Abstract
Background
To determine the effectiveness of three different local injection modalities in the treatment of lateral epicondilitis.
Methods
In a prospective randomized study on lateral epicondilitis, 75 patients were divided into three equal groups A, B and C (n = 25) and were treated using three different method of local injection. The patients in group A were treated with local injection of a steroid (1 mL triamcinolone) combined with local anaesthetic (1 mL lidocaine), those in group B were treated with injection of local anaesthetic (1 mL lidocaine) combined with peppering technique and those in group C with local injection of a steroid (1 mL triamcinolone) combined with local anaesthetic (1 mL lidocaine) and peppering technique. The outcome was defined by measuring the elbow pain during the activity using a 10-cm visual analogue scale (VAS) and satisfaction with the treatment using a scoring system based on the criteria of the Verhaar et al. at 3 weeks and 6 months after the injection and compared with the pre-treatment condition.
Results
There were significant (P = 0.006) differences in the successful outcomes between the three groups at 6 months. In group C in which local steroid + peppering injection technique were used; excellent results were obtained in 84% of patients comparing to 36% and 48% for patients in groups A and B, respectively. The successful outcomes were statistically higher in group C comparing to group A (P = 0.002) and group B (P = 0.011). In all groups, there was a significantly lower pain (VAS) at the 3-week and 6-month follow-ups comparing to the pre-treatment condition. VAS measured at 6-month follow-up were significantly lower in group C comparing to other groups (P = 0.002).
Conclusion
In the treatment of lateral epicondilitis, combination of corticosteroid injections with peppering is more effective than corticosteroid injections or peppering injections alone and produces better clinical results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tennis elbow, lateral epicondylitis of the humerus is an enthesopathy of the common extensor origin. The pathogenesis of lateral epicondylitis has not been determined with any certainty. The general opinion is that the condition is due to overuse [6, 12, 15, 18]. Epicondilytis may be a misleading term as there is no traditional inflammation [1, 15]. The histological findings may include granulation tissue, micro rupture and degenerative changes [11, 14, 15, 18].
Many treatment modalities have been described for lateral epicondylitis including rest, modification of activity, splints, analgesic and anti-inflammatory drugs, physiotherapy, acupuncture, injections and surgery, have all been investigated and have shown to end up with variable clinical benefit.
Targeting the common extensor origin, various substances have been used for injection treatment, including corticosteroids, platelet-rich plasma and autologous blood [5, 13]. Price et al. [16] have showed the preference for the use of injections of steroid (triamcinolone) in the management of tennis elbow. In another study, Verhaar et al. [24] have found that the steroid (triamcinolone) injections were more effective than physiotherapy. But the recurrence of symptoms after initial reduction or disappearance of pain has been reported [16, 24].
Rompe et al. [19, 20] have described the use of low-dose ESWT in patients with chronic tennis elbow with promising results. However, Crowther et al. [7] have found that in the medium term, local injection of steroid is more successful and 100 times less expensive than ESWT in the treatment of tennis elbow.
Despite of the various clinical results, the preferred method of treatment most often is local corticosteroid injection with or without addition of a local anaesthetic [4, 11, 22].
In a prospective randomized study Altay et al. [2] have assessed local injections for lateral epicondylitis and found peppering technique to be as effective as corticosteroid injection. They described this technique as a reliable and alternative method of treatment. Technically peppering is achieved by inserting, injecting, withdrawing without emerging from the skin, slightly redirecting, and reinserting. Surprisingly, only one randomized controlled trial has discussed the role of the peppering in the treatment of lateral epicondylitis.
In the current study, the effect of combining local corticosteroid injection with peppering was evaluated by comparing its effects with the local peppering injection technique and a local steroid injection alone, in a prospective controlled trial.
Materials and methods
The series consisted of 75 patients with lateral epicondylitis. The trial was approved by the local ethical committee and every patient gave informed consent.
The criteria for inclusion were: pain and tenderness over the extensor origin in the forearm, a positive chair test with pain in the region of lateral epicondyle when a chair is lifted with one hand in a position with the forearm pronated and the wrist is in flexion [9], and positive tennis elbow pain test (Mills’ sign) with pain in the lateral epicondyle when the elbow is actively moved from flexion to full extension with the forearm in the prone position and the wrist in flexion [8].
Exclusion criteria were surgery for lateral epicondylitis, previous injections for lateral epicondylitis, arthritis, effusion about the elbow, entrapment of the ulnar nerve, radiculopathy from the cervical spine, peri-articular fracture, distal humeral bone tumour, infection, and abnormal erythrocyte sedimentation rate.
The first 25 consecutive patients in group A were treated by local injection of triamcinolone (1 mL) combined with 1 mL of lidocaine, the second 25 in group B by 1 mL of lidocaine and with peppering, the third 25 in group C were treated using local injection of 1 ml triamcinolone combined with 1 mL of lidocaine with peppering injection technique. The patients were blinded to the type of injection.
The baseline characteristics in each group including the age, affected side, previous treatment methods including using NSAID, physiotherapy, splints, and the duration of pain were recorded and the mean in each group was tabulated (Table 1).
All the patients in the study were seen after 3 weeks, and later 6 months after the beginning of the treatment. No additional medication was given and no restriction of activity was advised. The patients were evaluated by reviewers who were blinded to the method of the study at 3 weeks and 6 months after the injections.
Clinical assessment consists of routine clinical history, a patient assessed 0–10 on the visual analogue scale (VAS) of pain, where zero reflected the total absence of symptoms and ten the worst imaginable pain. The outcome was, compared with the pre-treatment condition.
The rating, according to the criteria of the Verhaar et al. [23], was defined as excellent (no pain, patient satisfied with the treatment outcome, no subjective loss of grip strength and no pain provoked by resisted dorsiflexion of the wrist), good (symptoms substantially decreased, patient satisfied with the treatment outcome, occasional slight pain on the lateral epicondyle after strenuous activities, no or slight subjective loss of grip strength, and no pain provoked by resisted dorsiflexion of the wrist), fair (discomfort on the lateral epicondyle after strenuous activities but at a more tolerable level than before treatment, patient satisfied or moderately satisfied with the result of treatment, slight or moderate subjective loss of grip strength, and slight or moderate pain provoked by resisted dorsiflexion of the wrist), or poor (no decrease of pain of the lateral epicondyle, patient dissatisfied with the result of treatment, severe subjective loss of grip strength and severe pain provoked by resisted dorsiflexion of the wrist). Treatment was considered successful when the patient had an excellent or a good score.
Injection technique
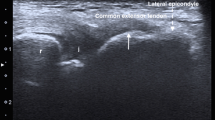
We used the technique described by Altay et al. [2] for peppering injection. As the patient lies supine on the examination table with the elbow in 90° flexion and neutral rotation position, the elbow was prepared using an antiseptic solution. The point of maximum tenderness is peppered with small injections by inserting an 18-gauge needle, injecting, and withdrawing without emerging from the skin, slightly redirecting, and reinserting. The injections are continued until the sensation of a crepitus or cracking, which was felt at the beginning, was lost, this required 40–50 shots. The needle should be inserted lightly to avoid damage to its tip, if the bone is contacted.
The SPSS package (version 11.5, SPSS Inc, Chicago, IL, USA) was used for all statistical calculations. Chi square test were used to compare the excellent and good results among the groups. The Kruskal–Wallis test was applied to compare VAS score changes before and after local injection. Differences in VAS over time within the groups were calculated using the Wilcoxon signed ranks test. The P value was set to 0.05.
Results
There was no statistically significant difference between the groups with respect to sex, mean age and the duration of symptoms (P > 0.05) (Table 1).
At the 3-week follow-up, the patients who were not fully satisfied were offered an additional injection. The rate of additional injection was statistically lower in group C (16%) when compared to group B (44%) (P = 0.031), but no statistically significant difference was observed comparing to group A (32%) (P = 0.185), and there was no statistically significant difference between groups A and B (P = 0.382) (Table 1).
At the 3-week follow-up, there were no significant differences in the pain measured using VAS between the three groups (P = 0.155). Successful treatment was reported by 23 (92%) patients in group A, 24 (96%) patients in group B and 20 (80%) for group C. The patients in all groups had a significantly lower VAS (pain during grip activity) post-treatment than they had pre-treatment (P = 0.000). Outcome for each group is shown in Table 2.
At the 6-month follow-up lateral epicondylar pain measured using the VAS were 0.84 in group A, 0.56 in group B as compared to 6.32 and 7.72 before the commencement of the treatment, and 0.12 in group C compared to pre-treatment scores of 7.20. There was statistically significant difference between the groups in the VAS measured at six months (P = 0.002) (Table 2). The improved VAS results in group C were significantly superior comparing to group A (P = 0.001). There was no statistically significant difference in the improved VAS results between group A and group B (P = 0.465), and between group B and group C (P = 0.08) (Table 2) (Fig. 1)
At the 6-month follow-up successful treatment (excellent + good) was reported by 22 (92%) patients in group A, 24 (96%) patients in group B and 25 (100%) for group C.
The rate of successful results was higher in group C when compared to groups A and B. There was also statistically significant differences in the successful results between group C and groups A and B (P = 0.006), but no statistically significant difference was observed between group A and B (P = 0.536) (Table 3).
All patients found the injection painful. No complications or adverse effects attributable to injections were observed during the study.
Discussion
The main finding in our study was that combining the peppering technique with local injection of steroid (group C) was more effective than local injection of steroid (group A) or local injection using the peppering technique (group B) in the treatment of lateral epicondylitis. No difference was found between local steroid injection (group A) or local injection using the peppering technique (group B). Furthermore, this study revealed that combining the steroid with peppering injection technique has reduced the additional injections in the third week of treatment significantly, comparing to the peppering technique (group B).
We agree with the findings of Smidt et al. [21] that steroid injections are the best option in the short term for patients with tennis elbow. In the current study the rates of excellent results in the 3-week follow-up were higher in groups were steroid were used in the injections (A and C). In the 6-month follow-up the excellent results were higher in the group were the steroid combined with peppering injection technique (group C) and lowest rates were found in the group treated with steroid injection alone (group A).
Altay et al. [2], in a prospective randomized study of lateral epicondylitis, has compared the peppering injection technique to (steroid + peppering) injection technique. In that study, at 6-month follow-up, excellent results were achieved in 93% of the patients in the group treated with local peppering and 95% of the patients in the group treated with (steroid + peppering). They found no significant differences in the rate of excellent results, satisfaction and success between the two groups.
In the current study excellent results were achieved in 84% of the patients treated using the steroid +peppering (group C) injections. However, the rate of excellent results was 48% for those treated with local peppering alone injections (group B) and 36% for the group treated with local steroid injection alone (group A). The rate of successful results was significantly higher in group C comparing to groups A and B.
In the current study, to diminish the local irritation and pain during injections, a local anaesthetic addition has been used in all groups. In the long term results, local anaesthetic plays no role in treating lateral epicondilitis. Solveborn et al. [22], in a prospective randomized study of lateral epicondylitis, has compared the effects of adding the short acting local anaesthetic, lidocaine, and the long acting bupivacaine to local steroid injection. The only difference was found at 2-week follow-up were bupivacine yielded a better outcome. The long term effects of local anesthetics were equal to that of a placebo.
Local corticosteroid injections have been used for treatment of lateral epicondilitis for many years, with varying results. Verhaar et al. [24] carried out a prospective, randomized trial on 106 patients to compare the effect of local injection of steroid with Cyriax-type physiotherapy. They used triamcinolone with lignocaine and concluded that the injections were more effective than physiotherapy. Hay et al. reported a study of 164 patients randomized to steroid injection, non-steroidal anti-inflammatory medication or a placebo. The injections gave rapid resolution of symptoms, but did not influence the long-term outcome. At 1 year there was no difference between the groups [10]. According to Boyer and Hastings, “if corticosteroid has any effect on patients with lateral Tennis elbow, it is of a short duration” [4]. A recent randomized controlled trial by Bisset et al. [3] found superior effects for physiotherapy compared with corticosteroid injections, in the long term (52 weeks) results.
Altay et al. [2] found no difference between local cortisone and local anaesthetic injection, using the peppering technique. In a review of the literature, Labelle et al. [11] reported a 66% recurrence rate, 6 months after corticosteroid injection treatment. This means that there are significant variations in the clinical results, with respect to the effectiveness of corticosteroid injections in the treatment of lateral epicondilitis.
The peppering technique of injection in the treatment of lateral epicondylitis was described 44 years ago [17]. The peppering technique probably act by creating new channels through the degenerative myxoid tissue, in which bleeding occurs; this may initiate the mode of healing in lateral epicondylitis [2].
The results of the current study suggest that, the local corticosteroid injection becomes more effective and lower the rate of required additional injections when combined with peppering in treating patients with lateral epicondylitis. This combination could be an effective alternative to the corticosteroid injection taking into account the complication of the repeated corticosteroid injections and its questionable role in treating patients with lateral epicondylitis.
Conclusion
This is the second study designed for the evaluation of the effects of combining peppering and steroid injection in the treatment of lateral epicondylitis. When local injection is considered in the treatment of lateral epicondylitis, local steroid injection with peppering may be the first choice of treatment as it has the highest success rate and may prevent the complications of further injections.
References
Alfredson H, Ljung BO, Thorsen K et al (2000) In vivo investigation of ECRB tendons with microdialysis technique—no signs of inflammation but high amounts of glutamate in tennis elbow. Acta Orthop Scand 71:475–479. doi:10.1080/000164700317381162
Altay T, Günal I, Oztürk H (2002) Local injection treatment for lateral epicondylitis. Clin Orthop Relat Res 398:127–130. doi:10.1097/00003086-200205000-00018
Bisset l, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B (2006) Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. Br Med J 333:41–939. doi:10.1136/bmj.38961.584653
Boyer MI, Hastings HII (1991) Lateral tennis elbow: “Is there any science out there?” J Shoulder Elbow Surg 8:481–491. doi:10.1016/S1058-2746(99)90081-2
Connell DA, Ali KE, Ahmad M et al (2006) Ultrasound-guided autologous blood injection for tennis elbow. Skeletal Radiol 35:371–377. doi:10.1007/s00256-006-0081-9
Coonrad RW, Hooper WR (1973) Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg 55:1177–1182
Crowther MA, Bannister GC, Huma H, Rooker GD (2002) A prospective, randomised study to compare extracorporeal shock-wave therapy and injection of steroid for the treatment of tennis elbow. J Bone Joint Surg Br 84-B:678–679. doi:10.1302/0301-620X.84B5.12741
Friedlander HL, Reid RL, Cape RF (1967) Tennis elbow. Clin Orthop Relat Res 51:109–116
Gardner RC (1970) Tennis elbow: diagnosis, pathology and treatment: nine severe cases treated by a new reconstructive operation. Clin Orthop Relat Res 72:248–253
Hay EM, Paterson SM, Lewis M, Hosie G, Croft P (1999) Pragmatic randomised controlled trial of local corticosteroid injection and naproxen for treatment of lateral epicondylitis of elbow in primary care. BMJ 319:964–968
Labella H, Guibert R, Joncas J et al (1992) Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow: an attempted meta-analysis. J Bone Joint Surg 74B:646–651
Ljung BO, Lieber RL, Friden J (1999) Wrist extensor muscle pathology in lateral epicondylitis. J Hand Surg Br 24:177–183. doi:10.1054/jhsb.1998.0178
Mishra A, Pavelko T (2006) Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 34:1774–1778. doi:10.1177/0363546506288850
Nirschl RP (1992) Elbow tendinosis/tennis elbow. Clin Sports Med 11:851–870
Potter HG, Hannafin JA, Morwessel RM et al (1995) Lateral epicondylitis: correlation of MR imaging, surgical, and histopathologic findings. Radiology 196:43–46
Price R, Sinclair H, Heinrich I, Gibson T (1991) Local injection treatment of tennis elbow: hydrocortisone, triamcinolone and lignocaine compared. Br J Rheumatol 30:39–44. doi:10.1093/rheumatology/30.1.39
Pruce AM, Miller JA, Berger IR (1964) Anatomic landmarks in joint paracentesis. Clinical symposia, Ciba Foundation, pp 23–24
Regan W, Wold LE, Coonrad R et al (1992) Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med 20:746–749. doi:10.1177/036354659202000618
Rompe JD, Hopf C, Kullmer K, Heine J, Burger R (1996) Analgesic effect of extracorporeal shock-wave therapy on chronic tennis elbow. J Bone Joint Surg Br 78:233–237
Rompe JD, Hopf C, Küllmer K, et al. (1996) Low-energy extracorporeal shock wave therapy for persistent tennis elbow. Int Orthop 20:23–27. doi:10.1007/s002640050021
Smidt N, van der Windt DA, Assendelft WJ, Deville WL, Korthals-de Bos IB, Bouter LM (2002) Corticosteroid injections, physiotherapy, or a wait and see policy for lateral epicondylitis: a randomized controlled trial. Lancet 359:657–662. doi:10.1016/S0140-6736(02)07811-X
Solveborn S-A, Buch F, Mallmin H, Adalberth G (1995) Cortisone injection with anesthetic additives for radial epicondylalgia (tennis elbow). Clin Orthop Relat Res 316:99–105
Verhaar J, Walenkamp G, Kester A, van Mameren H, van der Linden T (1993) Lateral extensor release for tennis elbow: a prospective longterm follow-up study. J Bone Joint Surg Am 75:1034–1043
Verhaar J, Walenkamp G, van Mameren H, Kester AD, van der Linden AJ (1996) Local corticosteroid injection versus Cyriax-type physiotherapy for tennis elbow. J Bone Joint Surg Br 78:128–132
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dogramaci, Y., Kalaci, A., Savaş, N. et al. Treatment of lateral epicondilitis using three different local injection modalities: a randomized prospective clinical trial. Arch Orthop Trauma Surg 129, 1409–1414 (2009). https://doi.org/10.1007/s00402-009-0832-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-009-0832-x