Abstract
Objective
This study evaluates a proximally angulated cortical screw forming a triangular construct in lateral locking plates of comminuted intraarticular tibial plateau fractures.
Methods
Sixteen composite tibiae were used for the fracture model and a complete articular fracture of the proximal tibia (AO 41.C2) was performed. A compression force was applied to the medial tibial plateau with an alternating, stepwise loading: 250 N–10 N–300 N–10 N–350 N–10 N–400 N. The relative motion between the different fragments of each sample was measured using a contactless, 3-dimensional digital image correlation system.
Results
Between the medial and lateral condyle, elastic as well as plastic shear was significantly lower using the triangular support screw (p < 0.05). In the metaphyseal region, elastic deformation remained identical, independent of the screw positioning. However, plastic deformation (varus collapse) was significantly reduced by 30–40% using a triangular support screw at higher compression forces (>300 N; p < 0.05).
Conclusion
Based on the results of this study, the use of a triangular support screw in metaphyseal comminuted tibial plateau fractures might enhance fracture stability. However, further studies are necessary to prove these biomechanical results in composite bone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraarticular fractures of the proximal tibia with metaphyseal comminution present a surgical challenge due to their highly unstable fracture pattern and the often-associated soft tissue damage [1]. There is still considerable controversy regarding the optimal fixation method [2–4]. Important cornerstones in treating these difficult fractures are anatomical restoration of the articular surface, correct mechanical alignment [5], and minimal surgical soft tissue injury. While double plating of theses fractures seems to restore good mechanical stability, the necessary extensive soft tissue dissection and the impaired blood supply to the bone remain a concern [5, 6], and the infection rate after double plating seems unacceptably high [6]. Hence, new angular stable implants have been developed to allow less invasive operating techniques and improve mechanical stability. While some biomechanical studies found equal strength and stiffness of lateral locking plates compared to conventional double-plate constructs [7, 8], others showed increased subsidence of the medial fragment with a single lateral locking plate [9, 10]. Higgins et al. [10] even raised concerns about the widespread use of isolated lateral locked plate constructs in bicondylar tibial plateau fractures. In addition, clinical data suggest that unilateral locking plates of bicondylar tibial plateau fractures may lead to loss of reduction [11]. Hence, the question arises as to whether it is possible to further improve the stability of a lateral locking plate with a triangular support screw.
The aim of this study was to evaluate the biomechanical advantages of a lateral locking plate in an AO C2 type tibial fracture fixed with a proximally angulated cortical screw forming a triangular construct. This form of fixation was compared to a horizontal screw.
Materials and methods
Sixteen fourth-generation composite tibiae (Sawbones® Europe, Malmö, Sweden) were used for the fracture model. Standardized osteotomies representing a complete articular fracture of the proximal tibia (AO 41.C2) were performed.
Osteotomies and screw placement
An osteotomy 4 cm lateral to the medial plateau was performed with a surgical saw. The tibiae were then osteotomized 6.5 cm distal to the tibial plateau and a gap of 1 cm in the diaphysis was created. All osteotomies were accomplished with the bone models clamped to a workbench using a custom-built jig to allow repeatable cuts. An eight-hole NCB® locking plate (Zimmer Inc., Winterthur, Switzerland) was placed on the lateral aspect of the tibiae using self-tapping cortical and cancellous screws. The proximal tibial NCB® plate is an anatomically precontoured plate with the possibility of polyaxial locking screw fixation. The cancellous screws are available partially or fully threaded and can reduce a fracture gap achieving interfragmentary and plate-to-bone compression. In a final step, the screw heads are locked to the plate with a locking cap.
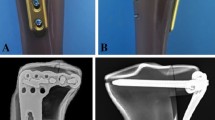
First, under direct visualization, the fracture was anatomically reduced and temporarily secured by applying reduction forceps. Subsequently, the medial and lateral tibial condyles were fixed with three partially threaded cancellous screws to the NCB® plate. These three screws were placed close to the subchondral bone and interfragmentary compression of the articular fragments was obtained (Fig. 1). Two plate holes were then omitted. The third hole was filled with a cortical locking screw in either a horizontal position or angulated support position. In group 1 (n = 8) a horizontal locking screw was placed. In group 2 (n = 8) a 15° proximally angulated locking screw was placed to create a triangular support (Fig. 1).
The two screw holes distally adjacent to the gap and the most distal screw hole were filled with cortical locking screws. All of the fractures showed an anatomical reduction of the articular fragments. Subsequently, locking caps were applied and tightened using a torque-limiting screwdriver (6 N m) as suggested in the manual. A single orthopaedic surgeon with experience in trauma performed all osteotomies and plate fixations.
Sample preparation and mounting
The distal end of the tibia was osteotomized and mounted in a custom-built stainless steel pot. The pot itself was connected to the actuator through a ball joint to avoid torque at the distal end during axial compression. The construct was placed vertically in the anteroposterior view and tilted 5° dorsally as described by Gosling et al. [7]. Proximally, a metal sphere was used to apply the axial compression force. A circular notch (2 mm depth, 7 mm diameter) was drilled into the medial plateau to act as a counterpart to the sphere and prevent slipping of the specimen.
Loading regime
A uniaxial electromechanical material testing machine (Zwick Inc., Ulm, Germany) applied axial compression. The compression force was applied to the medial-tibial plateau (Fig. 1b). The load was reduced to the preload after each load step. The load was held constant at each load step for 2 s to make sure that the peak relative movement between the fragments was detected by the image correlation system. The maximum load that the model securely resisted was 400 N without the metal sphere slipping from the tibial plateau. Stepwise loading (loading rate of 10 N/s) was performed starting at a load of 250 N and a preload of 10 N. The load was then increased stepwise by 50 N up to 400 N. To measure the motion between the different fragments of each sample (Fig. 2), a contactless, 3-dimensional digital image correlation system (LIMESS Messtechnik und Software GmbH, Pforzheim, Germany) was used. The image data were recorded time-synchronized with the force data from the material testing machine with a sampling rate of 5 Hz. This measurement system allows visualizing full-field surface deformations and fracture gap movements. The image data were recorded time-synchronized with the force and distance data from the material testing machine. To calculate the deformations, VIC-3D (Correlated Solutions, Inc., Columbia, SC, USA) software was used. The mean accuracy of the image correlation measurements in this set-up (field of view ~8.5 cm × 12 cm) was within ±1 μm. The two digital video cameras (1.6 megapixels each) tracked the dynamic movements of the sample surfaces with five frames per second (Fig. 1b).
Data were processed and analyzed using MathCAD 13.0 (Mathsoft Inc., Cambridge, MA, USA) and SPSS 15.0 (SPSS Inc., Chicago, IL, USA). Univariate descriptive statistics as well as non-paired t tests were calculated to compare mean elastic and plastic displacements between the two screw placement groups. The p values below 0.05 were considered statistically significant.
Results
Overall, there was no failure in medial fragment fixation or of the NCB® plate. In addition, there was no failure of sample fixation to the material testing machine during testing. The following parameters were measured and obtained.
Elastic shear between the medial and lateral condyle
There was a statistically significant difference between the two groups with regard to elastic shear displacement of the medial condyle in relation to the lateral condyle (Fig. 2c). Group 1 (horizontal screw) samples showed significantly larger displacements (p < 0.001) at all loading steps compared to group 2 samples (angulated screw). Shear motion with an angulated screw showed a reduction of ~80% compared to the shear with a horizontal screw for all loads. See Table 1 and Fig. 3.
Diagrams with mean elastic and plastic deformation as well as shear between the medial and lateral tibial condyles (mean ± standard deviation). For the corresponding image, see Fig. 2. R 2 coefficient of determination, m slope of linear trend line
Obviously, the absolute elastic and plastic shear between the medial and lateral fragment was marginal and probably without clinical relevance. However, with increasing load, only the motion in the group with the horizontal screw increased linearly. Hence the difference is more obvious with increasing load and may be of clinical relevance with higher loads (i.e., full weight bearing).
Plastic shear between the medial and lateral condyle
A statistically significant difference (p < 0.05) in the two groups was found in plastic shear deformation as well at all loading steps. Group 1 (horizontal screw) samples showed larger plastic shear deformation than the ones in group 2 (angulated screw, Fig. 2c). Angulated screws reduced plastic shear by ~115% compared to horizontal screw placement. See Table 1 and Fig. 3.
Elastic deformation at the metaphyseal osteotomy gap
Elastic deformation at the metaphyseal osteotomy gap was defined as the difference in length between the proximal joint fractions and the distal diaphysis below the osteotomy gap (Fig. 2a, b). At all loading steps, the samples with the proximally angulated screw showed 5.1–6.4% smaller elastic deformation at the lateral and the medial tibial condyle in relation to the tibial diaphysis (Table 2). However, these differences were not significant (Table 2; Fig. 3). Hence, both constructs showed no significant difference in stiffness.
Plastic deformation at the metaphyseal osteotomy gap
Plastic deformation at the metaphyseal osteotomy gap was defined as the residual difference in length between the proximal joint fractions and the distal diaphysis below the osteotomy gap after each loading step (Fig. 2a, b).
The plastic deformation across the metaphyseal gap was significantly reduced in the group with the angulated screw compared to the horizontal screw at compression loads higher than 300 N (Table 2). The differences increased with increasing axial loads. The most significant difference in plastic deformation was found at the highest axial load of 400 N [medial condyle (means): 519 μm for horizontal screw, and 336 μm for the angulated screw, difference 35.3%, p = 0.004; lateral condyle: 261 and 159 μm, respectively, difference 38.9%, p = 0.009]. See Table 2 and Fig. 3.
Discussion
High-energy bicondylar proximal tibial fractures with metaphyseal extension typically present with an associated severe soft tissue injury. Extensile approaches and double plating restore sufficient mechanical stability. However, extensive dissection can compromise the vulnerable tissue envelope around the joint as well as the periosteal blood supply with increased postoperative complications such as infection and non-union [11, 12]. Lateral locking plates are an established treatment option in operative management of proximal tibial plateau fractures [2]. The locking plates retain reduction better than conventional plates and the operative approach can be performed less invasively with percutaneous placement of the screws [11, 13]. However, Gosling et al. [11] reported a 14% loss of reduction in bicondylar tibial fractures despite unilateral locking fixation. Improving stability of lateral locking plates remains an important issue. There are no biomechanical studies investigating the effects of a triangular support screw to the best of our knowledge. A polyaxial locking plate was used which allowed different screw positions. The plastic deformation after loading represents the subsidence of the medial tibial plateau (Fig. 2c) or the varus collapse (Fig. 2a, b) at the metaphysis. Hence, plastic deformation should be as small as possible. A triangular support screw reduced the subsidence by more than 100% and the varus collapse by 30–40% at 400 N. Furthermore, the effect of this support screw became more evident as the load was increased. The current data strongly support the use of a triangular support screw in all proximal tibial fractures with metaphyseal comminution. It is noteworthy that the elastic deformation of the construct was no different between the two configurations. Hence, a triangular screw construct did not influence the stiffness or the fracture motion and should not influence fracture healing.
Most other studies compared locking plates versus conventional plates or double versus unilateral plating. Mueller et al. [14] investigated three different methods of plate fixation in 24 cadaveric bicondylar tibial fractures with meta-diaphyseal dissociation. They compared a lateral periarticular plate with a posteromedial small fragment dynamic compression plate, a lateral periarticular plate with a posteromedial 1/3-tubular plate and a lateral fixed-angle plate (LISS®, Synthes Inc.). Construct stiffness and maximum load to failure was measured with respect to medial condylar displacement. No significant difference between the three constructs was found. In addition, Gosling et al. [7] investigated the biomechanical stability of 41.C1 fractures in human cadaver tibiae managed with open reduction and internal fixation using a lateral locking plate (LISS®) in comparison with a five-hole L-buttress plate laterally and a four-hole 1/3-tubular plate in antiglide technique medially. There was no significant difference in vertical subsidence between the two constructs. Others, however, found superior results for the double-plating technique [9, 10, 15]. Higgins et al. [10] compared a dual-plate construct (4.5 mm non-locking proximal tibial plate with a 5-hole 1/3-tubular plate) to an isolated lateral locking plate (4.5 mm fixed-angle proximal tibial plate, Synthes Inc.) for a C1-type fracture. Subsidence of the medial and lateral tibia plateaus was measured as well as maximum load to failure. The dual-plate fixation showed less vertical subsidence of the medial fragment than the lateral locking plate. In addition, Egol et al. [9] found significantly less subsidence of the medial fragment with a dual-plate construct in C1 fractures. Ratcliff et al. [15] compared fixation of an isolated medial tibial plateau fracture with a lateral proximal tibial locking plate (Synthes Inc.) to a medial buttress plate in six matched pairs of fresh cadaveric tibiae. The medial buttress plate provided significantly greater stability in static loading.
However, these studies exhibit some considerable shortcomings. In the studies by Higgins et al. and Ratcliff et al. [10, 15] no lag screws for the articular fragments were used in the locking plate construct. Egol et al. [9] used two independent 3.5 mm cortical screws above the locking plate. It is not reported whether these two screws were lag screws or not. However, the X-ray of their construct shows that the fracture gap of the medial fragment was not closed, questioning whether sufficient interfragmentary compression of the articular fragments was obtained. In the present study, a polyaxial locking plate was used. The plate allows polyaxial screw placement and interfragmentary compression through the plate. The screws are locked at the end with a locking cap. Stoffel et al. [16] found improved construct stability in distal intraarticular femur fractures when plate-to-bone compression and locking were combined. It seems reasonable that interfragmentary compression of the medial and lateral articular fragment and plate-to-bone compression might also improve stability in proximal tibial fractures. This could explain the small amount of plastic deformation seen in the present study. Furthermore, the polyaxial plate allows subchondral screw positioning where generally good bone stock is available [17]. As demonstrated in human cadaveric MR and micro-CT studies, the bone is densest in the subchondral area [18] and therefore it is important to place the proximal screws near the subchondral region of the tibial plateau to gain the best support.
No comparison with the mechanical properties of dual-plating constructs or non-locking plates was done. Whether the combination of subchondral screw position, polyaxiality, and interfragmentary compression in combination with the triangular construct produces sufficient stability in proximal tibial fractures with metaphyseal comminution must be shown by future biomechanical studies using fresh frozen specimens.
A further limitation of this study is the use of a composite bone model instead of fresh frozen human cadavers. Composite bones reflect more the mechanical characteristics of young patients and the results might differ in osteoporotic bone. However, complex intraarticular tibial plateau fractures generally are high-energy traumas occurring more frequently in young patients.
Conclusion
In this study, a triangular support screw through a lateral locking plate supporting the medial tibial plateau allowed significantly less subsidence under axial loading compared to a construct with a horizontal screw. The difference was apparent not only in the intraarticular extension of the osteotomy, but also in the metaphyseal osteotomy gap. Relative shear between the lateral and the medial tibial condyles was significantly reduced and there was a decrease in plastic deformation for the intraarticular as well as the metaphyseal fragments. We recommend the use of a triangular construct in proximal bicondylar tibial fractures whenever possible.
References
Barei DP, Nork SE, Mills WJ et al (2004) Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma 18(10):649–657
Cole PA, Zlowodzki M, Kregor PJ (2004) Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma 18(8):528–535
Horwitz DS, Bachus KN, Craig MA et al (1999) A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma 13(8):545–549
Koval KJ, Polatsch D, Kummer FJ et al (1996) Split fractures of the lateral tibial plateau: evaluation of three fixation methods. J Orthop Trauma 10(5):304–308
Moore TM, Patzakis MJ, Harvey JP (1987) Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma 1(2):97–119
Young MJ, Barrack RL (1994) Complications of internal fixation of tibial plateau fractures. Orthop Rev 23(2):149–154
Gosling T, Schandelmaier P, Marti A et al (2004) Less invasive stabilization of complex tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma 18(8):546–551
Karunakar MA, Egol KA, Peindl R et al (2002) Split depression tibial plateau fractures: a biomechanical study. J Orthop Trauma 16(3):172–177
Egol KA, Su E, Tejwani NC et al (2004) Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma 57(2):340–346
Higgins TF, Klatt J, Bachus KN (2007) Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma 21(5):301–306
Gosling T, Schandelmaier P, Muller M et al (2005) Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res 439:207–214
Barei DP, Nork SE, Mills WJ et al (2006) Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am 88(8):1713–1721
Haidukewych G, Sems SA, Huebner D et al (2007) Results of polyaxial locked-plate fixation of periarticular fractures of the knee. J Bone Joint Surg Am 89(3):614–620
Mueller KL, Karunakar MA, Frankenburg EP et al (2003) Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop Relat Res 412:189–195
Ratcliff JR, Werner FW, Green JK et al (2007) Medial buttress versus lateral locked plating in a cadaver medial tibial plateau fracture model. J Orthop Trauma 21(7):444–448
Stoffel K, Lorenz KU, Kuster MS (2007) Biomechanical considerations in plate osteosynthesis: the effect of plate-to-bone compression with and without angular screw stability. J Orthop Trauma 21(6):362–368
Berend ME, Small SR, Ritter MA et al (2010) The effects of bone resection depth and malalignment on strain in the proximal tibia after total knee arthroplasty. J Arthroplasty 25(2):314–318
Hulet C, Sabatier JP, Souquet D et al (2002) Distribution of bone mineral density at the proximal tibia in knee osteoarthritis. Calcif Tissue Int 71(4):315–322
Acknowledgments
No other financial support was received by the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implants used in this study were donated by Zimmer, Inc., Switzerland.
Rights and permissions
About this article
Cite this article
Baumann, P., Ebneter, L., Giesinger, K. et al. A triangular support screw improves stability for lateral locking plates in proximal tibial fractures with metaphyseal comminution: a biomechanical analysis. Arch Orthop Trauma Surg 131, 815–821 (2011). https://doi.org/10.1007/s00402-010-1243-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-010-1243-8