Abstract
Purpose
Implant-related infections are disastrous complications in the clinic, and there are no effective therapies. In this preliminary study, gentamicin-loaded coating on titanium implants was prepared using the electrospinning technique, and some properties of the coating titanium implants were studied.
Methods
We adopted the electrospinning technique to prepare gentamicin-coated titanium implants. The surface structure of the coating implants was observed using scanning electron microscope. An elution study was performed to determine the release behavior of the gentamicin from the coating. The antibacterial efficacy and quantitative analysis of the bacterial adhesion of Staphylococcus aureus were evaluated in vitro, and the cytotoxicity of the coated titanium implants on osteoblasts was investigated in vitro.
Results
The morphology of the gentamicin-coated titanium implants exhibited nanofibers, and the release of gentamicin showed an initial gentamicin burst followed by a slow release. The gentamicin-coated titanium implants had a persistent antibacterial efficacy for 1 week and significantly reduced the adhesion of the Staphylococcus aureus compared with bare titanium implants in vitro. There was no cytotoxicity observed in vitro for the gentamicin-coated implants.
Conclusion
The gentamicin-coated titanium implants, which were prepared using an electrospinning technique, present many advantages and may be considered to prevent and treat the implant-related infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the development of the economy and the improvement of medical equipment, implants such as K-wires, titanium plates and prosthetic joints are increasingly being used in trauma and orthopedic surgery. There will likely be a significant and continued increase in the use of this type of medical equipment due to the ageing of western populations [1, 2].
An increased risk of infection related to equipment implantation has been observed [3, 4]. Infection, although uncommon, is the most disastrous complication because it causes many serious consequences, such as prolonged hospitalization, poor functional outcome, sepsis, and even death [2, 5]. There are no effective treatment options for implant-related infection, except the removal of the implants [6]. Although antibiotics can be administered systemically as part of routine clinical therapy, a high level of the drug may not be achieved locally with systemic administration [2, 7]. For this reason, local application of antibiotics has become more necessary.
Electrospinning is an effective technique that utilizes electrical forces to produce ultrafine polymeric fibers with diameters from the nanometer to micrometer range [8]. These fibers have been successfully applied in drug delivery, wound dressing, tissue engineering scaffolds and other applications because of their highly porous structure, high-specific surface area and high functionality [9–11]. In addition, electrospinning is cost-efficient and can be easily employed in laboratory and industrial settings [8]. Due to the above-mentioned advantages, there has been a tremendous increase in research and commercial attention to this technique in the last decade.
This preliminary study adopted an electrospinning technique to prepare an antibiotic coating on the surface of a three-hole titanium plate. Experiments were then performed to examine the following: (1) the amount of the antibiotic, gentamicin, contained in the coating and on the surface structure of the coated implants; (2) the in vitro release behavior of the antibiotic from the coated implants; (3) the antibacterial efficacy and bacterial adhesion of the coated implants in vitro; and (4) the cytotoxicity of the coated implants in vitro.
Methods
Coating procedure
An electrospinning technique was used to prepare an antibiotic coating on three-hole titanium implants (Health Medical Treatment Apparatus Co., Ltd. Suzhou, China). The electrospinning apparatus, supplied by the State Key Laboratory of Bioelectronics, School of Biological Science and Medical Engineering, Southeast University, Nanjing, contained a syringe pump, a needle, a high voltage source and an aluminum collecting screen. First, the polymer solutions were prepared, 0.75% (w/v) poly(lactic-co-glycolic acid) (PLGA, LA/GA = 50/50, MW = 80,000 Da, Daigang Biotechnology Co., Ltd., Jinan, China) was combined with 0.75% (w/v) polyethylene oxide (PEO, MW = 1,000,000 Da, Guoren Technical Company, Beijing, China), and dissolved in trifluoroethanol (TFE, Darui Finechemical Co., Ltd., Shanghai, China) and lyophilized gentamicin sulfate (Amresco Inc., Solon, OH, USA) was added (0.4% gentamicin base w/v of the solution). This mixed solution was stirred for 3 h, and then the solution was electrospun at room temperature at a humidity of 40% using a positive voltage of 12 kV. The titanium implants were fixed on the aluminum foil as a collector, and the distance between the spinneret and collector was 15 cm. The flow rates of the solution were controlled using a syringe pump operating at 2.5 ml/h. The gentamicin-coated titanium implants were prepared according to these procedures. The polymer-coated titanium implants were also prepared. All these specimens were subsequently sterilized (25 K-Gray gamma radiation) for the following experiment.
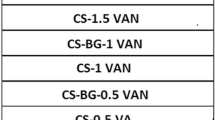
The amount of gentamicin contained within the coating and the surface structure study
Gentamicin-coated titanium implants (n = 10) were randomly selected, and each plate was weighed before and after the coating procedure. Then, the mean weight of the coating was calculated using SPSS17.0 after excluding the maximum and the minimum values. According to the formation of the polymer solutions, the amount of gentamicin of the coating was accurately determined.
The morphology of the gentamicin-coated titanium implants was observed using a Hitachi S4800 scanning electron microscope (SEM) (Hitachi, Tokyo, Japan). For SEM measurements, the gentamicin-coated titanium implants were sputtered with a gold layer in a sputter chamber.
In vitro release behavior of gentamicin
An elution study was performed to investigate the in vitro release behavior of the gentamicin from the gentamicin-coated titanium implants. The implants were immersed in 10 ml of phosphate buffer at pH 7.4 and stored in a water bath at 37°C. Specimens of 100 μl were withdrawn at the following intervals: 1, 6, 12, and 24 h, 2, 4, 6, 8, 10, 12, and 14 days, followed by the fresh dissolution medium replacement. The samples were assayed using a fluorescence polarization immunoassay device (TDxFLx, Abbott Laboratories, Abbott Park, IL, USA), and the studies were performed in triplicate.
The antibacterial efficacy of and bacterial adhesion to the gentamicin-coated titanium implants in vitro
We chose the Staphylococcus aureus as the experimental bacterial strain because Staphylococci are the most common microorganisms that cause implant-related infections [12, 13].
The Staphylococcus aureus strain (ATCC 29213) was supplied by the Department of Laboratory Medicine, Nanjing First hospital, Nanjing Medical University. These bacteria were inoculated on blood agar plates and incubated for 24 h in the incubator at 37°C. Next, a colony forming unit was inoculated in nutritional broth and cultured for 6 h at 37°C to obtain log-phase growth. This culture was then adjusted using the Vitek colorimeter (BioMerleux Inc., Durham, NC, USA) to provide a final density of 1.5 × 108 CFU/ml.
We used 0.5 ml of this bacterial suspension to inoculate a Mueller–Hinton (MH) plate uniformly. Specimens were placed individually on each plate and consisted of three bare titanium implants, three polymer-coated titanium implants and three gentamicin-coated titanium implants. After incubating the bacteria at 37°C for 24 h, measurements were taken to determine the diameter of the inhibition zone. Then, the titanium implants were removed, placed on the other fresh MH plates that had been inoculated with equal concentrations of the bacteria and incubated for 24 h at 37°C; the diameter of the inhibition zone was then measured again. These above-mentioned procedures were repeated until the inhibition zone was eliminated.
A bacterial adhesion study was performed on bare titanium implants and gentamicin-coated titanium implants to determine whether this antibiotic coating can prevent bacteria from adhering and growing on the surface of the implant. The bare titanium implants and gentamicin-coated titanium implants (n = 10) were incubated with 5 ml of the above-mentioned bacterial suspension for 24 h at 37°C. Then, the suspension was removed, and the titanium implants were cleaned twice using sterile PBS to dislodge any bacteria that had not adhered. The implants were then immersed in 2 ml of 0.9% NaCl solution, followed by ultrasonication using an ultrasound cleaner operating at 40 kHz for 5 min. Specimens of 200 μl were extracted and inoculated on the blood agar plates using the spread plate method. These plates were incubated for 24 h in the incubator at 37°C, and the CFUs were counted visually for quantitative analysis. We believed this measurement was a direct indicator of the number of viable bacteria counts adhering to the implants.
In vitro cytotoxicity assay
Osteoblastic MC3T3-E1 cells (MC3T3-E1 Subclone 14, Type Culture Collection of the Chinese Academy of Science, Shanghai, China) were cultured in 25 cm2 flasks containing DMEM medium supplemented with 10% fetal bovine serum and 10 U/L penicillin and streptomycin in a 5% CO2 incubator.
Cell viability was measured using the Cell Counting Kit-8 (Dojindo, Kumamoto, Japan). First, we adopted the above-mentioned electrospinning technique to prepare gentamicin-loaded coating and polymer coating samples on circular glass slides with a diameter of 1 cm. All of these specimens were sterilized using 25 K-Gray gamma radiation. MC3T3-E1 osteoblasts cells in the complete growth culture medium were seeded at a density of 5 × 103 cells/well on bare circular glass slides, gentamicin-coated circular glass slides and polymer-coated circular glass slides in 48-well plates containing six replicates. The culture medium was removed 1, 3 and 5 days after cell seeding, and 200 μl of fresh cell culture medium mixed with 20 μl of CCK-8 solution was added to each well; this was followed by incubation for 3 h. Afterwards, 100 μl of solution was transferred to a 96-well plate, and the fluorescence was read at 450 nm with a microplate reader (Bio-Rad Laboratories, USA).
Statistical analyses
Data are expressed as the mean ± the standard deviation (SD). Significant differences were analyzed using the Student’s t test; the results of cell viability data were analyzed using ANOVA, and p < 0.05 was considered to be statistically significant.
Results
The amount of gentamicin and the surface structure study of the coating
The mean weight of gentamicin was 392.2 ± 57.2 μg for each gentamicin-coated titanium implant. A prepared sample is shown in Fig. 1 shows the morphology of the gentamicin-loaded coating that exhibited nanofibers with smooth surfaces and round cross sections. Using Image J, the mode diameter of the nanofibers was 650–750 nm (average of 705 ± 122 nm).
In vitro release behavior of gentamicin
The release behavior of gentamicin revealed an initial burst release during the first 24 h, followed by a slow and continuous release during subsequent weeks (Fig. 2). Approximately 40% (approximately 156.9 μg) of the gentamicin was released into the PBS within the first day, and after the first 24 h, a slow and steady release of gentamicin was observed. At the end of the 2-week test period, 71% (approximately 278.3 μg) of gentamicin had been released from the coating.
The antibacterial efficacy and bacterial adhesion study
The effect of the gentamicin-coated titanium implants in the presence of Staphylococcus aureus was evaluated using zone of inhibition testing. A zone of inhibition was detected in gentamicin-coated titanium implants and compared with polymer-coated titanium implants and bare titanium implants with no inhibition zones. The maximum mean diameter of the inhibition zone was 19.4 ± 0.98 mm on the first day (Fig. 3a). Over the next several days, the diameter of the inhibition zone decreased slowly and disappeared on the ninth day (Fig. 3b–e).
The gentamicin-coated titanium implants significantly reduced the adhesion of the Staphylococcus aureus compared with bare titanium implants (Figs. 4, 5). Quantitative analysis of the bacterial adhesion of Staphylococcus aureus produced a mean value of 22.7 ± 1.9 CFUs for the gentamicin-coated implants and 1,805.0 ± 173.9 CFUs (p < 0.01) for the bare titanium implants. We think this measurement can directly indicate the ability of the gentamicin-coated implants to prevent bacterial adhesion.
In vitro cytotoxicity assay
The quantitative results were obtained using a CCK-8 assay after cell culture for 1, 3, and 5 days. Figure 5 shows that 1 day after cell seeding, there were slightly more cells adhered to the bare circular glass slides than the gentamicin-coated circular glass slides and polymer-coated circular glass slides, but no significant difference between bare circular glass slides and the other coated circular glass slides is observed (p > 0.05). After 3 and 5 days of culture, the number of cells on the gentamicin-coated circular glass slides and polymer-coated circular glass slides increased more dramatically than that on the bare circular glass. From these data obtained after 5 days of culture, it could be deduced that the coating that exhibited nanofibers with smooth surfaces and round cross sections can improve cellular compatibility by promoting cell migration, adhesion and proliferation. These effects occur because of the high-specific surface area and high porosity of the nanofibers, without cytotoxicity.
Discussion
Implants have played an important role in trauma and orthopedic surgery by helping patients to recover their lost mobility and improve their quality of life. In the United States, approximately 2.6 million orthopedic implants are applied annually [5]. Nevertheless, one major challenge has attracted the attention of clinicians: implant-related infection. Implant-related infection is a disastrous complication that can lead to implant failure, which can considerably delay recovery, reduce the functional outcome and increase health care costs; infection occurs in 0.8–1.9% of knee arthroplasties and 0.3–1.7% of hip arthroplasties [14, 15], and the frequency of implant-related infection is increasing as the number of orthopedic surgeries increases [16].
Various tests and studies have been performed to reduce the rate of implant-related infection. Researchers have developed many versions of metal ion or antibiotic-coated implants as local drug delivery systems to treat infection. Fiedler et al. [17] bound silver ion into the surface of titanium alloy and studied its proliferative response to osteoblasts and antibacterial effects in vitro. They found that the Ag-ion coating can inhibit the colony incidence of Staphylococcus aureus obviously at high dosages without cytotoxicity. Hardes et al. [18] applied the silver-coated prostheses to treat the patients with bone sarcoma. Their results indicated that the use of silver-coated prostheses can reduce the infection rate in the medium term. However, further studies with longer term follow-up periods and larger numbers of patients are necessary to confirm these encouraging results. Gollwitzer et al. [19] prepared a PDLLA coating loaded with gentamicin or teicoplanin on the surface of stainless steel and titanium K-wires, followed by studying the implants’ properties such as antibiotic release and adhesion of viable bacteria. Kälicke et al. [20] coated titanium plates with PLLA loaded with antibiotics and studied the coating’s effect on infection resistance in vitro and in vivo. Schmidmaier et al. [7] reported that intramedullary tibial nails loaded with gentamicin have been applied in eight patients who had open tibial fractures, and no infections were observed during the follow-up.
In this preliminary investigation, we adopted an electrospinning technique to prepare antibiotic coatings on the implants using biodegradable PLGA, PEO and gentamicin. Electrospinning is effective and cost-efficient; more importantly, this technique can result in continuous fibers with diameters ranging from a few nanometers to micrometers. These nanofibers can promote cell adhesion and growth because of their porosity and high-specific surface area [21–23]. The results from the in vitro cytotoxicity assay indicated that the gentamicin-coated circular glass slides promoted cell growth more dramatically than the bare circular glass slides. Therefore, the cell-promoting function of the nanofibers was validated in this study, and there were no indications that the coatings are toxic to the cells.
After implantation, a competitive relationship develops between bacterial adhesion and the adhesion of the host’s own cells to the implants’ surface [20]. Implants offer receptors not only for the host’s cells but also for bacterial cells. This is a very complicated process that is beyond the scope of this manuscript. In brief, time are crucial for the survival of the host’s own cells and the bacterial cells on the surface of the implants. Once the bacterial cells overtake the host and interact with the implants, a biofilm forms in which the bacteria are protected from conventional antimicrobial agents and the host immune system [24, 25] and the resultant infection is inevitable. So the local drug delivery system must provide a high initial release of antibiotic at the location of the implants. Schmidmaier et al. [7] also seem to support this idea. These authors suggested that the technique of delivery must guarantee a rapid release of the antibiotic to prevent the development of bacterial drug resistance. Based on the gentamicin release behavior shown in this study, the gentamicin exhibited an initial burst release from the coating, which was one of the aims of the study. Due to this burst release, a high local concentration of gentamicin can be guaranteed at the moment the equipment is implanted. This will lead to an incompatible environment for the bacteria. We deduced that a high-specific surface area of the coating was one of the major reasons for the initial burst release of gentamicin. Of course, there must be other reasons, such as an immediate detachment of the surface antibiotics from the coating.
The gentamicin does not appear to lose its antibacterial effect after the procedure of the coating preparation and the gamma radiation sterilization of the gentamicin-coated titanium implants. Consistent with our expectations, the coated implants which were loaded with gentamicin did exhibit excellent antibacterial efficacy in vitro and lasted for a week, whereas the control groups showed no signs of bacterial inhibition. In addition, the gentamicin-coated titanium implants significantly reduced the adhesion of the Staphylococcus aureus compared with bare titanium implants. Bacterial adhesion to the implant surface and growth of the above-mentioned biofilm are well-established steps in the pathogenesis of implant-related infection [13, 26, 27]. As a result, prevention of bacterial colonization and adhesion on the surface of the implants is crucial to reduce the rate of infection. In this preliminary investigation, the gentamicin-coated titanium implants showed the potential to prevent the bacterial adhesion.
This preliminary study showed the capacity of the gentamicin-coated titanium implants that were prepared using electrospinning techniques to act as a local drug delivery system. By studying the release kinetics, antibacterial efficacy, bacterial adhesion and cytotoxicity, the advantages are quite obvious. Limitations of the present study include the small sample size and the lack of in vivo experiments. We will address these limitations in our next study.
References
Lohmann R, Haid K, Stockle U, Raschke M (2007) Epidemiology and perspectives in traumatology of the elderly. Unfallchirurg 110:553–560 quiz 561–552
Vester H, Wildemann B, Schmidmaier G, Stockle U, Lucke M (2010) Gentamycin delivered from a PDLLA coating of metallic implants: in vivo and in vitro characterisation for local prophylaxis of implant-related osteomyelitis. Injury 41:1053–1059
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351:1645–1654
Del Pozo JL, Patel R (2009) Clinical practice. Infection associated with prosthetic joints. N Engl J Med 361:787–794
Darouiche RO (2004) Treatment of infections associated with surgical implants. N Engl J Med 350:1422–1429
Zhao L, Chu PK, Zhang Y, Wu Z (2009) Antibacterial coatings on titanium implants. J Biomed Mater Res B Appl Biomater 91:470–480
Schmidmaier G, Lucke M, Wildemann B, Haas NP, Raschke M (2006) Prophylaxis and treatment of implant-related infections by antibiotic-coated implants: a review. Injury 37(Suppl 2):S105–S112
Ji W, Sun Y, Yang F, van den Beucken JJ, Fan M, Chen Z, Jansen JA (2011) Bioactive electrospun scaffolds delivering growth factors and genes for tissue engineering applications. Pharm Res 28:1259–1272
Xu X, Yang L, Wang X, Chen X, Liang Q, Zeng J, Jing X (2005) Ultrafine medicated fibers electrospun from W/O emulsions. J Control Release 108:33–42
Meng W, Kim SY, Yuan J, Kim JC, Kwon OH, Kawazoe N, Chen G, Ito Y, Kang IK (2007) Electrospun PHBV/collagen composite nanofibrous scaffolds for tissue engineering. J Biomater Sci Polym Ed 18:81–94
Choi JS, Leong KW, Yoo HS (2008) In vivo wound healing of diabetic ulcers using electrospun nanofibers immobilized with human epidermal growth factor (EGF). Biomaterials 29:587–596
Trampuz A, Piper KE, Jacobson MJ, Hanssen AD, Unni KK, Osmon DR, Mandrekar JN, Cockerill FR, Steckelberg JM, Greenleaf JF, Patel R (2007) Sonication of removed hip and knee prostheses for diagnosis of infection. N Engl J Med 357:654–663
Zimmerli W, Sendi P (2011) Pathogenesis of implant-associated infection: the role of the host. Semin Immunopathol 33:295–306
Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ (2006) The incidence of deep prosthetic infections in a specialist orthopaedic hospital: a 15-year prospective survey. J Bone Joint Surg Br 88:943–948
Jamsen E, Huhtala H, Puolakka T, Moilanen T (2009) Risk factors for infection after knee arthroplasty. A register-based analysis of 43,149 cases. J Bone Joint Surg Am 91:38–47
Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J (2008) Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty 23:984–991
Fiedler J, Kolitsch A, Kleffner B, Henke D, Stenger S, Brenner RE (2011) Copper and silver ion implantation of aluminium oxide-blasted titanium surfaces: proliferative response of osteoblasts and antibacterial effects. Int J Artif Organs 34(9):882–888
Hardes J, von EC, Streitbuerger A et al (2010) Reduction of periprosthetic infection with silver-coated megaprostheses in patients with bone sarcoma. J Surg Oncol 101(5):389–395
Gollwitzer H, Ibrahim K, Meyer H, Mittelmeier W, Busch R, Stemberger A (2003) Antibacterial poly (d, l-lactic acid) coating of medical implants using a biodegradable drug delivery technology. J Antimicrob Chemother 51:585–591
Kalicke T, Schierholz J, Schlegel U, Frangen TM, Koller M, Printzen G, Seybold D, Klockner S, Muhr G, Arens S (2006) Effect on infection resistance of a local antiseptic and antibiotic coating on osteosynthesis implants: an in vitro and in vivo study. J Orthop Res 24:1622–1640
He W, Horn SW, Hussain MD (2007) Improved bioavailability of orally administered mifepristone from PLGA nanoparticles. Int J Pharm 334:173–178
Zhang YZ, Su B, Venugopal J, Ramakrishna S, Lim CT (2007) Biomimetic and bioactive nanofibrous scaffolds from electrospun composite nanofibers. Int J Nanomed 2:623–638
Bhardwaj N, Kundu SC (2010) Electrospinning: a fascinating fiber fabrication technique. Biotechnol Adv 28:325–347
Engelsman AF, Saldarriaga-Fernandez IC, Nejadnik MR, van Dam GM, Francis KP, Ploeg RJ, Busscher HJ, van der Mei HC (2010) The risk of biomaterial-associated infection after revision surgery due to an experimental primary implant infection. Biofouling 26:761–767
Mombelli A, Decaillet F (2011) The characteristics of biofilms in peri-implant disease. J Clin Periodontol 38(Suppl 11):203–213
Hall-Stoodley L, Costerton JW, Stoodley P (2004) Bacterial biofilms: from the natural environment to infectious diseases. Nat Rev Microbiol 2:95–108
Rodrigues LR (2011) Inhibition of bacterial adhesion on medical devices. Adv Exp Med Biol 715:351–367
Acknowledgments
We gratefully acknowledge the contributions of State Key Laboratory of Bioelectronics, School of Biological Science and Medical Engineering, Southeast University, Nanjing, China and we thank Health Medical Treatment Apparatus Co., Ltd. Suzhou, China for supplying the three-hole titanium implants.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Ll., Wang, Lm., Xu, Y. et al. Preparation of gentamicin-loaded electrospun coating on titanium implants and a study of their properties in vitro. Arch Orthop Trauma Surg 132, 897–903 (2012). https://doi.org/10.1007/s00402-012-1490-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1490-y