Abstract
Introduction
The occurrence of exaggerated femoral anteversion and the role of femoral derotation osteotomy in developmental dysplasia of hip, especially early walking age group are controversial.
Method
We evaluated femoral anteversion, acetabular anteversion, acetabular index in 15 dislocated hips and 11 normal hips in cases of unilateral dislocation of hip in DDH of age group 12–48 months. We correlated this femoral anteversion with the intra operative “test of stability” which is described by Zadeh et al. We found that there was no statistically significant difference in femoral anteversion between dislocated and normal hips. In all the 15 cases we did open reduction by anterior approach (Somerville approach) and evaluated the position for maximum stability. In 3 cases we were unable to perform test of stability as they needed femoral shortening for reduction of joint.
Results
In the rest 12 hips, 10 were stable in flexion and abduction while 2 were stable in flexion. None of the hips required internal rotation for stability. Hence we did salters osteotomy in all the hips and femoral shortening through lateral approach in 3 cases. At a minimum follow up of 18 months all the hips were clinically stable and none of them dislocated till final follow up. The mean correction of acetabular index was 15.4° and the outcome was excellent in 8 hips and good in 7 hips as per modified McKay’s criteria. Hence we recommend that femoral derotation osteotomy is not needed in DDH of early walking age group.
Conclusion
As the surgical treatment of DDH involves complex osteotomies around the hip and these surgeries have effect on long term outcome, MRI evaluation of femoral anteversion as a part of pre operative evaluation is advised. Also, as the intra operative evaluation needs enough clinical experience and it can not be performed in cases requiring femoral shortening for reduction, we consider pre operative evaluation of femoral anteversion by MRI as essential rather than adjunctive.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The association of femoral anteversion (FAV) with developmental dysplasia of hip (DDH) has always been a matter of curiosity. Regarding the surgical management of DDH, in early walking age group there are few established guidelines with respect to femoral derotation osteotomy (DRO) in whom to do and when to do if needed. Most of the recommendations are based on clinical evaluation. In 2000 Zadeh et al. [18] described a “test of stability” to determine when to do DRO which is based on intra operative analysis. Various surgeons have achieved good–fair outcomes in surgical management of DDH by both doing and not doing DRO [6, 10, 11]. The rationale to do a DRO was hardly supported by any radiological evaluation in all these studies. Under/over correction of FAV has been quoted as one of the common causes for recurrent dislocation in DDH after surgery [5]. Role of radiology was always confined to confirmation of diagnosis in DDH. However, it was only after the advent of CT/MRI, it was possible to assess accurately the FAV in DDH and soon they became an important part of pre operative evaluation in DDH. Several studies based on CT/MRI analysis have documented exaggerated FAV in DDH but there are also many contradictory to this [1, 4, 13, 15]. Most of them were in wide range of age populations and a few correlated their findings with surgical evaluation and clinical outcomes.
In the present study, we evaluated FAV, acetabular anteversion (AAV), acetabular anteversion of the cartilage anlage (CAAV), acetabualr index (AI) in DDH children of early walking age group (12–48 months) by MRI as a part of pre operative assessment and correlated this with intra operative analysis and follow up clinical evaluation.
Materials and methods
We included in our study 15 cases of unilateral dislocated cases of DDH (confirmed by X-rays) in early walking age group ranging from 12 to 48 months (mean age of 23.91 months) in whom single stage surgery was planned. All the 15 cases, X-ray pelvis with both hips AP view was done and hips were classified according to Ishida’s criteria. Fifteen were dislocated hips, 11 were normal hips, 3 were dysplastic hips, and 1 was subluxated hip [8]. Male to female ratio was 3:12. In 12 hips it was left side involvement while it was right sided in 3 hips. In all the cases, MR evaluation of FAV, AAV, CAAV, AI was done as a part of preoperative analysis. But for statistical analysis we excluded the dysplastic and subluxated hips and we compared dislocated hips with the normal hips. We excluded the patients who had previous operative or non-operative treatment for DDH because the treatment could alter the acetabular and femoral neck anatomy. Also the patients with neuromuscular disease or teratologic dislocations (e.g., arthrogryposis or genetic syndromes) were excluded from this study.
MRI evaluation
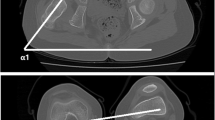
Femoral anteversion was analyzed by the method described by Tomczak et al. [16]. Oblique axial-to-sagittal sections were placed parallel to the femoral neck axis exactly perpendicular to the table. A single image that showed the centers of the head and femoral neck and therefore allowed visualization of the true neck axis was obtained. The alpha angle between the neck axis and a horizontal reference line was calculated (Fig. 1a). Then an axial section through the center of the distal femoral condyles was obtained. The beta angle between the posterior tangent to the femoral condyles and a horizontal reference line was determined (Fig. 1b). Because of the rotation, femoral anteversion was calculated by subtraction (external rotation) of the beta angle from the alpha angle.
a Twenty-four months old female child with right dislocated hip. T1-weighted MR image showing, entire neck in profile. Alpha angle between femoral neck axis and horizontal reference line is measured to be 58°. b T1-weighted MR image of right distal femur (dislocated side) of the same child measuring the beta angle between posterior condylar axis and horizontal reference line which is 32°. Hence femoral anteversion is 58(alpha) − 32(beta) = 26°
Acetabular anteversion was analyzed in the axial sections placed parallel to the pelvic obliquity showing both the triradiate cartilages. AAV was expressed as the angle between line perpendicular to the trans-triradiate line and a line drawn across the margins of the acetabulum, from its posterior to the anterior edge. Similar measurements were also made for the cartilaginous model [4].
The AAV, FAV, AI values of the 11 normal hips were obtained simultaneously and they served as controls. Unpaired t test was applied to analyze the significance of difference between the 2 groups.
In order to assess the reproducibility of the method of measurement of various parameters, all the variables were re evaluated by the same surgeon 4 weeks later. Intra class correlation co-efficient was applied to assess the reproducibility. All the statistical analysis was done using SPSS 12.0 software.
Surgical technique
Single stage open reduction with or without femoral shortening osteotomy/pelvic (Salter’s) osteotomy was done under general anaesthesia by an experienced surgeon. All the surgeries were done by the same surgeon to avoid the technique variation and inter-observer variation. Anterior open reduction was done through an oblique “Bikini” incision as described by Somerville [14].
Test of stability [18]
This was done wherever possible to determine the position of maximum stability of the hip. Stable reduction was considered to be present when the hip remains reduced with axial loading with the leg in 30° flexion, 30° abduction, and 30° internal rotation. Now the various components of this position were sequentially removed beginning with flexion, to identify the position in which the leg must be placed for maximum stability.
Femoral shortening [17]
Osteotomy for femoral shortening when needed was done through a separate lateral incision. Fixation is with low contact dynamic compression plate.
Pelvic (Salter’s) osteotomy [12]
Salter’s osteotomy was done by classical technique as described by Salter through the same incision used for open reduction when the hip was found to be stable in 30° flexion and 30° abduction or 30° flexion only. Osteotomy was fixed with triangular bone graft taken from anterior superior iliac spine region with 2 k-wires.
In cases where we were unable to perform the test of stability as they needed femoral shortening to reduce the hip we did open reduction along with femoral shortening and salters osteotomy. Proper capsulorrhaphy was performed to avoid lax joint capsule in all the cases.
Post operatively the reduced hip was maintained in a hip spica for 6 weeks followed by an abduction brace for 6 weeks more. In follow up period clinical evaluation according to the modified McKay’s criteria [3] was done at 3 months, 6 months, 12 months and at 2 years. In all cases acetabular index in X-rays was also evaluated during the follow up period. All the hips with a minimum follow up of 18 months were included in our study.
Results
X-ray evaluation
As per Ishida’s criteria, of 30 hips 15 were dislocated hips with a mean acetabular index of 38.20° + 3.46° (mean + SD), while 11 were normal hips with a mean acetabular index of 17.63° + 2.15°. Evaluation of acetabular index 4 weeks later showed it to be 37.73° + 2.78° on the dislocated side, while it was 17.54° + 1.75° on the opposite side.
MR evaluation
In none of the cases the FAV exceeded 30° on the dislocated side. The mean values of all the 4 variables FAV, AAV, CAAV, and AI in both the dislocated group and normal group are given in Table 1. Also mentioned in the table are values evaluated after 4 weeks by the same analysist to look for intra observer variability. Comparison of FAV in both the groups was found to be statistically insignificant (P value = 0.345) while comparison of AAV, CAAV, AI in both the groups was highly significant (P value < 0.00).
Reliability analysis for all the 5 variables including acetabular index in X-rays was analyzed by intra class correlation co-efficient and is shown in Table 2.
Correlation analysis among the various variables showed a strong positive correlation between AAV and CAAV, as well between AI and acetabular index measured on x ray. The Spearmann’s correlation co-efficient was 0.790 and 0.855, respectively, while the correlation among the other variables was found to be insignificant.
Surgical assessment
In all the 15 cases we were able to achieve concentric open reduction, however, 3 hips needed femoral shortening to achieve this. In rest 12 hips we assessed the position of maximum stability with the aid of “test of stability”. Ten hips needed flexion and abduction for stability, 2 hips needed flexion only for stability and none of the hips needed internal rotation for stability. In the 3 cases where we were unable to perform the test of stability we did not do femoral DRO as in all these 3 cases the pre operative MRI evaluation did not show any exaggerated FAV (25°, 22°, and 21°, respectively). Hence in all the 15 hips salters osteotomy was done along with open reduction. Femoral DRO was done in none of the cases.
Follow up
All the hips were clinically stable at final follow up (mean 21.2 months) and none of the hips dislocated during this period. According to modified McKay’s grading 8 hips had excellent outcome while the remaining 7 hips had good outcome (Table 3 ). The mean acetabular index at final follow up was 17.63° + 2.15°, thus mean decrease in the acetabular index compared to pre operative X-rays was 15.4° (Fig. 2a, b). We did not find any significant correlation between any of the radiological parameters and final functional outcome.
a Pre operative X-ray of 14 months old female child showing dislocated hip on the left side with an acetabular index of 44°. b Post operative X-ray of the same child as shown in Fig. 1a at a follow up of 8 months showing a reduced stable hip with adequate supero lateral coverage of the head. The acetabular index is 21° with a correction of 23°
Discussion
Regarding the patho anatomy of bony structures in DDH, it is said that the basic etiopathogenesis of DDH lies in acetabulum. Germinal failure of development of postero superior buttress of ilium leads to a flat socket. The changes occurring in the femur are considered to be secondary changes due to persistent dislocation [2]. Authors like Jansen, Bruce, Morrison, Hey Groves, Fairbank are of the strong belief that femoral anteversion is a secondary adaptive change of femur that occurs gradually as the child walks with a dislocated hip [2]. Further strengthening this, Herring has stated that they did not find increased femoral anteversion, valgus in DDH and did not recommend any routine varus derotation osteotomy for femur [7]. Sugano et al. [15] did CT analysis of femur in 35 cases of DDH in adult patients and found an increase in anteversion by 10–14°. Their samples were also adult femora thus supporting the concept that increase in femoral anteversion might be an adaptive change.
Sezgin et al. [13] documented CT analysis where they compared 25 dislocated hips with 10 normal hips in DDH. The mean age was 32.3 months ranging from 12 to 48 months that is early walking age group. They found a femoral anteversion of 32.9° + 6.4° in the dislocated group and 30.7° + 6.1° in the normal group. The difference was insignificant (P value = 0.378). While in our study it was found to be 23.06 + 4.36° on the dislocated side, while on the normal side it is 21.36° + 4.56°. The difference between them is statistically insignificant (P value = 0.345). Though the results obtained in both studies are similar the mean femoral anteversion in Sezgin’s study was higher compared to our study. This can be explained by the difference in the technique used. They used the CT as mode of evaluation and in CT the measured angle is head trochanter angle which is higher than the true neck angle.
Oshako et al. [11] achieved 72% good results in 22 hips and in all of them DRO of femur was done. Similar results with DRO were also obtained by Nakamura et al. [10]. Contrary to this Haidar et al. [6] achieved 97.35% good results in 37 hips in which only Salters osteotomy was done. Lehman et al. [9] compared results of VDRO versus Salters osteotomy and found that results are superior in salters osteotomy group. Some have done DRO in some selective cases based on their intraoperative analysis. Although all the above mentioned studies got good results with various surgeries, none of them proved their point regarding femoral anteversion, radiologically and none had prescribed guidelines when to do DRO.
Fixen et al. [5] reported on recurrent dislocations after innominate osteotomies and stated that the most common causes for recurrent dislocation are poor capsulorrhaphy and under/over correction of FAV. It has been reported that combining femoral DRO with salters osteotomy predisposes for posterior dislocation.
It was Zadeh et al. [18], based on an intra operative test of stability, gave guidelines when to do DRO. Their study included 95 hips with a mean age of 28 months. 81 hips were aged below 4 years and 14 hips were aged more than 4 years. In their study of 95 hips as per their test of stability 66 hips needed DRO, stating that increased femoral anteversion is common in DDH. But they had no radiological evidence to prove the increased femoral anteversion on the dislocated side. In our study contrary to their findings we found that none of our hips needed internal rotation for stability (30°) and this was also supported by our MR analysis of FAV where none of the dislocated hips had FAV exceeding 30° and the difference in FAV when compared to the normal hips was insignificant.
Further “test of stability” can only be done in cases where we can achieve reduction of the joint while in cases which need femoral shortening it is not possible to perform this test and in such situations pre operative radiological assessment of FAV always helps. As clinical decision making as per intra operative assessment always needs enough clinical experience it is always better to have a pre operative radiological assessment when feasible.
The limitations of this study are the sample size is small and the follow up period is short to comment on the incidence of avascular necrosis and premature physeal closure. Also these complications can be picked up early if post operative MRI had been done. But due to lack of consent only 4 out of 15 cases got post operative MRI done, in our series and this is not adequate to comment on these complications. We selected 18 months as minimum follow up period because the main theme of our study is evaluation of anteversion and the most common complication of under/over correction of anteversion is recurrent dislocation which occurs in the early post operative period, once the child is out of spica/brace. As per our protocol all the patients were put in a cast for 6 weeks followed by an abduction brace for 6 weeks. Hence we could found out any dislocation if at all had occurred during this follow up.
We believe that the majority of the abnormalities in early walking age patients with DDH are on the acetabular side and changes on the femoral side in older children seem to be secondary to pressure effects on the femoral head from the acetabulum or ilium due to persistent dislocation. Hence we conclude that exaggerated femoral anteversion is not come across in early walking age group as shown by our MRI analysis and femoral DRO is not needed in them as shown by our intraoperative and follow up analysis. We recommend that evaluation of femoral and acetabular patho anatomy is essential rather than an adjunctive in pre operative planning for DDH to avoid complications and for this we recommend MR as the modality of choice, as always a radiation free imaging is preferred.
References
Anda S, Terjesen T, Kvistad KA, Svenningsen S (1991) Acetabular angles and femoral anteversion in dysplastic hips in adults:CT investigation. J Comput Assist Tomogr 15:115–122
Badgley CE (2008) The etiology of congenital dislocation of hip. Clin Orthop Relat Res 466:90–103
Barrett WP, Staheli LT, Chew DE (1986) The effectiveness of Salter’s innominate osteotomy in the treatment of congenital dislocation of the hip. J Bone Joint Surg Am 68-A:79–86
Catherine M, Taylor FN, Lee C, Graham HK, Nattrass GR (2002) MRI evaluation of surgical management in developmental dysplasia of hip in childhood. J Pediatr Orthop 22:92–97
Fixsen JA (1987) Anterior and posterior subluxation of hip following innominate osteotomy. J Bone Joint Surg Br 69-B:361–366
Haidar RK, Jones RS, Vergroesen DA (1996) Simultaneous open reduction and salter innominate osteotomy for developmental dysplasia of the hip. J Bone Joint Surg Br 78-B:471–476
Herring JA (2002) Developmental dysplasia of the hip. In: Tachdjian’s pediatric orthopaedics, vol 1, 3rd edn. W.B. Saunders, Philadelphia, pp 513–654
Ishida K (1977) Prevention of the development of the typical dislocation of the hip. Clin Orthop 126:167–169
Lehman WL, Grogan DP (1985) Innominate osteotomy and varus derotational osteotomy in the treatment of congenital dysplasia of the hip. Orthopedics 8:979–986
Nakamura M, Matsunaga S, Yoshino S, Ohnishi T, Higo M, Sakou T (2004) Longterm result if combination of open reduction and femoral varus derotation osteotomy with shortening for developmental dislocation of hip. J Pediatr Orthop 13:248–252
Oshako H, Sakou T, Matsunaga S (1998) Open reduction and varus derotation osteotomy with shortening in treatment of congenital dislocation of hip. J Orthop Sci 3:304–309
Salter RB (1961) Innominate osteotomy in the treatment of congenital dislocation of hip. J Bone Joint Surg Br 43-B:518–529
Sezgin S, Adil O, Hasan T (2005) Anteversion of the acetabulum and femoral neck in early walking age patients with developmental dysplasia of the hip. J Pediatr Orthop B 14:410–414
Somerville EW (1957) The direct approach to developmental dislocation of hip. J Bone Joint Surg Br 39-B:623–627
Sugano N, Noble PC, Kamaric E, Salama JK, Tullos HS (1998) The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br 80B:711–717
Tomezak RJ, Guenther KP, Rieber A, Mergo P, Ros PR, Brambs HJ (1997) MR imaging Measurement of femoral anteversion as a new technique: comparison with CT in children and adults. Am J Roentgenol 168:791–798
Wenger DR (1989) Congenital dislocation of the hip: techniques for primary open reduction including femoral shortening. Instr Course Lect 38:343–351
Zadeh HG, Catterall A, Hashemi-Nejad A, Perry RE (2000) Test of stability as an aid to decide the need of osteotomy in association with open reduction in developmental dislocation of hip. J Bone Joint Surg Br 82B:12–19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mootha, A.K., Saini, R., Dhillon, M. et al. Do we need femoral derotation osteotomy in DDH of early walking age group? A clinico-radiological correlation study. Arch Orthop Trauma Surg 130, 853–858 (2010). https://doi.org/10.1007/s00402-009-1020-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-009-1020-8