans; (3) MRI display the MPFL injury to the femoral insertion or combinations of patellar insertion (Fig. 1). Patients were excluded when they had the following: (1) sulcus angle greater than 150°; (2) tibial tuberosity-trochlear groove (TTTG) distance greater than 15 mm; (3) patella alta (Insall-Salvati index greater than 1.2); (4) with patellar dysplasia grade IV and V (Wiberg classification); (5) concomitant knee cruciate ligament or collateral ligament injury; (6) rheumatoid arthritis, osteonecrosis with cartilage damage greater than grade II.
The diagnosis of patellar dislocation was confirmed by patellar apprehension test, MRI, and the CT scan of patellofemoral joint at 30° knee flexion. In addition, if a CT scan slice of the trochlear groove was overlayed with a CT slice of the proximal tibia showing the tibial tubercle, the trochlear groove tibial tubercle distance (TT-TG) can be determined. PTA was determined by the angle between one line parallelled with the lateral patellar facet and the other line parallelled with the posterior condylar line. A sulcus angle (SA) is formed between the two tangential lines of the joint surface of the medial and the lateral femoral condyles. And the CA is the angle formed between the bisector line of a sulcus angle and the tip–tip line (A tip–tip line connects the tips of the sulcus angle and the patellar ridge). The knee function was assessed with the Kujala score and with a subjective questionnaire.
The CONSORT flow chart of patient selection was shown in Fig. 2. Between October 2005 and December 2009, 61 patients with patellar dislocation in children and adolescents underwent arthroscopically assisted medial capsule reefing or medial patellar retinaculum plasty. With permission of the ethics committees of the Third Hospital of Hebei Medical University, randomization was based on the birth year of patients (even/odd). There were 29 cases with medial capsule reefing, of which 13 cases also received lateral retinacular release (LRR) (Group I). There were 32 cases with medial patellar retinaculum plasty, 12 of which also received LRR (Group II). The demographic data on the groups were shown in Table 1.
Surgical technique
With the patient lying supine and under subarachnoid anesthesia, after prepping, arthroscopy was carried out to assess and address any possible chondral lesions and concomitant pathology. The force directed medial shift of the patella less than one-fourth the width of the patella indicates an overtension of the lateral retinaculum structure, and an LRR was then performed [28].
In Group I, an LRR was performed under arthroscopy in 13 patients. After removing the arthroscope, an incision was made on the anteromedial aspect of patella. The subcutaneous tissue and deep fascia were dissected so as to expose the quadriceps muscle, the medial retinaculum of the patella, and the patellar tendon. The medial retinaculum and medial capsule were dissected thoroughly from the patellar tendon to the junction point of VM and vastus intermedius, and the imbrication of the medial capsule was sutured to the medial patella. After evaluating the patella activity by hand, the congruence of patellofemoral joint was observed with the knee at complete extension and the tracking of patella was observed during flex motion under arthroscope. Finally, the tension of medial capsule was adjusted according to the tracking of patella.
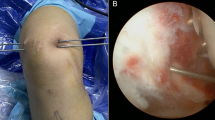
In Group II, an LRR was performed under arthroscopy in 12 cases. After removing the arthroscope, an incision was made on the anteromedial aspect of patella. The subcutaneous tissue and deep fascia were dissected so as to expose the VM, the medial retinaculum of the patella, and the patellar tendon. A longitudinal dissection was made along the medial border of patella so as to separate the VM and medial retinaculum from the patella. And then, a transverse dissection was made along the junction line of VM and medial retinaculum to the medial femoral condyle to separate the two adjacent sections. Then the medial retinaculum including MPFL was stretched so as to evaluate the integrity of femoral attachment site. The patients who had a hard end point of the medial retinaculum were excluded from our study. A 3-cm-length longitudinal incision was made over the MPFL femoral insertion. Then a transverse dissection was made to divide the medial retinaculum into two parts: the distal part, including both medial retinaculum and MPFL, and the proximal part, only including medial retinaculum. The distal part of medial retinaculum was sutured proximally medial femoral condyle. The proximal part of retinaculum was sutured distally over the retensioned distal part of medial retinaculum. Then the aforementioned separated medial retinaculum was proximally and laterally sutured to near the upper pole of the patella temporarily. The VM was then sutured distally and laterally to the midline of patella temporarily. After evaluating the patella activity by hand, the congruence of patellofemoral joint was observed with the knee at completely extension and the tracking of patella was observed during flex motion under arthroscope (Fig. 3). Based on the tracking of patella, the tension of medial retinaculum and VM was adjusted and the two sections were sutured together in the medial side of patella. Finally, the overlapped tissues (including the medial retinaculum, VM and the proximal and distal section of medial retinaculum) were sutured together by PDS-1 sutures (Fig. 4).
a The transverse incision which was made at the junction of the vastus medialis obliquus and the medial retinaculum of patella. VMO vastus medialis oblique. b The femoral attachment of MPFL was dissected. c A transverse dissection was made to divide the medial retinaculum into two parts: the distal part, including both medial retinaculum and MPFL, and the proximal part, only including medial retinaculum. d The distal part of medial retinaculum advanced proximally and rear to medial femoral condyle, the proximal part of retinaculum, and then advanced distally over the retensioned distal part of medial retinaculum. e The isolated medial retinaculum of the patella site advanced proximally and laterally to near the upper pole of the patella, and then the vastus medialis advanced distally and laterally to the patella
Postoperative rehabilitation program and follow-up
Quadriceps setting exercises and straight leg raising exercises were encouraged from the first day following surgery. Walking with partial weight bearing on two crutches and knee flex activities were also permitted within tolerance and gradually progressed from the day following surgery. After 1 week, knee flexion up to 30° was obtained. After 2 weeks knee flexion up to 90° was obtained. After 4 weeks, full weight bearing was allowed. Patients who achieved enough quadriceps strength, stability of patella, and sufficient range of motion were allowed to begin normal daily living and jogging 2 months after surgery and athletic exercises 3 months after surgery. During the follow-up period, the patellofemoral joint was evaluated with CT scans. The apprehension test was conducted and the redislocation was recorded. And the knee function was determined by the Kujala score and with a subjective questionnaire.
Statistics analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 16.0 (SPSS, Chicago, IL, USA). Kolmogorov–Smirnov test was used to test the normality of the numeric data. Levene’s test was applied to assess homogeneity of variance between data. All numeric variables showed normal distribution or equal variance. The differences between the two groups (TT-TG, CA, PTA, SA, PLS, Kujala score) were analyzed with two-sample t test. The apprehension sign and subjective questionnaire were analyzed with Pearson Chi-square test. Numeric data are showed as mean ± standard deviation (SD); categoric data are shown as numbers with percentages. A P value of less than 0.05 was considered statistically significant.
Results
MRI scans showed that all patients had MPFL injury near the femoral insertion and part of them were accompanied by patellar insertion. In addition, there were no differences in preoperative data between the two groups (Table 1). Four patients including two in Group I and two in Group II were lost to follow-up after 1 year, and the remaining 61 patients including 29 in Group I and 32 in Group II were included in the final analysis. Patients were followed up for an average period of 50 months (25–75 months). On CT scans, the CA and patellar lateral shift was significantly different between the two groups at the last follow-up (Fig. 5). There were nine patients with recurrent patellar dislocation in Group I. However, two patients in Group II had a patellar lateral shift that exceeded 1.5 cm with a hard end point for the apprehension test, with a significant difference between the two groups (P < 0.05). The Kujala score had significantly improved after surgery, from 52.3 ± 2.9 to 78.1 ± 3.6 in Group I and from 53.5 ± 3.4 to 82.2 ± 3.4 in Group II. The subjective questionnaire revealed that there were 7 (21.1 %) excellent results in Group I and 18 (56.3 %) in Group II, 12 (41.4 %) patients in Group I and 5 (15.6 %) patients in Group II answered fair. The Kujala score with a statistically significant difference between the two groups and the subjective knee function in Group II was better than that in Group I (Table 2). Five patients (three in Group I and two in Group II) initially complained of weakness after the operation when extending the knee; three knees (one in Group I and two in Group II) had mild anterior knee pain and limitation in flexed-knee activities. However, the muscle strength was recovered and all the symptoms disappeared after 8–9 weeks of exercise. No extension nor flexion deficit of 5° or more was observed in the range of knee motion compared with the contralateral knee at the final evaluation.
Discussion
The aim of this study was to determine the clinical effect of medial capsule reefing and medial retinaculum plasty for the patients with patellar dislocation. The Kujala score and subjective questionnaires were used to evaluate the knee function. Physical apprehension tests were examined and the redislocation recorded. The results revealed that the medial retinaculum plasty was better than medial capsule reefing in improving the subjective effects and decreasing the rate of patellar dislocation in children and adolescents.
The related anatomic and biomechanical study showed that the MPFL was an important structure as a passive check rein at 20° knee flexion, providing 53–67 % of the medial soft tissue restraint to prevent lateral displacement of the patella and control its tracking [5, 6]. Lesions of MPFL could be found in almost all of the cases [18]. Therefore, it was important to repair the medial retinaculum and MPFL for patellar dislocation.
MPFL reconstruction was considered as an important operation for patellar dislocation, and there was a low rate of recurrence and good clinical outcome after MPFL reconstruction [7, 12, 17, 23, 24]. However, in the adolescents with open growth plates, this surgical technique was not recommended by most scholars because of the damage to the growth plate and the subsequent deformity. Therefore, medial capsule reefing, as a traditional method of soft-tissue procedure, was a widely accepted surgery for children and adolescents with patellar dislocation. However, a retrospective study by Matthias Buchner et.al [15] reported a rather high recurrent instability rate of 27 % after medial capsule reefing. Hawkins et al. [10] reported that despite conservative or immediate surgical stabilization, 30–50 % of patients will continue to have symptoms of instability or anterior knee pain, or both.
In addition, according to the results of the knee joint MRI, MPFL injury occurred not only in patellar insertion, but also at femoral attachment, and even at both the patellar and femoral attachments. Peter Balcarek et al. [2] reported that the MPFL injury occured in 98.6 % of the patients with patellar dislocation. In addition, Kepler et al. [11] reported that the MPFL injury was isolated to the patellar attachment in 61 % of children and adolescent patients and to the femoral attachment in 12 %. Moreover, 12 % of children and adolescent patients had injury at both the patellar and femoral attachments.
However, the traditional method of medial capsule reefing only sutured the imbrication of the medial capsule to the medial of patella. The MPFL injury at femoral attachment site and (or) midsubstance were not repaired. Therefore, the integrity of medial retinaculum and MPFL was not restored. In this new surgical technique, we not only repaired the medial patella injury, but also sutured the soft tissue including MPFL and medial retinaculum near its femoral attachment site proximally and posteriorly to medial femoral condyle. The MPFL injury at femoral attachment site was also repaired so as to keep the integrity of the MPFL and medial retinaculum.
For the medial capsule reefing, the imbrication of the medial capsule was sutured to medial patella alone, only shortening the lengths of MPFL and medial retinaculum to increase the tension of the medial retinaculum. The tension of medial retinaculum together with MPFL might gradually weaken as time went on, leading to failure finally. However, in our new surgical technique, the overlapped tissues were sutured together (including the medial retinaculum, VM, and the proximal and distal section of medial retinaculum), so as to increase the thickness of medial retinaculum and MPFL, consequently increasing the strength of retinaculum and MPFL. The medial retinaculum was sutured proximally and laterally to near the upper pole of the patella, further shortening the length of retinaculum and MPFL, increasing their tension.
Vastus medialis was an important dynamic structure in preventing patella lateral translation. A notable change was observed in the restraining force-flexion angle curve with the VM relaxed, with a minimum at 30° knee flexion [8]. In addition, Goh et al. [9] reported that the absence of VMO tension resulted in a lateral displacement of the patella in a cadaveric study. Therefore, restoring the function of VMO was very important. Panagiotopoulos et al. [20] revealed that the function of the strong “meshing” fibers from the VMO to the MPFL close to its patellar insertion by the VMO “dynamizes” the MPFL, so MPFL provides both static and dynamic stability for patella.
Compared with medial capsule reefing, the lower border of VM was distally and laterally sutured to the middle line of the patella, not only to restore the tension of VMO, but also to strengthen the dynamic stability for medial of patella. And we overlapped VM with the medial retinaculum then sutured the two overlapping tissues. In this way, we could further strengthen and “reconstruct” the static stability of MPFL and medial retinaculum. The overlapping tissues from MPFL and VMO formed a strengthened anatomical structure to keep joint dynamic-static stability.
LRR was also often performed in patients with an overtension of the lateral retinaculum structure. In the present study, LRR was applied to 25 (40.98 %) cases in all of patients. A previous study showed LRR had no obvious effect on treating patella dislocation [14]. Therefore, it was a limitation of our study not to compare the difference between LRR(+) and LRR(−) groups.
To our knowledge this is the first time that medial patellar retinaculum plasty for patellar dislocation in children and adolescents is described. In comparison with MPFL reconstruction, this surgical technique avoided the damage to the growth plate. Compared with traditional medial capsule reefing, medial patellar retinaculum plasty repaired the MPFL injury at both patellar attachment and femoral attachment sites so as to keep the integrity of medial retinaculum and MPFL. In addition, the overlapped tissues were sutured together (including the medial retinaculum, VM and the proximal and distal section of medial retinaculum) so as to increase the strength of retinaculum and MPFL. This technique also further strengthened and “reconstructed” the static stability of both MPFL and medial retinaculum, together with the overlapping tissues from MPFL and VMO, finally improving the joint dynamic-static stability structure. In conclusion, medial patellar retinaculum plasty for patellar dislocation in children and adolescents might achieve good clinical effects, with a good congruous patellofemoral joint and good knee function.
References
Arendt EA, Fithian DC, Cohen E (2002) Current concepts of lateral patella dislocation. Clin Sports Med 21:499–519
Balcarek P, Ammon J, Frosch S (2010) Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy 26(7):926–935
Beasley LS, Vidal AF (2004) Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr 16:29–36
Cash JD, Hughston JC (1988) Treatment of acute patellar dislocation. Am J Sports Med 16:244–249
Conlan T, Garth WP, Lemons J (1993) Evaluation of the medial soft tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75:682–693
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Elias DA, White LM, Fithian DC (2002) Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 225:736–743
Farahmand F, Naghi Tahmasbi M, Amis A (2004) The contribution of the medial retinaculum and quadriceps muscles to patellar lateral stability—an in vitro study. Knee 11(2):89–94
Goh JC, Lee PY, Bose K (1995) A cadaver study of the function of the oblique part of vastus medialis. J Bone Joint Surg Br 77:225–231
Hawkins RJ, Bell RH, Anisette G (1986) Acute patellar dislocations: the natural history. Am J Sports Med 14:117–120
Kepler CK, Bogner EA, Hammoud S, Malcolmson G, Potter HG, Green DW (2011) Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med 39(7):1444–1449 (Epub 2011 Mar 3)
Kirsch MD, Fitzgerald SW, Friedman H, Rogers LF (1993) Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol 161:109–113
Lance E, Deutsch AL, Mink JH (1993) Prior lateral patellar dislocation: MR imaging findings. Radiology 189:905–907
Lattermann C, Toth J, Bach BR Jr (2007) The role of lateral retinacular release in the treatment of patellar instability. Sports Med Arthrosc 15(2):57–60
Buchner M, Baudendistel B, Sabo D (2005) Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med 4:62–66
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14:513–515
Nomura E, Horiuchi Y, Kihara M (2000) A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patella dislocation. Knee 7(4):211–215
Nomura E, Horiuchi Y, Inoue M (2002) Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee 9:139–143
Nomura E (1999) Classification of lesions of the medial patellofemoral ligament in patellar dislocation. Int Orthop 23:260–263
Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G (2006) Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 14(1):7–12
Quinn SF, Rose PM, Brown TR, Demlow TA (1994) MR imaging of the patellofemoral compartment. Magn Reson Imaging Clin N Am 2:425–440
Rorabeck CH, Bobechko WP (1976) Acute dislocation of the patella with osteochondral fracture. J Bone Joint Surg Br 58:237–240
Sanders TG, Morrison WB, Singleton BA, Miller MD, Cornum KG (2001) Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr 25:957–962
Spritzer CE, Courneya DL, Burk DL Jr, Garrett WE, Strong JA (1997) Medial retinacular complex injury in acute patellar dislocation: MR findings and surgical implications. AJR Am J Roentgenol 168:117–122
Sillanpää PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamäki H (2009) Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. Am J Sports Med 37:1513–1521
Vähäsarja V, Kinnunen P, Lanning P, Serlo W (1995) Operative realignment of patellar malalignment in children. J Pediatr Orthop 15:281–285
Virolainen H, Visuri T, Kuusela T (1993) Acute dislocation of the patella: MR findings. Radiology 189:243–246
Watanabe T, Muneta T, Ikeda H et al (2008) Visual analog scale assessment after medial patellofemoral ligament reconstruction: with or without tibial tubercle transfer. J Orthop Sci 13:32–38
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ma, Lf., Wang, Ch., Chen, Bc. et al. Medial patellar retinaculum plasty versus medial capsule reefing for patellar dislocation in children and adolescents. Arch Orthop Trauma Surg 132, 1773–1780 (2012). https://doi.org/10.1007/s00402-012-1598-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1598-0