Abstract
Introduction
Cerclages regain interest due to a rising number of periprosthetic fractures. The contact distribution at the circumferential cerclage-bone interface is still unknown. Local interface pressure depends on the amount of contact area. Cortical damage at the interface would provoke cerclage loosening. Therefore, the contact area, the bone pressure along the interface and the cortical resistance underneath loaded cerclages were determined in an ex vivo model.
Materials and methods
Human diaphyseal femoral bone was used with differing cross-sectional geometry. Bone contact points of fixed 1.5 mm wire and 1.7 mm cable cerclages were identified from axial radiographs. Pressure distribution at the cerclage-bone interface was recorded with a pressure-measuring film using a distraction setup with two cortical half shells. Bone shells with installed cerclages were separated with up to 400 N force and were subsequently analyzed histologically to detect cortical damage.
Results
Both cerclage types exhibited a point contact fixation with non-loaded spanned zones in-between. Cables cover larger contact areas. Both cerclages exhibited an inhomogeneous interface pressure distribution depending on the bone surface geometry. Histology revealed intact cortical bone without cortical affection after loading of both cerclage types.
Conclusion
Point contact fixation of the cerclages installs non-loaded, spanned zones where the periosteum is not compressed, rendering a strangulation of the blood supply unlikely. Cortical bone withstands static concentric pressure produced by the cerclage. Cortical groove formation is attributed to instability under functional load and not to weakness of the cortex itself.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerclages are widely used in small animal surgery [1], but as a stand-alone implant for human long bones, they are too weak to fulfill the requirements of functional aftercare [2]. The unsatisfactory results of cerclages as primary fixation devices such as nonunions or bone resorption at cerclage contact sites are mainly evoked by an increased instability at the fracture site [2, 3]. However, the belief of a strangled blood supply owing to cerclage application is still present [4, 5]. Nowadays the situation has changed especially due to a rising number of periprosthetic fractures, because implants penetrating the medullary cavity are of restricted use since the intramedullary canal is blocked by the prosthesis stem.
The stability of a cerclage as a circumferential and extraosseous fixation device depends on its lasting tension, so that an investigation on the cerclage bone interface mechanics helps evaluating and explaining the biological aspects. Since the periosteum plays an essential role in fracture healing, especially when the intramedullary blood supply might be affected by an implant [6], a possible impairment of the periosteum by the cerclage is considered of importance. Blood flow is impeded at the bone contact area on an implant [7]. Plates with reduced bone contact surface show less early temporary bone porosity due to less damage to the blood supply [8]. Analogical to the low contact plates, cerclages with a cogwheel-like undersurface were designed to minimize the contact area at the cerclage-bone interface [9, 10]. They failed wide clinical application due to their insufficient fixation properties. In vivo studies revealed no adverse effect of cerclages on bone viability and periosteal blood supply when applied without damage to large vessels [2, 3, 9, 11]. Interestingly, in vivo experiments exhibited no difference in fracture healing, irrespective of whether the cerclage was placed below or above the periosteum [12]. Devitalized cortical bone segments, fixed by cerclages, showed a complete revascularization [13]. A rationale for the discrepancy between observed experimental phenomena and surgical perception is still lacking. The influence of bone geometry on cerclage application and interface contact area had not been focused on yet. The normal anteroposterior and lateral radiographs provide only limited information on the contact zones between the bone and the cerclage. Computed tomography slices are disturbed by metal artifacts of the cerclage.
Load transmission from the cerclage to the bone has been widely investigated for tension band wiring [14, 15], but there is little information available on the load transmission area of cerclages as centripetal load carriers on the diaphysis of a bone.
Therefore, the contact area at the circumferential cerclage-bone interface was determined by axial radiographs from a section of the femoral shaft and the pressure distribution at the cerclage-bone interface was determined with a pressure measurement film, being widely used for intraarticular pressure distribution evaluation [16] or pressure formation detection within a fracture gap [15]. The influence of loaded cerclages on the ex vivo cortical surface was examined histologically. This paper will give another approach to better understand the mechanobiology of cerclages.
Materials and methods
Fresh-frozen (−20 °C) human femoral diaphyseal bones were used in this study. Soft tissues were removed prior to testing and bones were kept moist with physiologic saline solution. Two different bone geometries, representing the anterior and posterior aspects of the femoral shaft were chosen. Fragments of 25-mm-length were cut from the mid-diaphysis of the femur and the intramedullary canal was reamed up to 20 mm diameter. The fragment was cut lengthwise into two half shells. Two different cerclages were investigated: wire Ø 1.5 mm (ref. nr. 291.130, Synthes GmbH, Solothurn, Switzerland) and cable Ø 1.7 mm (ref. nr. 298.801). Axial radiographs were taken from a femoral shaft segment with fixed cerclages to visualize the cerclage/bone contact zones.
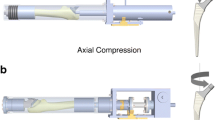
The prepared diaphyseal bone shells were mounted on two metal half cylinders with a diameter of 20 mm forming a full circle. The upper metal half cylinder was rigidly attached to the actuator and the lower half cylinder was affixed to the 25-kN load cell of a servo-hydraulic testing system (Bionix 858.20; MTS Systems, Eden Prairie, MN, USA) (Fig. 1). For assessment of the radial pressure underneath the cerclage, a pressure sensor (Model 5033, TekScan Inc., South Boston, MA, USA) was placed on the upper bone shell, covering approximately a third of the total bone circumference. Pressure distribution was registered with n = 6 repeated measurements per group. The setup allowed controlled separation of the bony half-shells and measurement of the resulting distraction force as described previously [17]. The cerclages were fixed around the cortical half shells. Subsequently the constructs were loaded in a quasi-static, non-destructive range at 40 N/s to a plateau of 200 N load. The pressure distribution at the cerclage-bone interface along the cerclage was recorded during the load plateau. A maximum load of 200 N was chosen to allow a comparison between the different cerclage types, while assuring a strictly linear elastic behavior of the cerclage.
Test setup. Two cortical half shells of human femoral shaft were mounted on two metal half cylinders. The distal half cylinder is connected to the load cell, and the upper half cylinder is connected to the actuator of the test system. The pressure measurement film was fixed on the upper cortical half shell for pressure registration at the bone-cerclage interface. The figure shows a mounted 1.7 mm cable cerclage before load application. Arrows indicate the direction of the applied load. The insert displays a 1.5 mm wire cerclage, installed on the test setup before load application
Bone specimens without underlying pressure sensor were loaded up to 400 N and subsequently histologically examined to detect cortical surface affection using a basic-fuchsin staining.
For statistical analysis of the pressure distribution a binary approach was chosen by dividing the cerclage-bone area into loaded and unloaded regions. Loaded contact was defined at ≥0.5 MPa contact pressure. Analysis of the pressure distribution was done by a custom-made software routine (Matlab R2010a; The Mathworks, Natick, MA, USA). Statistical analysis was performed with the use of SPSS software (SPSS 19.0; SPSS, Chicago, IL, USA). Data did not reveal normal distribution within each group as indicated by the Shapiro–Wilk Test. For the detection of significant differences between the two cerclage types regarding percentage of loaded interface zones, the Mann–Whitney U test was used. Significance was defined at p < 0.05.
Results
Cerclage-bone contact area is dependent on bone geometry. Two investigated bone shapes are illustrated in Figs. 2, 3. One characteristic section shows a plateau to be spanned by the cerclage; the other one incorporates a hump as present in various anatomical locations. On the bony section with a plateau (Fig. 2), the cable cerclage generated pressure on 52 % ± 2 of the spanned area whereas the wire cerclage generated pressure on 39 % ± 1 of the spanned area. This difference was significant between the two cerclage type groups (p = 0.003). On the bony section with the hump (Fig. 3) the cable cerclage generated pressure on 31 % ± 3 of the spannend area, whereas the wire cerclage generated pressure on 29 % ± 0.1 of the spanned area with no significant difference between the two cerclage type groups. The non-circular geometry of the femoral shaft leads to a spanning of the cerclage from deflection point to deflection point with non-loaded zones in between (Fig. 4). On the femoral shaft, cerclages provide a point-contact fixation. Histological evaluation of the cerclage-bone interface after load application revealed an intact cortical surface with no cortical affection (Fig. 5).
Mean pressure distribution along the cerclage–bone interface. Pressure distribution underneath wire and cable cerclages is displayed. Correspondent bone surface geometry is indicated below. In concordance with the radiographs, cerclage cables exhibit a more equalized pressure distribution with an overall larger loaded area compared with the cerclage wires, where the load concentrates mainly at the deflection points of the cerclage. Both cerclages show an overspan effect with a non-loaded area in-between. Pressure distribution underneath the cerclage is dependent on its flexibility and on bone surface geometry
Mean pressure distribution along the cerclage bone interface. Pressure distribution underneath wire and cable cerclages is displayed. Correspondent bone surface geometry is indicated below. Compared with Fig. 2, the bone provides an eminence in the center, where both cerclages are deflected and the pressure is concentrated. Similar to the bone geometry of Fig. 2, cable cerclages exhibit a more spread pressure distribution with a lower peak, compared with the less flexible wire cerclages, where the pressure is concentrated on a smaller area
Axial X-rays of femoral shaft with fixed cerclages for cerclage-bone interface visualization. a 1.5 mm wire cerclage wrapped around the femur and closed by a twist. Arrows indicate point contact fixation of the cerclage. In the radiolucent space at the cerclage-bone interface, no cerclage-bone contact is given and periosteum will be not affected therein. b 1.7 mm cable cerclage wrapped around the bone and tightened before crimp closure. Due to its higher flexibility, bone contact areas are larger compared with the wire cerclages. Comparable to wire cerclages, cables also provide a point-contact fixation. The arrow indicates a radiolucent space at the cerclage-bone interface, with no cerclage-bone contact
Fluorescence microscopy of basic fuchsin stained sections of femoral shaft after cerclage application and subsequent loading with 400 N. Loaded cortex areas underneath the cerclage are shown. Cortex remained intact after 1.5 mm wire (a) and 1.7 mm cable (b) cerclage application and subsequent loading, indicating that cortical bone withstands high forces without being affected
Discussion
This study investigated on the pressure distribution at the cerclage-bone interface of the femoral shaft, which is related to the circumferential geometry of the bone. Due to the fact that the femoral shaft does not represent an idealized round tube, pressure measurement underneath the cerclage revealed an uneven pressure distribution with peak loaded areas, especially the deflection points of the cerclage and low to non-loaded areas, in particular the spanned bone sections, indicating a point-contact fixation. The concept of point contact fixation was successfully introduced in plate osteosynthesis to ameliorate the blood supply of the underlying bone. The axial radiographs and pressure distribution profile at the cerclage-bone interface endorse this concept, too. In lag screw or compression plate fixation, where high local pressure is applied on the screw hole or at the plate-bone contact point, no pressure-induced bone necrosis has been reported either [10, 18, 19]. Living bone can tolerate static compression up to the limit of mechanical strength but not exceeding it [2, 19]. In our study, static loading of the bone before histological examination was performed with a maximum load of 400 N to prevent unraveling and loosening of the wire cerclage. The histologic examination revealed no bone surface affection by the cerclage, indicating no groove formation on the bone as reported by Baumann [20].
As implication to clinical practice, the cortex withstands static concentric pressure and it is unlikely to produce a cortical surface fracture by cerclage tightening, when the fracture is properly reduced. Furthermore, no grade cutting of the cerclage into the cortical bone has to be expected in a congruently reduced fracture. As already discussed by Jones [21], the groove formation is not induced by the weakness of the cortex itself, but the micromovement between the cerclage and the bone at high strain induces the bone loss. Bone surface resorption can be evoked by the so-called loose-lock stability [2], which is typically observed in loosened cerclages. In vivo, no cortical bone resorption was seen under well-tightened cerclages [22]; in contrast, a bony ingrowth in terms of callus formation was found [23]. In vivo experiments [23] with a spring-locked cerclage providing a constant tension revealed no shortening travel of the cerclage during fracture healing, which might have occurred during cortical bone resorption and grade cutting. Analyzing the radiographs from the case reports on cerclage pressure-induced bone necrosis [4, 5], in all cases fracture instability due to insufficient reduction or fixation could be detected, supporting the motion-induced bone necrosis theory [2].
On the bony section with plateau, wire cerclages exhibited significantly less loaded zones compared with cable cerclages, which could be explained by the higher flexibility of cable cerclages leading to a closer adaption to the bone surface. The bony section with hump revealed no significant difference in the percentage of loaded zones in between the two cerclage types, demonstrating that the spanning effect also exists for cables. With a more flexible construct like the cable cerclage, fracture reduction and its maintenance might be easier to achieve. A wire as a stiffer construct will deform with loss of stability; the cable offers to a certain degree an elastic element which to a certain range compensates the loss of stability and shifts it towards a reversible displacement, the so-called relative stability.
Concerning the footprint of cerclages, its structure is of importance. In the cross-sectional view, solid wires show a circular surface, whereas cables, consisting of wire bundles including several strands, lead to half the cross-sectional contact area of solid wires as shown in histological preparations of Fernandez et al. [2]. They also observed that half the amount of periost was affected by a cable cerclage compared with a solid wire, but in both cases, in accordance to our histologic findings and to Franke et al. [23], the underlying cortical surface was intact and not affected by the cerclage. Our pressure-measuring film was not sensitive enough to detect these differences along the cerclage in the micrometer range. Similar to our results of interface pressure distribution along the cerclage, the histological preparation of the in vivo study of Fernandez et al. [2] revealed a small area between wire cerclage and bone, filled with soft tissue, which corresponds to the non-loaded zones detected in our study, where the cerclage spans the bone without contact.
Conclusion
Cerclage-bone interface contact is dependent on surface geometry of the bone. On the femoral shaft, cerclages provide a point contact fixation, a blood-supply preserving principle, which is already well established in plate osteosynthesis.
Cortical damage and bone resorption have to be attributed to micromotion, since cortical bone is stable enough to withstand the centripetal forces of the loaded cerclage without being damaged. The findings suggest reconsidering cerclage as an additional fixation tool, particularly for periprosthetic fracture treatment.
References
Johnson AL, Houlton JEF, Vannini R (1989) AO principles of fracture management in the dog and cat. Thieme, Stuttgart
Perren SM, Fernandez Dell’Oca A, Lenz M, Windolf M (2011) Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir Orthop Traumatol Cech 78(3):190–199
Eitel F, Dambe LT, Klapp F, Schweiberer L (1976) Vascularization of diaphyseal long bones by cerclage. Unfallheilkunde 79(2):41–44
Cebesoy O, Subasi M, Isik M (2011) Cerclage cable in fracture: frustration or necessity? Int Orthop 35(5):783–784
van Steijn MJ, Verhaar JA (1997) Osteonecrosis caused by percutaneous cerclage wiring of a tibial fracture: case report. J Trauma 43(3):521–522
Macnab I, De Haas WG (1974) The role of periosteal blood supply in the healing of fractures of the tibia. Clin Orthop Relat Res 105:27–33
Gautier RP, Perren SM (1991) Die Reaktion der Kortikalis nach Verplattung—eine Folge der Belastungsveränderung des Knochens oder Vaskularitätsprobleme? In: Die Plattenosteosynthese und ihre Konkurrenzverfahren. Springer, Heidelberg, pp 21–37
Perren SM (2002) Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br 84(8):1093–1110
Nyrop KA, DeBowes RM, Ferguson HR, Leipold HW, Wilson JW, Guffy MM (1990) Vascular response of the equine radius to cerclage devices. Vet Surg 19(4):249–253
Windolf M, Perren SM (2012) Mechanobiology. In: Babst R, Bavonratanavech S, Pesantez R (eds) Minimally invasive plate osteosynthesis. 2nd expanded edn. Thieme, Stuttgart, in press
Rhinelander FW, Stewart CL (1983) Experimental fixation of femoral osteotomies by cerclage with nylon straps. Clin Orthop Relat Res 179:298–307
Wilson JW (1987) Effect of cerclage wires on periosteal bone in growing dogs. Vet Surg 16(4):299–302
Klapp F, Eitel F, Dambe LT, Schweiberer L (1976) Revascularization of devitalized cortical segments under stabilizing encircling wires. Langenbecks Arch Chir Suppl, pp 303–306
Brill W (1987) Morphologic analysis of endoprosthesis materials with scanning electron microscopy. Z Orthop Ihre Grenzgeb 125(5):553–558
Wilson J, Bajwa A, Kamath V, Rangan A (2011) Biomechanical comparison of interfragmentary compression in transverse fractures of the olecranon. J Bone Joint Surg Br 93(2):245–250
Krause FG, Sutter D, Waehnert D, Windolf M, Schwieger K, Weber M (2010) Ankle joint pressure changes in a pes cavovarus model after lateralizing calcaneal osteotomies. Foot Ankle Int 31(9):741–746
Wähnert D, Lenz M, Schlegel U, Perren S, Windolf M (2011) Cerclage handling for improved fracture treatment. A biomechanical study on the twisting procedure. Acta Chir Orthop Traumatol Cech 78(3):208–214
Cordey J, Blumlein H, Ziegler W, Perren SM (1976) Study of the behavior in the course of time of the holding power of cortical screws in vivo. Acta Orthop Belg 42(1):75–87
Perren SM, Huggler A, Russenberger M, Allgöwer M, Mathys R, Schenk R, Willenegger H, Müller ME (1969) The reaction of cortical bone to compression. Acta Orthop Scand Suppl 125:19–29
Baumann E (1956) The material to be used for cerclage of bones. Schweiz Med Wochenschr 86(20):533–534
Jones DG (1986) Bone erosion beneath partridge bands. J Bone Joint Surg Br 68(3):476–477
Leemann R (1954) Indications for the technic of cerclage in leg fractures. Helv Chir Acta 21(5–6):480–492
Franke D, Glatz R, Hennig K, Georgi P, Krempin B (1981) Theoretical basis and animal experiments to demonstrate a new method of bone-wiring (cerclage) using a diffraction-free-wire-fixation. Unfallheilkunde 84(8):338–344
Acknowledgments
We thank Ursula Eberli, MSc, for her excellent technical assistance and Dirk Nehrbass, DVM and Mauro Bluvol for the brilliant histological images.
Conflict of interest
The authors are not compensated and there are no other institutional subsidies, corporate affiliations, or funding sources supporting this work unless clearly documented and disclosed. Implants were kindly donated by Synthes GmbH, Solothurn, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was performed at the AO Research Institute Davos, Switzerland.
Rights and permissions
About this article
Cite this article
Lenz, M., Perren, S.M., Gueorguiev, B. et al. Underneath the cerclage: an ex vivo study on the cerclage-bone interface mechanics. Arch Orthop Trauma Surg 132, 1467–1472 (2012). https://doi.org/10.1007/s00402-012-1572-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1572-x