Abstract
Patients and methods
Forty consecutive patients (21 females and 19 males) in a single centre underwent 50 tibial tubercle advancement osteotomy procedures for patellofemoral arthritis between January 1993 and April 2007. Twenty knees with patellar maltracking also underwent medialisation of the tibial tubercle (6–12 mm) in addition to the standard 10–15 mm elevation. Femoral head bone allograft blocks were utilised in all cases, and all patients achieved bony union without further surgery. Forty-five knees had previously undergone arthroscopy, 18 with arthroscopic lateral releases.
Results
Ninety-four percentage of knees had sustained improvement in visual analogue pain scores (mean improvement of 37.4, P < 0.05) at a mean follow-up of 81 months (range 26–195 months), with 96% of patients still satisfied; and 92% of knees had sustained improvement in Shelbourne and Trumper anterior knee function scores (mean improvement of 39.8, P < 0.05). Overall clinical outcomes were rated excellent/good in 77%, fair in 35% and poor in 8% of knees. Two knees required arthroplasty surgery over the follow-up period (at 18 months and 8 years), and their anterior knee pain and function scores were not included in the analyses. Six knees (12%) suffered major complications: 1 temporary common peroneal neuropraxia; 2 intraoperative tibial metaphyseal fractures; and 3 tibial tuberosity fractures (at 8 days, 3 weeks and 3 months). Four knees (8%) suffered superficial wound infections, 31 knees had some numbness around the midline scar, 7 knees had scar pain lasting up to 12 months, and 22 knees (44%) experienced some discomfort relating to the metalwork, which was removed in all these cases.
Conclusions
Tibial tubercle advancement osteotomy can be an effective treatment for anterior knee pain and for patients with arthroscopic evidence of patellar chondral damage. It can provide excellent/good long-term functional results in the majority of patients, with very high satisfaction levels and sustained improvement in pain symptoms. The use of femoral head bone allograft is both effective in obtaining bony union and by definition avoids the donor-site morbidity. Knees with patellar malalignment may also undergo individualised medialisation of the tibial tubercle such that the patella lies in the centre of the femoral trochlea, and may benefit from lateral trochleaplasty surgery in the presence of trochlear dysplasia. However, the major operative complication rate is high at 12%, and fracture of the tibial tubercle is associated with a poorer outcome. One can expect 10% of operated knees to have had some clinical deterioration in the patellofemoral joint by a mean follow-up of 93 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The optimum treatment for anterior knee pain associated with patellofemoral arthritis remains controversial, and various surgical options have been proposed when there is a failure of conservative management. Amongst these is the displacement osteotomy of the tibial tuberosity, which was first conceived in the nineteenth century in an attempt to alter patellar tracking. Medial displacing single plane tubercle transfers, such as the Elmslie-Trillat procedure, decreased the Q angle. The Maquet osteotomy, first described in 1976 as a treatment for chondromalacia patellae and patellofemoral osteoarthritis, elevated the tibial tubercle 20 mm in a single plane. This advanced the patellar tendon insertion, increasing the lever arm of the extensor mechanism, and reduced the forces acting across the patellofemoral joint [1]; an elevation of 10–15 mm was subsequently shown to be the optimum advancement to reduce the patellofemoral contact stresses [2–4]. Though attaining satisfactory clinical results with improvements in function and pain relief in 65.5–85% of patients [5–8], the Maquet osteotomy was associated with major complications and up to 40% of patients were reported to have problems with delayed wound healing, tibial tubercle and proximal tibial fractures and non-union at the osteotomy sites [9–12]. The Fulkerson osteotomy, a multiplane anteromedialising modification of the Elmslie-Trillat procedure, also elevated the tibial tubercle up to 15 mm, decreasing the lateral facet contact pressures as well as realigning the joint, without the need for bone graft [13–15]. Though obtaining good/excellent short-term clinical results in 60–93% of patients [14, 16] and with improved wound healing compared with the Maquet procedure, non-union, loss of fixation and tibial fractures still occurred [17–22], and this sliding osteotomy suffered from the loss of ability to adjust each of the single planes alone, once made. Adaptations to the Maquet osteotomy that have combined tibial tubercle medialisation and elevation have also been reported to reduce patellofemoral contact pressures and improve patellar tracking; these have been reported to have lower complication rates and up to 84% overall subjective improvement in symptoms [23].
This paper retrospectively reviews the outcomes of 50 consecutive tibial tubercle advancement osteotomies, 20 with additional tibial tubercle medialisation and 5 with additional lateral femoral trochleaplasties, performed on 40 patients by a single surgeon over a fourteen-year period, with a mean follow-up of 81 months (26–195 months).
Patients
Forty consecutive patients (21 females and 19 males), with a mean age of 29 years (range 17–51 years), and a mean body mass index of 27 (range 20–35), underwent 50 (23 right- and 27 left-sided) tibial tubercle advancement osteotomy procedures performed by the senior author between January 1993 and April 2007. The indication for surgery was symptomatic patellofemoral arthritis in all 50 knees, and 14 knees also had a history of recurrent habitual patella dislocation. No patient had any history of patellar fracture. The degree of patellofemoral chondral damage was scored intraoperatively according to the Outerbridge classification. The mean Outerbridge score was 3.44, and all knees had chondral damage to the lateral patellar facet and distal patella. The medial patellar facet was affected to a lesser extent with mean Outerbridge scores of 1.72. There was no significant difference in either the distribution or the degree of chondral damage between those patients with or without patellar maltracking/dislocation (Maltracking knees: lateral facet 11 grade 3, 9 grade 4; medial facet 9 grade 1, 8 grade 2, 3 grade 3; distal patella 15 grade 2, 5 grade 3. Non-maltracking knees: lateral facet 17 grade 3, 13 grade 4; medial facet 11 grade 1, 17 grade 2, 1 grade 3, 1 grade 4; distal patella 11 grade 1, 17 grade 2, 1 grade 3, 1 grade 4). Standard knee radiographs included standing AP, standing lateral at 30° and Merchant views. No patient had significant radiographic degenerative changes.
Twenty knees (including all 14 patients with previous patella dislocation) required concomitant medialisation of the tibial tubercle in addition to the tubercle advancement to restore normal patellar tracking; lateral trochlea elevation osteotomies were also performed in 5 of these 20 knees to help restore patellofemoral stability where there was trochlear dysplasia. The five patients undergoing lateral trochlea elevation had a mean sulcus angle of 152° (SD = 3.3) and a mean congruence angle of 6° (SD = 1.26). Forty-five knees had undergone previous arthroscopy, 18 with arthroscopic lateral releases.
Patient case-notes were reviewed and all patients returned a postal questionnaire evaluating their clinical outcomes at a mean of 81 months (range 26–195 months) following surgery. The study conformed to the ethical standards of the institution, and informed consent for participation in the study was obtained from each patient.
Visual analogue scales were used to assess overall patient satisfaction and knee pain both pre- and post-operatively. A score of 0 indicated the patient being very dissatisfied, 100 indicated very satisfied and 50 indicated neither dissatisfaction nor satisfaction. Patients were asked to specify post-operative complications as well as any further intervention that was subsequently made at any Institution. The Shelbourne and Trumper score was used to assess knee function [24]. Though not formally validated, this scoring system specifically examines anterior knee pain symptoms and is suitable for a postal questionnaire. It was originally designed to assess anterior knee pain symptoms following anterior cruciate ligament reconstruction [24] and is based on five exacerbating functional activities including strenuous work/sports, stair-climbing, prolonged sitting, normal daily activities and kneeling. Each activity is scored out of twenty creating a maximum score of one hundred (indicating minimal or no symptoms). Surgical outcome is rated as poor if no improvement is observed, an improvement of 1–19 points is rated fair, 20–49 points is rated good, and 50+ is rated as excellent.
Statistical analysis of the data was performed using Microsoft Excel software. Parametric data were analysed using a two-tailed paired t test at 5% significance levels. Power analysis revealed that a minimum sample size of 19 patients was required to detect a difference in mean anterior knee pain score of twenty with a standard deviation of twenty-five (alpha = 0.05, beta = 0.2) [25].
Surgical procedure
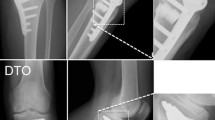
All surgery was performed under general anaesthesia with antibiotic prophylaxis. A thigh tourniquet was inflated with the knee flexed after exsanguination with an Esmarch bandage. A midline incision was made from the superior pole of the patella, extending ten centimetres below the tibial tuberosity. Medial and lateral patellar retinacular releases were performed from the superior pole of the patella to the level of the osteotomy. The infrapatellar fat pad was dissected free from the patellar ligament to allow for adequate mobilisation (Fig. 1a, b).
An osteotomy was made using a microsagittal saw from the medial and lateral sides of the tuberosity and was extended distally for ten centimetres, leaving the distal bony pedicle intact. Two 3.2-mm drill holes were made at the medial and lateral aspects of the distal attachment of the bone shingle to allow elevation without propagating a cortical fracture distally in the tibia. The tuberosity was slowly elevated over a period of 4–5 min using an osteotome to a height of 10–15 mm whilst maintaining an intact periosteal sleeve. A pyramidal block of allograft femoral head was fashioned and wedged beneath the elevated tubercle, maintaining its position.
Flexion of the knee allowed for an assessment of the patellar tracking to be made. If maltracking was identified, the tuberosity was medialised 6–12 mm to restore the position of the patella to the centre of the femoral trochlea. The tuberosity and bone graft were then overdrilled with a 4.5-mm drill and then drilled using a 3.2-mm drill, with countersinking of the cortex. After tapping, a 4.5-mm cortical screw was passed, engaging the posterior tibial cortex (Fig. 2a, b). Screw fixation was not employed in the first six osteotomies in the series, but was subsequently used in all cases. Wounds were closed in layers with a drain placed in the knee joint.
Intravenous antibiotics were continued for 24 h post-operatively, and drains were removed on the morning following surgery. Patients were mobilised fully weight bearing as tolerated and discharged on the first post-operative day. Straight-leg splints were worn for 4 weeks, and gradual mobilisation of the knee commenced after 4 weeks with the aid of a physiotherapist.
Results
Forty-five of 48 operated knees (94%) had improved pain scores, with mean visual analogue scores improving from 79.0 pre-operatively (CI 73.9–84.1) to 41.6 at a latest mean follow-up of 81 (range 26–195) months following surgery (CI 34.6–48.6, P = 0.01); three knees had had no long-term improvement in pain symptoms and one of these had gradually worsened from 3 months post-operatively (Table 1). Shelbourne and Trumper function scores improved from a mean pre-operative score of 36.7 (CI 29.6–43.8) to 76.5 (CI 69.0–84.1, P = 0.01) at 81 months. Forty-four of 48 knees (92%) had a function score improvement and 4 (6%) had had a score deterioration by 81 months (3 of these knees had suffered peri-operative tibial tubercle fractures, and 1 other patient had gradually worsening patellofemoral pain, undergoing knee arthroscopy and synovectomy at 2 and 4 years). The overall clinical outcomes were thus described as excellent in 20 knees (42%), good in 17 knees (35%), fair in 7 knees (15%) and poor in 4 knees (8%).
The two remaining knees had required arthroplasty surgery over the intervening period, and their anterior knee pain and function scores were thus not included in these final analyses. One of these patients, a 39-year-old woman, had had no initial improvement in pain following tubercle transfer surgery and underwent patellofemoral replacement for arthritis 18 months later (she now reports a 30-point improvement following her arthroplasty surgery); a second 40-year-old male patient had total knee replacement surgery after 8 years for progressive knee arthritis, despite having initially had a 48-point improvement in anterior knee pain.
Mean patient satisfaction scores were 79.2 (CI 72.3–86.2). Two cases had satisfaction scores of less than 50; one of these had suffered a tibial tubercle fracture post-operatively which required subsequent operative fixation, and the second had failed to have any symptom improvement following surgery. The two arthroplasty patients registered satisfaction scores of 75 and 78. There were no significant differences in the functional outcomes, pain or satisfaction scores between those patients undergoing tibial tubercle advancement alone and those having combined medialisation and/or trochleaplasty procedures. Similarly, no correlations were found between those patients with worse pre-operative pain or function scores doing either less well or better than those with lesser prior symptoms. Patient body mass index at the time of surgery, their professions/sporting hobbies and the severity of chondromalacia had no significant impact on their clinical outcomes; females had slightly better pain and function scores following surgery, though this only approached significance P = 0.17.
Six cases (12%) encountered major complications; two occurring intraoperatively, three occurring early in the post-operative period and one after 6 months. All these 6 patients had only advancements of the tibial tubercle. One patient developed a post-operative neuropraxia of the common peroneal nerve resolving after 5 weeks and at latest follow-up 55 months post-operatively had a satisfaction score of 74 and a 26-point improvement in anterior knee pain. One knee operated early in the series had an osteotomy without screw fixation, which then fractured 8 days later; this required open reduction and internal fixation using three 3.5-mm screws and subsequently healed. Two knees sustained fractures of the tibial tuberosity following screw fixation; both fractured at the level of the screw, one three weeks post-operatively and the second after 3 months. Neither had disruption of the extensor mechanism and both fractures healed with conservative treatment. Peri-operative tibial tubercle fracture was associated with a poorer functional knee score at latest follow-up. These 3 knees had a mean decrease of 24 points from pre-operative values at a mean follow-up of 94 months (79–108 months). Furthermore, one of these patients also developed a patellar tendonitis that required a subsequent open decompression. Two further patients sustained intraoperative undisplaced proximal metaphyseal tibial fractures at the level of the screw fixation, both of which healed in a straight-leg splint. Thus, 5 knees (10%) suffered peri-operative tibial fractures.
Four knees (8%) suffered superficial wound infections, all of which resolved with oral antibiotics, 31 knees had some numbness around the midline scar, and 7 knees had scar pain lasting up to 12 months. Twenty-two knees (44%) experienced some longer-term pain in relation to the screw, and all had subsequent screw removal. One patient developed medial compartment arthritis and underwent a high tibial osteotomy 4 years post-operatively without complication. No cases of delayed or non-union of the tibial tuberosity osteotomies were observed, and there were no post-operative patellar dislocations.
Discussion
Thirty-seven of 48 knees in our series (77%) had good/excellent outcomes at a mean follow-up of 81 months. This is comparable to the 65.5% good/excellent three-year outcomes seen in a series of 29 consecutive tibial tubercle advancement osteotomies for anterior knee pain [5], the 72.5% good/excellent results seen in 80 tibial tubercle relocation procedures for patellar instability or patellofemoral pain and maltracking at a median of 6.2 years follow-up [26], the 86% good/excellent results in a series of 21 knees undergoing Fulkerson osteotomies for chronic patellofemoral malalignment at a mean of 28 months [27] and the 70% satisfactory results seen at a mean of 30 months in a series of 22 patients undergoing Fulkerson osteotomies for patellofemoral pain and malalignment [16]. Forty-five of 48 knees (92%) in our series also had sustained improvement in pain symptoms at 81 months post-operatively, and 48 knees (96%) had overall satisfaction scores of fifty or more. These results also compare favourably with those of a series of patients undergoing combined tubercle advancement and medialisation who had an 84% overall subjective improvement in symptoms after a mean of 7 years [23].
Forty-two of 45 (93%) arthroscoped knees in our series had prior evidence of patellar chondral damage, which might help explain the significant symptom improvement in 92% of our patients following a reduction in the forces acting across the patellofemoral joint [1]. A previous reported series of Maquet procedures also saw high levels of symptom improvement in those patients with higher Outerbridge grades of chondral damage [28], and a second series of 35 knees with patellofemoral osteoarthritis found that 80% had very good/good long-term results [7].
The decision to combine a medialisation procedure with the tibial tubercle advancement was made based on both the patient history of patella instability and the intraoperative assessment of the patellar tracking. Using this methodology, no patient suffered recurrent patella instability and the two patient groups had indistinguishable good symptom and functional improvement. We did not perform routine pre-operative CT analyses or employ intraoperative patellar tracking methods such as femoral nerve stimulation to calculate tubercle transfer distances; these techniques do not appear to be necessary to achieve good clinical outcomes, with reported series achieving 97% [29] and 86% [30] post-operative patellar stability, respectively.
As has been similarly reported [5], the development of major surgical complications was associated with poorer outcomes in our patients. Of the 4 patients with poor outcomes, 3 had suffered peri-operative tibial tubercle fractures leading to an inevitable hindrance in their rehabilitation, and their latest functional knee scores at a mean of 94 months (79–108 months) had worsened by a mean of 24 points.
Though a 10% tibial fracture rate may appear high, two of these 5 knees were noted to have undisplaced metaphyseal fractures on post-operative radiographs and suffered no post-operative sequelae; both patients followed the normal post-operative protocol. The remaining 3 tibial tuberosity fractures, representing 6% of our cases, each occurred during the post-operative period, two very early (at 8 days and 3 weeks) and one at 3 months, in line with published rates of 2.6–5% of cases [18, 29]. Though there have been reports of delayed tibial fracture occurring after anteromedial osteotomies [31], we encountered no such problem in our 20 anteromedialised knees.
Following surgery, two knees in our series (4%) suffered a subsequent deterioration in patellofemoral osteoarthritis. One of these patients required patellofemoral arthroplasty surgery 18 months post-operatively, and the second knee had 2 knee arthroscopic synovectomies at 2 and 4 years. Two (4%) further knees developed progressive osteoarthritis in the medial knee compartment, one of which then underwent total knee replacement and the other a high tibial osteotomy.
Thus, an overall 5 of the 48 knees in this series (10.4%) suffered some form of clinical deterioration (either functional deterioration or worsening pain) in their patellofemoral joint at latest follow-up (which in these patients was at a mean of 93 months (79–108 months)); this is comparable to the 13% seen in a series of 29 Maquet osteotomy patients at 6 years [5] and to the 14% seen in 25 Fulkerson osteotomies at 30 months post-operatively [16], though greater than that of a reported 5-year review of 12 patients with Fulkerson osteotomies, in whom the quality of improvement was sustained [14].
Despite wound breakdown over the elevated tubercles having been frequently reported [9–12, 32], this did not occur in any of our patients despite our use of the standard midline incision, and only four knees (8%) had superficial wound infections all of which settled with oral antibiotics. A recent series of 42 consecutive Maquet osteotomies performed through an anterolateral incision, with the preservation of the local blood supply and lymphatics, also suffered no single wound complication [32]. Additionally, the commonly reported bone graft donor-site pain, which occurs in 21.9% of patients having bone graft harvesting from the iliac crest [33], was avoided through our use of femoral head allograft. No patient suffered a delayed or non-union of their osteotomy site, which is also in line with findings from a comparative study of 64 patients undergoing tibial tubercle elevation which showed no difference in the clinical efficacy between autograft and allograft bone and found that those patients receiving bone allograft had significantly shorter hospital stays [34]. Twenty-two knees (44%) suffered discomfort in relation to the fixation screw and required removal of this metalwork. This is a common finding in patients having tibial tubercle surgery [16].
In conclusion, tibial tubercle advancement osteotomy is an effective treatment for anterior knee pain and for patients with arthroscopic evidence of patellar chondral damage. It can provide excellent/good long-term functional results in the majority of patients, with very high satisfaction levels and sustained improvement in pain symptoms. The use of femoral head bone allograft is both effective in obtaining bony union and by definition avoids the donor-site morbidity. Knees with patellar malalignment may benefit from an individualised medialisation of the tibial tubercle such that the patella lies in the centre of the femoral trochlea, as well as from a lateral trochleaplasty in the presence of trochlear dysplasia. This approach may reduce the chance of recurrent patellar instability, as was seen in this series. However, the major operative complication rate is high at 12%, and fracture of the tibial tubercle is associated with a poorer outcome. One can expect around 10% of operated knees to have had some clinical deterioration in the patellofemoral joint by a mean follow-up of 93 months.
References
Maquet P (1976) Advancement of the tibial tuberosity. Clin Orthop Relat Res 115:225–230
Ferguson AB, Brown TD, Fu FH, Rutkowski R (1979) Relief of patellofemoral contact stress by anterior displacement of the tibial tubercle. J Bone Joint Surg Am 61(2):159–166
Nakamura N, Ellis M, Seedhom BB (1985) Advancement of the tibial tuberosity: a biomechanical study. J Bone Joint Surg Br 67(2):255–260
Wang CJ (2001) Management of patellofemoral arthrosis in middle-aged patients. Chang Gung Med J 24(11):672–680
Heatley FW, Allen PR, Patrick JH (1986) Tibial tubercle advancement for anterior knee pain. Clin Orthop Relat Res 208:215–224
Mendes DG, Soudry M, Iusim M (1987) Clinical assessment of Maquet tibial tuberosity advancement. Clin Orthop Relat Res 222:228–238
Schmid F (1993) The Maquet procedure in the treatment of patellofemoral osteoarthrosis: long-term results. Clin Orthop Relat Res 294:254–258
Ferguson AB Jr (1982) Elevation of the insertion of the patellar ligament for patellofemoral pain. J Bone Joint Surg Am 64(5):766–771
Bessette GC, Hunter RE (1988) The Maquet procedure. A retrospective review. Clin Orthop Relat Res 232:159–167
Radin EL, Pan HQ (1993) Long-term follow-up study on the Maquet procedure with special reference to the causes of failure. Clin Orthop Relat Res 290:253–258
Radin EL (1986) The Maquet procedure—anterior displacement of the tibial tubercle: indications, contraindications and precautions. Clin Orthop Relat Res 213:241–248
Hadjipavlou A, Helmy H, Dubravcik P, Heller L, Kerner M (1982) Maquet osteotomy for chondromalacia patellae: avoiding the pitfalls. Can J Surg 25(3):342–345
Fulkerson JP (1983) Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res 177:176–181
Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA (1990) Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med 18(5):490–496
Fulkerson JP (1991) Operative management of patellofemoral pain. Ann Chir Gynaecol 80(2):224–229
Morshuis WJ, Pavlov PW, de Rooy KP (1990) Anteromedialization of the tibial tuberosity in the treatment of patellofemoral pain and malalignment. Clin Orthop Relat Res 255:242–250
Cosgarea AJ, Freedman JA, McFarland EG (2001) Nonunion of the tibial tubercle shingle following Fulkerson osteotomy. Am J Knee Surg 14(1):51–54
Stetson WB, Friedman MJ, Fulkerson JP, Cheng M, Buuck D (1997) Fracture of the proximal tibia with immediate weightbearing after a Fulkerson osteotomy. Am J Sports Med 25(4):570–574
Godde S, Rupp S, Dienst M, Seil R, Kohn D (2001) Fracture of the proximal tibia six months after Fulkerson osteotomy. A report of two cases. J Bone Joint Surg Br 83(6):832–833
Bellemans J, Cauwenberghs F, Brys P, Victor J, Fabry G (1998) Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer. A report of four cases. Am J Sports Med 26(2):300–302
Fulkerson JP (1999) Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer. A report of four case. Am J Sports Med 27(2):265
van Haeff MJ, Sauter AJ (1991) Tibial fracture after transposition of the tibial tubercle. Acta Orthop Belg 57(3):317–319
Naranja RJ, Reilly PJ, Kuhlman JR, Haut E, Torg JS (1996) Long-term evaluation of the Elmslie-Trillat-Maquet procedure for patellofemoral dysfunction. Am J Sports Med 24(6):779–784
Shelbourne KD, Trumper RV (1997) Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med 25(1):41–47
DSS Research Inc., Fort Worth, Texas. http://www.dssresearch.com/toolkit/sscalc/size_a2.asp. Accessed 23 May 2009
Pritsch T, Haim A, Arbel R, Snir N, Shasha N, Dekel S (2007) Tailored tibial tubercle transfer for patellofemoral malalignment: analysis of clinical outcomes. Knee Surg Sports Traumatol Arthrosc 15(8):994–1002
Karamehmetoğlu M, Oztürkmen Y, Azboy I, Caniklioğlu M (2007) Fulkerson osteotomy for the treatment of chronic patellofemoral malalignment. Acta Orthop Traumatol Turc 41(1):21–30
Jenny JY, Sader Z, Henry A, Jenny G, Jaeger JH (1996) Elevation of the tibial tubercle for patellofemoral pain syndrome. An 8- to 15-year follow-up. Knee Surg Sports Traumatol Arthrosc 4(2):92–96
Koëter S, Diks MJ, Anderson PG, Wymenga AB (2007) A modified tibial tubercle osteotomy for patellar maltracking: results at two years. J Bone Joint Surg Br 89(2):180–185
Ebinger TP, Boezaart A, Albright JP (2007) Modifications of the Fulkerson osteotomy: a pilot study assessment of a novel technique of dynamic intraoperative determination of the adequacy of tubercle transfer. Iowa Orthop J 27:61–64
Eager MR, Bader DA, Kelly JD IV, Moyer RA (2004) Delayed fracture of the tibia following anteromedialization osteotomy of the tibial tubercle: a report of 5 cases. Am J Sports Med 32(4):1041–1048
Kadambande SS, Auyeung J, Ghandour A, Mintowt-Czyz W (2004) A review of wound healing following Maquet osteotomy. Knee 11(6):463–467
Hill NM, Horne JG, Devane PA (1999) Donor site morbidity in the iliac crest bone graft. Aust NZ J Surg 69(10):726–728
Cornu OH, de Halleux J, Banse X, Delloye C (1995) Tibial tubercle elevation with bone grafts. A comparative study of autograft and allograft. Arch Orthop Trauma Surg 114(6):324–329
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Atkinson, H.D., Bailey, C.A., Anand, S. et al. Tibial tubercle advancement osteotomy with bone allograft for patellofemoral arthritis: a retrospective cohort study of 50 knees. Arch Orthop Trauma Surg 132, 437–445 (2012). https://doi.org/10.1007/s00402-011-1433-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1433-z