Abstract
The Neer type II distal clavicle fracture is notorious for its high nonunion rate, and surgical treatment is usually recommended. We reviewed articles from January 1990 to September 2009, and among them, 425 cases from 21 studies were included. According to the 425 cases in the literature, sixty patients were treated nonsurgically and 365 surgically. From 365 patients who were treated surgically, 105 were identified as receiving the coracoclavicular stabilization, 162 hook plate, 42 intramedullary fixation, 16 interfragmentary fixation, and 40 K-wire plus tension band wiring. The nonsurgical treatment resulted in 20 (33.3%) nonunions and 4 (6.7%) other complications. The surgical treatment resulted in 6 (1.6%) nonunions, 81 (22.2%) complications other than nonunion. The nonunion rate was significantly high with nonsurgical treatment (p < 0.001), and the complication rate was statistically high with surgery (p = 0.002). With surgical treatment, the nonunion rate was not significantly different among the modalities (p = 0.391). The complication rate was significantly higher in cases of the hook plate (40.7%) and the K-wire plus tension band wiring (20.0%) than those of the coracoclavicular stabilization (4.8%), the intramedullary (2.4%) and the interfragmentary fixation (6.3%). For the nonsurgical treatment, the functional outcomes were generally acceptable despite the high nonunion rate. The nonsurgical treatment could be considered as the first line treatment after sufficient counsel with the patient. The nonunion rate is high, however, the functional outcome is acceptable in most of the cases with nonunion. If the surgical treatment is considered, the intramedullary screw fixation, CC stabilization and interfragmentary fixation would be preferred because of their low complication rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
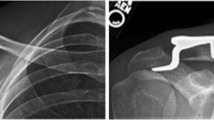
The fractures of the clavicle reportedly represent 2.6% of all fractures with an overall incidence of 64 out of 100,000 per year [1, 2]. Specifically, the distal clavicle fractures account for approximately 10–15% of all clavicle fractures [3, 4]. The distal clavicle fractures typically result from a fall on an outstretched hand or a direct blow to the point of the shoulder [5]. Neer’s classification is widely used to classify such fractures that are mentioned above [6], and these fractures are classified according to their relations to the coracoclavicular ligaments. Fractures that are lateral to the coracoclavicular ligaments are the Neer type I fractures and they make up the majority of lateral clavicle fractures. The Neer type II fractures are characterized by the detachment of the coracoclavicular ligaments from the medial segment [6, 7]. These can be subcategorized into type IIA, in which the fractures occur medial to the coracoclavicular ligaments, and type IIB, in which the fractures occur more laterally with coracoclavicular ligaments disrupted from the proximal section [6]. The Neer type III fractures involve the articular surface of the acromioclavicular joint.
The Neer type I fractures are stable, and they generally require no operation. For the Neer type III fractures, surgical intervention is usually not required in the acute condition. However, these may lead to acromioclavicular arthrosis or osteolysis, requiring late resection of the clavicular end [4]. The Neer type II fractures have received a clinical concern because of the high nonunion rate in nonsurgical treatment that have been observed (>30%) since Neer’s original report. Therefore, operations have been generally required for managing the type II injuries [6, 8–19].
A variety of surgical treatments have been previously reported. As the distal clavicle fracture is relatively rare, many studies about distal clavicle fractures have an insufficient number of cases and lack of control groups. Hence, it is difficult to conclude which treatment modality is most suitable for the type II injury. In addition, there is neither systematic review nor meta-analysis on distal clavicle fractures in the literature. Therefore, the current study was designed to systematically summarize and compare the results of different treatment options [nonoperative method, coracoclavicular (CC) stabilization, hook plate, intramedullary fixation, interfragmentary fixation, and K-wire plus tension band wiring (TBW)] in the management of the distal clavicle fractures, especially for the Neer type II fractures. The purposes of this systematic review were to (1) identify the nonunion and other complication rate according to the treatment methods that had been employed, (2) observe the functional outcomes, and (3) determine which treatment modality is most suitable for the Neer type II distal clavicle fracture.
Materials and methods
Eligibility criteria
The literature review was done on the reports that deal with the distal clavicle fracture. The selected studies presented in this article are found through Cochrane database and Pubmed search. The keywords used for the selection were “distal* AND clavic* AND fracture*” or “lateral* AND clavic* AND fracture*.” The search included the articles that had been published in between January 1990 and September 2009 and written in English. The review of the bibliographies of identified articles was also done to find the omitted studies in the database. Open fractures, obstetric fractures, and mid-shaft and medial clavicle fractures were not included in this study. Among the candidates of 37 studies, we excluded the studies with chronic nonunion cases [5, 20], distal clavicle fracture other than the Neer type II fractures [5, 21], and skeletally immature patients (ages under 18) [12, 20, 22–29]. We also excluded the studies that dealt with performance of two or more different surgical modalities simultaneously among CC stabilization, hook plate, intramedullary fixation, interfragmentary fixation and K-wire plus TBW (e.g. CC stabilization and interfragmentary fixation, or CC stabilization and intramedullary fixation) [12, 28–33]. However, for the studies with an individual data, we extracted the patients’ data that met our inclusion criteria into our study [9, 34–39]. In the end, 21 studies were included in our review.
Available evidence
-
1.
One nonrandomized, retrospective, cohort study that compares nonsurgical treatment and CC stabilization with nonabsorbable braided suture [18] (EBM-level 3 therapy).
-
2.
One nonrandomized, retrospective, cohort study that compares nonsurgical treatment and surgical treatment: CC stabilization and K-wire [9] (EBM-level 3 therapy).
-
3.
One nonrandomized, retrospective, cohort study that compares hook plate, and K-wire plus TBW [40] (EBM-level 3 therapy).
-
4.
Eighteen case series presenting the results of either nonsurgical [19, 37], CC stabilization [34, 35, 41–44], Hook plate [38, 45–48], intramedullary [49, 50], interfragmentary [39, 51] and K-wire plus TBW [36] (EBM-level 4 therapy).
Data abstraction
The following data was extracted from each identified article: the study type, the level of evidence, the type of treatment, the nonunion rates, other complication rates and functional scores. We categorized the surgical treatment into five types based on the fixation mechanism: CC stabilization, hook plate fixation, intramedullary fixation, interfragmentary fixation, and K-wire plus TBW. The CC stabilization includes all the cases of fixation of the CC interval with a CC screw, suturing with a PDS, a Dacron graft, a mersilene tape, an ethibond, or a suture anchor. The Hook plate fixation is a mechanism specifically designed to hold medial clavicle fragment and acromion (e.g. Wolter plate, AO hook plate, and clavicle hook plate). The Intramedullary fixation includes fixation with an extra-articular or a transarticular screw. The interfragmentary fixation includes an open reduction and internal fixation with a plate except a hook plate or an interfragmentary suture with an ethibond, a PDS, a dacron or a wire. Because the fixation mechanism of a hook plate is different from that of an interfragmentary fixation with the other plates, we analyzed the hook plate separately from the interfragmentary fixation with other plates. We also separated the K-wire fixation which concept is classical and unique as a different method.
Data analysis
The nonunions were analyzed separately from other complications. Further treatment of the nonunion was also considered in the study. The complications included infection, fractures, and hardware-related problems. Specific complications in each treatment modality were listed and interpreted. Functional results were compared when functional evaluations were available in each study. All the information gathered in this study was recorded and analyzed by SPSS software package (version 12.0, SPSS Inc., Chicago, IL).
Results
A total number of 425 adult Neer type II distal clavicle fractures were identified. There were 290 men and 135 women, and the age range was from 18 to 84 years at the time of the trauma. Sixty cases (14.1%) were treated nonsurgically. The CC stabilization was performed in 105 cases (24.7%), hook plate fixation in 162 cases (38.1%), intramedullary fixation in 42 cases (9.9%), interfragmentary fixation in 16 cases (3.8%), and K-wire plus TBW in 40 cases (9.4%).
Overall, there were 26 (6.1%) nonunions, 85 (20%) complications other than nonunion (Table 1). In 60 nonsurgical cases, there were 20 (33.3%) nonunions and 4 (6.7%) other complications. In 365 surgical cases, there were 6 (1.6%) nonunions and 81 (22.2%) other complications (Tables 2 and 3). The nonunion rate was significantly higher in the nonsurgical group, and the other complication rate was higher in the surgical group (p < 0.001 and p = 0.002, Tables 2 and 3). The type of the complications were various according to the treatment modalities (Table 4).
In the surgical treatment group, the nonunion rates were not significantly different among the modalities (p = 0.391). However, the complications other than nonunion were significantly higher in the hook plate fixation (40.7%) and the K-wire plus tension band wiring (20.0%) than those of the coracoclavicular stabilization (4.8%), intramedullary (2.4%) and interfragmentary fixation (6.3%, Fig. 1). That is, the hook plate had a significantly higher complication rate than the rest of the four modalities (all p < 0.017), and the K-wire plus TBW had a higher complication rate than the intramedullary fixation (p = 0.013) and the CC stabilization (p < 0.001), but not significantly higher than the interfragmentary fixation (p = 0.421). However, 4 cases which are CC ossification in CC stabilization [35, 41], 35 cases of the acromial hole migration and some migration of hook plate [38, 45] and 17 symptomatic hardware in hook plate fixation were not considered as complications [40], because the authors of the studies did not consider them as complications in their articles. The ossification of CC space did not affect the functional outcome in most of the cases. Therefore it was considered as a sound phenomenon after the CC stabilization (Appendix).
Since not all studies reported the functional outcome scores of the distal clavicle fractures and they used different functional evaluation instruments, it was difficult to analyze and compare the function between the different treatment modalities. Available evidences was one case control study that dealt with nonsurgical group (nonsurgical vs. CC stabilization) reported no significant difference among the University of California at Los Angeles Shoulder Rating Scale (UCLA score), Constant score, and American Shoulder and Elbow Surgeons (ASES) scores despite the high rate of nonunion, and suggested that the nonsurgical treatment of distal clavicle fracture could be an option [18]. They even separately analyzed 7 nonunion patients who had the mean scores of 31.1 in UCLA, 94.8 in Constant, and 89.9 in ASES score, and which were comparable to the scores in the union cases. The high incidence of nonunion does not preclude a clinical outcome comparable to that achieved by the surgical treatment. Other two case series of the nonsurgical treatment also reported the good clinical outcome and claimed that the conservative treatment is a good option [19, 37]. Among four studies dealt with nonsurgical treatment, only one case control study (nonsurgical vs. CC stabilization and K-wire) criticized the nonsurgical treatment because of the high nonunion rate [9]. However, even in this study, further surgical management, that is distal clavicle resection, was done to one case among five nonunions.
Among 20 nonunion cases in the nonsurgical treatment, five had mild-to-moderate pain and only one had secondary surgical procedure (distal clavicle resection). In six nonunion cases in the surgical treatment group, not all but two underwent secondary surgical procedure (revision and distal clavicle resection).
All case series of the surgical treatment advocated that their method yielded a satisfactory outcome in terms of the union rate and functional score. However, one study supported the hook plate fixation over the K-wire plus TBW because of its low complication rate [40].
Discussion
In this systematic review, the authors intended to identify the union and the complication rate according to the treatment methods and to determine which treatment modality is better suited for the Neer type II distal clavicle fracture. However, many studies that dealt with the distal clavicle fracture had some problems. The distal clavicle fracture is a relatively rare injury. Therefore, the sample size was small in most of the reports. The smallest sample only dealt with five cases. The available literature included only three nonrandomized retrospective case control studies [9, 18, 40]. The majority of all identified studies was retrospective case series, had no control group, and did not use any randomization even though a control group was included. The results should therefore be interpreted with caution, as the validity of the observational studies is limited by the lack of a control group (case series), imbalances between the comparison groups because of the lack of randomization (retrospective case control studies), and potentially biased assessment of outcome measures due to the lack of blinding.
Main reason for the exclusion of the studies was that those include skeletally immature patients and different types other than the type II. We tried to include a study when it presented the individual data. However, if it did not, we had to discard the candidate studies. We set the age limit to 18. The lateral physis continues to proliferate until 18 to 19 years of age and thick periosteum around distal clavicle and acromion forms a protective tube around the bony structures in children. Therefore, distal clavicle fracture of skeletally immature patient surely behaves differently. In addition, we also excluded studies that used two or more different fixation mechanisms simultaneously. We intended to figure out the nonunion and complication rate of the treatment modalities by each mechanism of a fixation. However, since the K-wire plus TBW is a traditional way of fixing fractures and its complication rate is known to be high when it is used around the shoulder region [23, 26], we included and analyzed it separately.
In the present systematic review, the nonsurgical treatment of the Neer type II distal clavicle fracture resulted in a high nonunion rate (33.3%), which is similar to that in the Neer’s study [9, 18, 19, 37]. However, despite the high nonunion rate, the nonsurgical group had no significant difference in the functional scores compared to the surgically treated group in most of the studies [18, 19, 37]. Moreover, the complication rate in the nonsurgical group was statistically low compared to the surgical group. As mentioned in the Result section, some studies did not consider some additional findings as complications, that is 4 cases of CC ossification in CC stabilization [35, 41], 35 cases of the acromial hole migration and some migration of hook plate [38, 45] and 17 symptomatic hardware-related problems in hook plate fixation [40]. These ossifications of CC space did not affect the functional outcome and hardware-related problems in hook plate were resolved after removal. Therefore if we consider these cases as a complication, the complication rate would be much higher in surgically treated group, especially hook plate.
Consequently, this systematic review suggests that the distal clavicle fracture could be treated nonsurgically. In that case, there should be sufficient counsel between the clinician and patient about high nonunion rate and cosmetic problem after nonunion, especially in younger population. However, the functional outcome after nonsurgical treatment remains controversial between studies, therefore a well-organized and randomized clinical trial is needed to resolve this issue.
In the surgical treatment, the nonunion rates were not statistically significant among the methods. However, the complication rates were unacceptably higher in the hook plate fixation and the K-wire plus TBW than those in other surgical modalities. The intramedullary fixation with screw, the CC stabilization and the interfragmentary fixation were clinically acceptable in terms of nonunion and complication rate. Moreover, most of the authors who used the hook plate recommended the removal of the plates as soon as the bony union was achieved to prevent acromial osteolysis and impingement [40, 45–48, 52]. Nevertheless, reported functional outcomes were satisfactory, regardless of what kind of evaluation method used, in all surgical modalities including the hook plate and K-wire. All case series concluded that their surgical methods were acceptable and suitable for treating the Neer type II distal clavicle fracture.
There are some limitations to the present study. First, we subjectively categorized the surgical treatment into five types: CC stabilization, hook plate, intramedullary fixation, interfragmentary fixation and K-wire plus TBW. This was based on the theoretical similarity among the fixation mechanism, however, not everyone may agree with such categorization. Second, among the type II fractures of distal clavicle, there was no certainty whether the type II was purely a type IIB or it included the type IIA. This presented a problem, since the type IIA is not totally distinguishable from the mid-clavicular fracture. Moreover, most of the studies did not subclassified the type II (A and B), even though the difference of prognosis between the two subtypes was not verified until now. Lastly, as described in the Result section, not all the studies reported the functional outcomes of their series, and they also utilized different functional evaluation instruments. Until now, there is no universally accepted scoring instrument, thus it was difficult to analyze and compare the functional outcomes between the studies.
Conclusion
We suggest that the distal clavicle fracture should be treated individually after sufficient discussion with the patients. Based on the current results, we could conclude that there is no clear evidence, but nonsurgical treatment could be considered as the first line treatment. The nonunion rate is high as alleged, however, the functional outcome including pain is acceptable in most of the cases with nonunion. If the surgical treatment is considered, intramedullary screw fixation, CC stabilization and interfragmentary fixation would be preferred due to their low complication rate. On the contrary, K-wire plus TBW should not be considered and hook plate also should not be preferred due to their high complication rate.
Future studies should be based on an adequate sample size which allows a meaningful interpretation of the results and there should be a prospective and randomized multicenter study to compare the different treatment methods.
References
Nordqvist A, Petersson C (1994) The incidence of fractures of the clavicle. Clin Orthop Relat Res 300:127–132
Postacchini F, Gumina S, De Santis P, Albo F (2002) Epidemiology of clavicle fractures. J Shoulder Elbow Surg 11(5):452–456
Craig E (1998) Fractures of the clavicle. In: Rockwood CA Jr, (ed) The shoulder. W.B. Saunders, Philadelphia, pp 428–482
Neer C (1984) Fractures in adults. J B Lippincott Company, Philadelphia
Meda PV, Machani B, Sinopidis C, Braithwaite I, Brownson P, Frostick SP (2006) Clavicular hook plate for lateral end fractures: a prospective study. Injury 37(3):277–283
Neer CS II (1968) Fractures of the distal third of the clavicle. Clin Orthop Relat Res 58:43–50
Neer CS II (1963) Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma 3:99–110
Heppenstall RB (1975) Fractures and dislocations of the distal clavicle. Orthop Clin North Am 6(2):477–486
Edwards DJ, Kavanagh TG, Flannery MC (1992) Fractures of the distal clavicle: a case for fixation. Injury 23(1):44–46
Eskola A, Vainionpaa S, Patiala H, Rokkanen P (1987) Outcome of operative treatment in fresh lateral clavicular fracture. Ann Chir Gynaecol 76(3):167–169
Herscovici D Jr, Sanders R, DiPasquale T, Gregory P (1995) Injuries of the shoulder girdle. Clin Orthop Relat Res 318:54–60
Hessmann M, Kirchner R, Baumgaertel F, Gehling H, Gotzen L (1996) Treatment of unstable distal clavicular fractures with and without lesions of the acromioclavicular joint. Injury 27(1):47–52
Neviaser RJ (1987) Injuries to the clavicle and acromioclavicular joint. Orthop Clin North Am 18(3):433–438
Poigenfurst J, Rappold G, Fischer W (1992) Plating of fresh clavicular fractures: results of 122 operations. Injury 23(4):237–241
Post M (1989) Current concepts in the treatment of fractures of the clavicle. Clin Orthop Relat Res 245:89–101
Zenni EJ Jr, Krieg JK, Rosen MJ (1981) Open reduction and internal fixation of clavicular fractures. J Bone Joint Surg Am 63(1):147–151
Neer CS II (1960) Nonunion of the clavicle. J Am Med Assoc 172:1006–1011
Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA (2002) A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis 61(1–2):32–39
Deafenbaugh MK, Dugdale TW, Staeheli JW, Nielsen R (1990) Nonoperative treatment of Neer type II distal clavicle fractures: a prospective study. Contemp Orthop 20(4):405–413
Webber MC, Haines JF (2000) The treatment of lateral clavicle fractures. Injury 31(3):175–179
Tambe AD, Motkur P, Qamar A, Drew S, Turner SM (2006) Fractures of the distal third of the clavicle treated by hook plating. Int Orthop 30(1):7–10
Robinson CM, Cairns DA (2004) Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am 86-A(4):778–782
Flinkkila T, Ristiniemi J, Hyvonen P, Hamalainen M (2002) Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop Scand 73(1):50–53
Levy O (2003) Simple, minimally invasive surgical technique for treatment of type 2 fractures of the distal clavicle. J Shoulder Elbow Surg 12(1):24–28
Flinkkila T, Ristiniemi J, Lakovaara M, Hyvonen P, Leppilahti J (2006) Hook-plate fixation of unstable lateral clavicle fractures: a report on 63 patients. Acta Orthop 77(4):644–649
Kona J, Bosse MJ, Staeheli JW, Rosseau RL (1990) Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma 4(2):115–120
Jackson WF, Bayne G, Gregg-Smith SJ (2006) Fractures of the lateral third of the clavicle: an anatomic approach to treatment. J Trauma 61(1):222–225
Wang SJ, Wong CS (2008) Extra-articular knowles pin fixation for unstable distal clavicle fractures. J Trauma 64(6):1522–1527
Shin SJ, Roh KJ, Kim JO, Sohn HS (2009) Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury
Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR (1997) Type 2 fractures of the distal clavicle: a new surgical technique. J Shoulder Elbow Surg 6(4):380–382
Chen CH, Chen WJ, Shih CH (2002) Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma 52(1):72–78
Bezer M, Aydin N, Guven O (2005) The treatment of distal clavicle fractures with coracoclavicular ligament disruption: a report of 10 cases. J Orthop Trauma 19(8):524–528
Herrmann S, Schmidmaier G, Greiner S (2009) Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury 40(3):236–239
Yamaguchi H, Arakawa H, Kobayashi M (1998) Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop 22(6):366–368
Jin CZ, Kim HK, Min BH (2006) Surgical treatment for distal clavicle fracture associated with coracoclavicular ligament rupture using a cannulated screw fixation technique. J Trauma 60(6):1358–1361
Kao FC, Chao EK, Chen CH, Yu SW, Chen CY, Yen CY (2001) Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma 51(3):522–525
Nordqvist A, Petersson C, Redlund-Johnell I (1993) The natural course of lateral clavicle fracture. 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand 64(1):87–91
Haidar SG, Krishnan KM, Deshmukh SC (2006) Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg 15(4):419–423
Kalamaras M, Cutbush K, Robinson M (2008) A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg 17(1):60–62
Lee YS, Lau MJ, Tseng YC, Chen WC, Kao HY, Wei JD (2008) Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop
Ballmer FT, Gerber C (1991) Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br 73(2):291–294
Fazal MA, Saksena J, Haddad FS (2007) Temporary coracoclavicular screw fixation for displaced distal clavicle fractures. J Orthop Surg (Hong Kong) 15(1):9–11
Macheras G, Kateros KT, Savvidou OD, Sofianos J, Fawzy EA, Papagelopoulos PJ (2005) Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics 28(7):693–696
Mall JW, Jacobi CA, Philipp AW, Peter FJ (2002) Surgical treatment of fractures of the distal clavicle with polydioxanone suture tension band wiring: an alternative osteosynthesis. J Orthop Sci 7(5):535–537
Kashii M, Inui H, Yamamoto K (2006) Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res 447:158–164
Mizue F, Shirai Y, Ito H (2000) Surgical treatment of comminuted fractures of the distal clavicle using Wolter clavicular plates. J Nippon Med Sch 67(1):32–34
Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T (2007) Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg 127(3):191–194
Renger RJ, Roukema GR, Reurings JC, Raams PM, Font J, Verleisdonk EJ (2009) The clavicle hook plate for Neer type II lateral clavicle fractures. J Orthop Trauma 23(8):570–574
Fann CY, Chiu FY, Chuang TY, Chen CM, Chen TH (2004) Transacromial Knowles pin in the treatment of Neer type 2 distal clavicle fracturesA prospective evaluation of 32 cases. J Trauma 56(5):1102–1105; discussion 1105–1106
Scadden JE, Richards R (2005) Intramedullary fixation of Neer type 2 fractures of the distal clavicle with an AO/ASIF screw. Injury 36(10):1172–1175
Badhe SP, Lawrence TM, Clark DI (2007) Tension band suturing for the treatment of displaced type 2 lateral end clavicle fractures. Arch Orthop Trauma Surg 127(1):25–28
Haidar SG, Singh Shergill G (2007) Re: clavicular hook plate for lateral end fractures: a prospective study. Injury 38(2):252–253
Conflict of interest
There is no conflict of interest among the authors.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Oh, J.H., Kim, S.H., Lee, J.H. et al. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg 131, 525–533 (2011). https://doi.org/10.1007/s00402-010-1196-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-010-1196-y