Abstract
Background
This study aims to compare radiographic and clinical outcomes of Dynesys and posterior lumbar interbody fusion (PLIF) for the treatment of multisegment disease.
Methods
Thirty-five consecutive patients who received Dynesys implantation at three levels from L1 to S1 from November 2006 to July 2007 were studied. A retrospective analysis of the medical records of 25 patients with the same indications who received 3-level PLIF (L1–S1) was also conducted. Radiographic and clinical outcomes between the groups were compared. All patients included in the analysis completed 3-year follow-up. Dynesys stabilization resulted in higher preservation of motion at the operative levels, as well as total range of motion from L1 to S1. A decrease of anterior disc height was seen in the Dynesys group and an increase was seen in the PLIF group. An increase in posterior disc height was noted in both groups; however, was greater in the PLIF group at 3 years.
Results
The Dynesys group showed a greater improvement in Oswestry Disability Index and visual analogue scale back pain scores at 3 years postoperatively. There were no differences in complications between the two groups.
Conclusion
In conclusion, Dynesys is an acceptable alternative to PLIF for the treatment of multisegment lumbar disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Due to the disadvantages of fusion in the treatment of degenerative conditions of the lumbar spine including pseudoarthrosis, nonunion, instrumentation failure, infection, donor site pain, and adjacent segment disease [1–5], interest has been given to techniques that preserve motion. The Dynesys Spinal Stabilization System (Zimmer, Inc., Minneapolis, MN, USA) uses pedicle screws, polyethylene-terephthalate cords, and polycarbonate urethane spacers to stabilize a functional spinal unit [6]. Contrary to fusion and instrumentation, which results in a rigid connection of the operative level, the system is designed to stabilize the operated segment while allowing some mobility, thus preserving a greater degree of lumbar mobility than with fusion [7]. The Dynesys system is indicated for lumbar spinal stenosis with or without spondylolisthesis and symptomatic disc degeneration and can be used on single or multisegment disease [6, 8].
Clinical studies have mostly indicated positive outcomes with improved Oswestry Disability Index (ODI) scores and visual analogue scale (VAS) pain scores, as well as shorter recovery times than for fusion, for patients with degenerative disc disease (DDD) of the lumbar spine treated with the Dynesys system [9–15]. Despite the positive results reported with Dynesys, there is concern of the effects of stabilization on adjacent segments, and a number of cadaveric, in vivo, and modeling studies have provided conflicting results [7, 16–21]. In addition, there have been few studies on the use of Dynesys for multisegment disease [22, 23].
Thus, the purpose of this prospective study was to compare the radiographic and clinical outcomes of patients who received Dynesys implantation for 3-level disease with those who received posterior lumbar interbody fusion (PLIF) with a minimum follow-up of 3 years.
Methods
This prospective study included 35 consecutive patients, 54–71 years of age, who met the inclusion and exclusion criteria and received Dynesys implantation at 3 levels from L1 to S1 from November 2006 to July 2007. In addition, a retrospective analysis of the medical records of 25 patients with the same indications who received 3-level PLIF (L1–S1) from May 2004 to March 2006 was conducted, and results were compared between the two groups. This study was approved by the Institutional Review Board of our hospital, all patients in the Dynesys group provided written informed consent for the study and surgery, and the requirement of written consent was waived for the retrospective review.
Patients were included if they had three levels of lumbar spinal degeneration from L1–S1 meeting the following characteristics: one level of spinal stenosis with/without grade 1 spondylolisthesis with two levels of DDD (Pfirmann Grade 2–4), two levels of spinal stenosis with/without grade 1 spondylolisthesis with one level of DDD (Pfirmann Grade 2–4), one level of recurrent herniated intervertebral disc (HIVD) with two levels of DDD (Pfirmann Grade 2–4), or two levels of recurrent HIVD with one level of DDD (Pfirmann Grade 2–4). For inclusion patients also had to have a preoperative ODI >40 and failure of 3 months of conservative therapy. Exclusion criteria were <3 levels of disc degenerative disease, >grade 1 spondylolisthesis, disc collapse >50%, degenerative scoliosis >10°, osteoporosis [bone mineral density (BMD) <−2.5], prior fusion surgery, chronic disease which markedly increased the operative risk, and immunosuppression.
Dynesys implantation was performed according to the directions of the manufacture [6]. In brief; a midline approach was used in all cases as all patients required decompression for at least one level. For levels with no obvious decreased disc height preoperatively, the length of spacer implanted was as measured, whereas for levels with obvious decreased disc heights preoperatively, 1–2 mm was added to the measured length to offload loading in posterior elements including disc and facet joints. Decompression was performed using standard laminotomy techniques. Simple decompression was performed for most cases; however, for cases of severe stenosis or far lateral stenosis extensive decompression, sometimes including facetectomy, was performed.
PLIF was performed in a standard manner. When required, extensive decompression and facetectomy were performed for cage insertion. Autologous bone graft using the decompressed bone chips was used within and around the cage, followed by pedicle screw instrumentation and fixation. Postoperatively, patients in the Dynesys group received a soft support brace (lumbar corset) for 3 months and patients in the PLIF group received a hard plastic lumbar brace for 3 months. Patients did not participate in a rehabilitation program, and were instructed that they should avoid bending but otherwise could maintain a normal lifestyle.
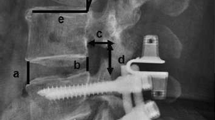
All patients received preoperative and follow-up physical and radiographic examinations at 3 months, and at 1, 2 and 3 years postoperatively. Data collected included flexion, extension, and neutral radiographs, range of motion (ROM) in sagittal view, anterior and posterior disc heights, ODI score, VAS pain score, and preoperative BMD. Radiographs were measured and analyzed by two experienced spine surgeons. Flexion and extension views were taken with the patients in the lateral position. The ROM in the sagittal (flexion–extension) view was obtained by the following formula: ROM sagittal = angle (extension) − angle (flexion). Motion preservation (%) was defined as ROM (postoperatively)/ROM (preoperatively). Disc height was determined on radiographs taken with the patient in the neutral position, and was assessed by measurement of lines drawn at the most prominent points of the endplates anteriorly and posteriorly. Total disc height measured from L1 to S1 was the sum of the disc height of each level. Radiographic instability was defined as (1) flexion versus extension (angulation) >10° or (2) flexion versus extension at the spinal ridge (translation) >3–4 mm. Screw loosening was based on the presence of the double-halo sign on plain radiographs [24]. Only screw loosening as evidenced by a double-halo sign was included in this study. VAS scores were determined on a scale ranging from 0 (no pain) to 10 (worst pain imaginable).
Primary outcome measures were motion preservation and anterior and posterior disc height at the operated level and from L1 to S1. Secondary outcome measures were changes of ODI and VAS back and leg pain scores. ODI and VAS scores were determined preoperatively and at each follow-up visit. Operation time, blood loss, length of hospital stay, and complications were also compared between the two groups. In addition, indications for surgery, the number of levels requiring decompression, and BMD were evaluated with respect to complications.
Statistical analysis
Continuous and categorical variables were compared by independent two-sample t test and Chi-square/Fisher’s exact test, respectively. Paired t tests in both groups were employed to analyze the results of improvement differences from baseline (preoperatively) to 3 years postoperatively. All statistical assessments were two-sided and evaluated at the 0.05 level of significant difference. Statistical analyses were performed using SPSS 15.0 statistics software (SPSS Inc, Chicago, IL, USA).
Results
The Dynesys group included 35 patients (15 males, 20 females) with a mean age of 60.8 ± 4.8 years and the PLIF group included 25 patients (13 males, 12 females) with a mean age of 63.1 ± 4.4 years. Patient demographic and baseline characteristics are shown in Table 1. Implanted levels, ROM at the operated levels, posterior disc height, and ODI and VAS scores were similar between the groups (all, P > 0.05). However, ROM at the L1–S1 level was significantly greater in the PLIF group than in the Dynesys group (47.84 ± 6.97° vs. 42.80 ± 8.43°, respectively, P = 0.017). The anterior disc heights at both the operated level and total height from L1 to S1 in the Dynesys group were significantly greater than those in PLIF group (both, P < 0.001)
Six patients in the Dynesys group were excluded from the radiological and clinical outcomes analyses because they did not complete the 3-year follow-up. All other patients completed the 3-year follow-up. The percentage changes of radiographic and clinical outcomes 3 years postoperatively between the groups are presented in Table 2. Significant decreases of the ROM at both the operated and L1–S1 levels at 3 years postoperatively were observed in both groups (all, P < 0.001). Motion preservation at the operated and L1–S1 levels 3 years postoperatively in the Dynesys group was significantly greater than in the PLIF group. A statistically significant decrease in the percentage change of total anterior disc height at both the operated and L1–S1 levels at 3 years postoperatively was observed in the Dynesys group (P < 0.05). In contrast, a significant increase in the percentage change of total anterior disc height at both the operated and L1–S1 levels at 3 years postoperatively were observed in the PLIF group (P < 0.05). Significant differences in the percentage change of total anterior disc height at the operated level and L1–S1 levels were found between the groups. Moreover, significant increases in the percentage change of total posterior disc height at both the operated and L1–S1 levels were observed in both groups (P < 0.05) and a significant difference in the percentage changes in disc height at the operated and L1–S1 levels between the two groups was found (P < 0.05).
Statistically significant improvements in the ODI and VAS leg and back pain scores were found in both groups at 3 years postoperatively (all, P < 0.05). The degree of improvements in ODI and VAS back pain were significantly greater in the Dynesys group than in the PLIF group. Figure 1 shows that operation time, blood loss, and length of hospital stay were all significantly less in the Dynesys group (P < 0.05).
There was no significant difference in postoperative complications such as screw loosening, malpositioning of screw, adjacent level instability, dislodgement of the interbody device, wound infection, dura tears, pseudarthrosis, and unresolved back pain between the groups (Table 3; all, P > 0.05). However, two patients in the Dynesys had malpositioning of screws during surgery.
Eleven complications occurred in nine patients of the Dynesys group; five screw loosening (14.3%) and six of adjacent level instability (17.1%). There were 12 patients with spondylolisthesis in the Dynesys group, and the chances of screw loosening and adjacent level instability in patients with spondylolisthesis were significantly higher than in patients without spondylolisthesis (80.0 vs. 20.0%, P = 0.038 and 83.3 vs. 16.7%, P = 0.012, respectively). Moreover, complications occurred more often in patients who underwent 2- or 3-level decompression (4/20, 20.0% and 5/7, 71.4%, respectively). In addition, 7 of 25 patients (28%) with a BMD >−1.5 and 2 of 10 patients (20%) with a BMD ≤−1.5 had complications in the Dynesys group. However, the statistically significant association between BMD and complications was not found in the Dynesys group (28 vs. 20%; P = 0.625).
Discussion
With 3-year follow-up, the results of this study indicated that compared to PLIF, Dynesys stabilization resulted in higher preservation of motion at the operative levels as well as total ROM from L1 to S1. Dynesys implantation resulted in a decrease of anterior disc height, PLIF resulted in an increase in anterior disc height, and both systems resulted in an increase in posterior disc height; however, PLIF resulted in a greater height than that of Dynesys at 3 years. Dynesys implantation resulted in greater improvement in ODI and VAS back pain scores at 3 years postoperatively than PLIF.
Few studies have examined the use of Dynesys for the treatment of multisegment disease. Klöckner et al. [23] reported good results in 20 patients who received multiple segment decompression and Dynesys implantation. Kim et al. [22] compared single and multilevel Dynesys implantation (single, 7; multiple level, 14) in patients with degenerative spinal disease and found similar clinical improvements in both groups, though they noted retrolisthesis in cranial adjacent segments in 6 of the 14 patients who received multiple level Dynesys implantation. Our results are comparable with those above, though we did not note significant adjacent segment pathology.
Greater preservation of motion with Dynesys than with PLIF is predicted by the design of the device, and we found that Dynesys is able to provide a controlled ROM at 3 years postoperatively when implanted at three levels. Schaeren et al. [25] reported the results of 19 patients with degenerative spondylolisthesis treated with decompression and Dynesys stabilization with a minimum of 4-year follow-up and found excellent clinical outcomes and that the device provided enough stability to prevent progression of spondylolisthesis, but that degeneration at adjacent motion segments occurred. Lee et al. [14] reported the results of 20 consecutive patients treated with Dynesys, and found that the system allowed preservation of motion of the stabilized segments and clinical improvements of ODI and VAS pain scores.
While we found that PLIF was able to maintain both anterior and posterior disc height to a much greater degree that Dynesys, the loss of disc height at both the operative level and L1–S1 with Dynesys was small, and posterior disc height was maintained at both the operated level and L1–S1, though to a lesser degree, than with PLIF. However, there are conflicting reports on maintenance of disc height with Dynesys. Kim et al. [22] compared the results of single and multiple-level stabilization with Dynesys in patients with degenerative spinal disease and found no decrease of disc height in either group with a mean follow-up of 31 ± 14 months. Kumar et al. [26] studied 32 patients who received Dynesys implantation, and with all patients completing 2-year follow-up found that the anterior intervertebral disc height was reduced by 2 mm from 9.25 to 7.17 (P < 0.001), whereas there was no significant change in posterior disc height. Beastall et al. [7] reported a reduction of anterior disc height without a significant increase in posterior disc height at 9 months after surgery in 24 patients treated with Dynesys.
In our study, five patients who received Dynesys exhibited adjacent level instability during follow-up, but none required reoperation because of excessive instability. Studies of the effect of Dynesys on the mobility and degeneration of adjacent segments are conflicting. Some authors have suggested that preservation of motion at the operative level prevents degeneration at the adjacent segments [12]. Beastall et al. [7] studied 24 patients treated with Dynesys and at 9 months postoperatively found limited movement at the operative level and no significant increase of mobility at the adjacent levels. Schmoelz et al. [16] reported that Dynesys stabilization did not result in an increase in mobility of adjacent segments based on a study of cadavers. Schaeren et al. [25] studied 19 patients with a minimum 4-year follow-up and found no measurable motion at the operative level, while new signs of degeneration were present in adjacent motion segments in 47% of the patient, a rate similar to that reported after lumbar fusion [27]. Kumar et al. [26] studied 32 patients with Dynesys and also noted continued degeneration at the index and adjacent segments, but believed that the changes were possibly a result of the natural progression of the disease. Liu et al. [17] used a displacement-controlled finite element analysis to evaluate the mechanical behavior of the lumbar spine after Dynesys placement and found greater ROM, annulus stress, and facet loading in the adjacent levels.
The improvement in ODI and back pain VAS scores was greater at 3 years postoperatively in the Dynesys group. Significant improvements in ODI and pain scores with Dynesys stabilization are consistent with many reports in the literature [9–15]. We believe that the reason for the greater improvement with Dynesys in treating multisegment disease is because Dynesys is a load-sharing device that results in less stiffness than PLIF.
We found that operation time, blood loss, and length of hospital stay were all significantly less in the Dynesys group. The shorter surgical time is likely because with the Dynesys system there is no need for endplate preparation and insertion of an interbody device or bone grafting. Less blood loss in the Dynesys group is presumably because insertion of the Dynesys device requires less bone and soft tissue dissection as compared to PLIF. Likewise, the shorter hospital stay of patients in the Dynesys group is most likely because insertion of the device is less invasive as compared to PLIF [9, 13, 25].
Complications in the two groups were comparable in this study. However, with Dynesys screw loosening and adjacent level instability were significantly greater in patients with spondylolisthesis than those without, and complications were more common in patients who required 2- or 3-level decompression. Ko et al. [28] studied screw loosening after implantation of the Dynesys system in 71 patients who underwent decompression for 1- or 2-level lumbar spondylosis. They found radiographic evidence of screw loosing in 19.7% of patients (4.6% of screws); however, screw loosening had no adverse impact on clinical improvement. In our study, five cases of screw loosening occurred in each group; however, no revision surgeries were required. It should be noted that, although the difference was not statistically significant, two dural tears occurred in the PLIF group during the procedure of cage insertion, whereas none occurred in the Dynesys group; dural tear with cage insertion is a known complication of PLIF whereas is not likely to occur with implantation of Dynesys.
Though most studies have shown good outcomes with Dynesys, some have reported results no better than those obtained with PLIF. In a study of 37 patients with acquired lumbar stenosis, segmental instability, and DDD who underwent lumbar decompression and Dynesys implantation, Würgler-Hauri et al. [29] reported that patients experienced a reduction of radicular pain, but a worsening of lumbar pain, and that 27% of patients described a poor outcome. In addition, 19% of patients required revision surgery by 1-year. Grob et al. [30] retrospectively studied 31 patients who received Dynesys with at least 2 years of follow-up and during the 2 years following the original surgery, 19% of patients either had or were scheduled for revision surgery, only half of the patients indicated that the operation had improved their overall quality of life, and less than half reported improvements in their functional capacity.
There are some limitations of this study. Though the follow-up period in this study was 3 years, much longer follow-up is required to fully determine segmental instability in adjacent levels and long-term outcomes. Potential errors exist in measuring radiographic images, though this was by having two experienced spine surgeons read the radiographs. Though statistical significance was found in the results, the patient numbers are relatively small, and the data are from a single medical center. Lastly, of note is that many guidelines indicate that surgery should not be considered until after 1 year of nonsurgical treatment; however, in our country 3 months of nonsurgical treatment is standard after which surgery is considered if there is no improvement.
Conclusions
In summary, results of this study indicate that Dynesys is an acceptable alternative to PLIF for the treatment of multisegment lumbar disease. Dynesys results in good motion preservation, and compared to PLIF Dynesys is associated with less blood loss and shorter surgical time and hospital stay. Though the results of this study are based on a follow-up of 3 years, lengthier follow-up is needed to adequately determine long-term outcomes.
References
Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG, Mummaneni P, Watters WC 3rd, Wang J, Walters BC, Hadley MN (2005) American Association of Neurological Surgeons/Congress of Neurological Surgeons. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 5: correlation between radiographic and functional outcome. J Neurosurg Spine 2:658–661
Kumar MN, Baklanov A, Chopin D (2001) Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 10:314–319
Chou WY, Hsu CJ, Chang WN, Wong CY (2002) Adjacent segment degeneration after lumbar spinal posterolateral fusion with instrumentation in elderly patients. Arch Orthop Trauma Surg 122:39–43
Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T (2004) Risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976) 29:1535–1540
Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K (2000) Outcome of one level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine (Phila Pa 1976) 25:1837–1842
Dynesys® Dynamic Stabilization System. Dynesys LIS surgical technique. Zimmer, Inc., Minneapolis
Beastall J, Karadimas E, Siddiqui M, Nicol M, Hughes J, Smith F, Wardlaw D (2007) The Dynesys lumbar spinal stabilization system: a preliminary report on positional magnetic resonance imaging findings. Spine (Phila Pa 1976) 32:685–690
Schwarzenbach O, Berlemann U, Stoll TM, Dubois G (2005) Posterior dynamic stabilization systems: DYNESYS. Orthop Clin North Am 36:363–372
Schnake KJ, Schaeren S, Jeanneret B (2006) Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976) 31:442–449
Bordes-Monmeneu M, Bordes-Garcia V, Rodrigo-Baeza F, Saez D (2005) System of dynamic neutralization in the lumbar spine: experience on 94 cases. Neurocirugia (Astur) 16:499–506 (article in Spanish)
Putzier M, Schneider SV, Funk JF, Tohtz SW, Perka C (2005) The surgical treatment of the lumbar disc prolapse: nucleotomy with additional transpedicular dynamic stabilization versus nucleotomy alone. Spine (Phila Pa 1976) 30:E109–E114
Stoll TM, Dubois G, Schwarzenbach O (2002) The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J 11(Suppl 2):S170–S178
Welch WC, Cheng BC, Awad TE, Davis R, Maxwell JH, Delamarter R, Wingate JK, Sherman J, Macenski MM (2007) Clinical outcomes of the Dynesys dynamic neutralization system: 1-year preliminary results. Neurosurg Focus 22:E8
Lee SE, Park SB, Jahng TA, Chung CK, Kim HJ (2008) Clinical experience of the dynamic stabilization system for the degenerative spine disease. J Korean Neurosurg Soc 43:221–226
Nockels RP (2005) Dynamic stabilization in the surgical management of painful lumbar spinal disorders. Spine (Phila Pa 1976) 30(Suppl 16):S68–S72
Schmoelz W, Huber JF, Nydegger T, Dipl-Ing, Claes L, Wilke HJ (2003) Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech 16:418–423
Liu CL, Zhong ZC, Shih SL, Hung C, Lee YE, Chen CS (2010) Influence of Dynesys system screw profile on adjacent segment and screw. J Spinal Disord Tech 23:410–417
Delank KS, Gercek E, Kuhn S, Hartmann F, Hely H, Röllinghoff M, Rothschild MA, Stützer H, Sobottke R, Eysel P (2010) How does spinal canal decompression and dorsal stabilization affect segmental mobility? A biomechanical study. Arch Orthop Trauma Surg 130:285–292
Vaga S, Brayda-Bruno M, Perona F, Fornari M, Raimondi MT, Petruzzi M, Grava G, Costa F, Caiani EG, Lamartina C (2009) Molecular MR imaging for the evaluation of the effect of dynamic stabilization on lumbar intervertebral discs. Eur Spine J 18(Suppl 1):40–48
Cheng BC, Gordon J, Cheng J, Welch WC (2007) Immediate biomechanical effects of lumbar posterior dynamic stabilization above a circumferential fusion. Spine (Phila Pa 1976) 32:2551–2557
Niosi CA, Zhu QA, Wilson DC, Keynan O, Wilson DR, Oxland TR (2006) Biomechanical characterization of the three-dimensional kinematic behaviour of the Dynesys dynamic stabilization system: an in vitro study. Eur Spine J 15:913–922
Kim CH, Chung CK, Jahng TA (2011) Comparisons of outcomes after single or multilevel dynamic stabilization: effects on adjacent segment. J Spinal Disord Tech 24:60–67
Klöckner C, Beck A (2011) Polysegmental Dynesys system. Orthopade 40:156–161 (article in German)
Dakhil-Jerew F, Jadeja H, Cohen A, Shepperd JA (2009) Inter-observer reliability of detecting Dynesys pedicle screw using plain X-rays: a study on 50 post-operative patients. Eur Spine J 18:1486–1493
Schaeren S, Broger I, Jeanneret B (2008) Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976) 33:E636–E642
Kumar A, Beastall J, Hughes J, Karadimas EJ, Nicol M, Smith F, Wardlaw D (2008) Disc changes in the bridged and adjacent segments after Dynesys dynamic stabilization system after two years. Spine (Phila Pa 1976) 33:2909–2914
Rahm MD, Hall BB (1996) Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord 9:392–400
Ko CC, Tsai HW, Huang WC, Wu JC, Chen YC, Shih YH, Chen HC, Wu CL, Cheng H (2010) Screw loosening in the Dynesys stabilization system: radiographic evidence and effect on outcomes. Neurosurg Focus 28:E10
Würgler-Hauri CC, Kalbarczyk A, Wiesli M, Landolt H, Fandino J (2008) Dynamic neutralization of the lumbar spine after microsurgical decompression in acquired lumbar spinal stenosis and segmental instability. Spine (Phila Pa 1976) 33:E66–E72
Grob D, Benini A, Junge A, Mannion AF (2005) Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine (Phila Pa 1976) 30:324–331
Conflict of interest
All authors confirm that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, SW., Yen, CY., Wu, CH. et al. Radiographic and clinical results of posterior dynamic stabilization for the treatment of multisegment degenerative disc disease with a minimum follow-up of 3 years. Arch Orthop Trauma Surg 132, 583–589 (2012). https://doi.org/10.1007/s00402-012-1460-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1460-4