Abstract
Introduction
Osteoporosis is a major health problem. Dual energy X-ray absorptiometry (DXA) of the hip and spine is the worldwide standard in diagnosing osteoporosis. Measurement of bone mineral density (BMD) with dual energy X-ray and laser absorptiometry of the calcaneus (Calscan) might be a good alternative. Advantages of the Calscan are that it is quick, widely available and manageable. In this study we compared BMD expressed in T-scores measured by DXA and Calscan. The aim of this study was to define threshold T-scores on the Calscan that could exclude or predict osteoporosis correctly in comparison with DXA.
Materials and methods
Patients ≥50 years attending our emergency department with a fracture were offered osteoporosis screening at our fracture and osteoporosis outpatient clinic (FO-Clinic) and enrolled in this study. BMD was measured at the hip and spine using DXA and at the calcaneus using Calscan. A T-score measured by DXA ≤−2 standard deviations (SD) below the reference population was defined as manifest osteoporosis and was the treatment threshold.
Results
During a 10-month study period, 182 patients were screened with both devices. The mean DXA-T-score was −1.63 SD (range −4.9 to 2.1) and Calscan T-score −1.91 SD (range −5.3 to 1.4). There was a significant correlation between both devices (r = 0.47, P < 0.01). Using an upper threshold for the Calscan T-score of −1.3 SD, 47 patients could be classified as non-osteoporotic with 89.3% sensitivity (95% CI 80.0–95.3%). Using a lower threshold for the Calscan T-score of −2.9 SD, 34 patients could be classified by the Calscan as osteoporotic with 90.7% specificity (95% CI 83.5–95.4). The remaining 101 patients could only be correctly classified by DXA-T-scores.
Conclusion
Although DXA is the established modality worldwide in measuring BMD it is restricted to specialized centres. Peripheral bone densitometers like the Calscan are widely available. When BMD measurements with DXA were compared to Calscan measurements it was possible to correctly classify 81 of 182 patients based on the Calscan T-score. Of these 81 patients 34 could be classified as manifest osteoporotic and 47 as non-osteoporotic. Therefore the Calscan seems to be a promising technique which might be used as a screening device at a FO-Clinic, especially when DXA is not easily available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major health problem, which can be illustrated by the fact that it has been estimated that 50% of Caucasian females over 50 years of age will experience an osteoporosis-related fracture in their lifetimes [15, 16]. By measuring bone mineral density (BMD) it is possible to identify a group of patients which is at increased risk of developing a fracture [11]. Nevertheless, it is not possible to identify individuals who will develop a fracture [11]. A general screening program for osteoporosis can therefore not be recommended but selective screening for people at high risk of osteoporosis might be worthwhile [7, 11, 16]. Nevertheless, 80% of all people at high risk for osteoporosis attending an emergency department with a fracture is not evaluated for osteoporosis [15]. This is a missed opportunity because adequate treatment is known to reduce the risk of another osteoporotic fracture up to 50% [5, 6, 10, 11, 13, 15]. Therefore, case finding osteoporosis is necessary [6, 12]. An active search for osteoporosis, by means of a fracture and osteoporosis outpatient clinic (FO-Clinic), is the best way in case finding osteoporosis and results in identifying 85% of patients at risk [6, 12].
The established modality worldwide in assessing osteoporosis is measurement of BMD with dual energy X-ray absorptiometry (DXA) of the hip or spine [1, 7]. This is due to the fact that DXA is available worldwide and most studies describing the relation between fracture risk and BMD or therapeutic effects are performed using DXA [7]. The disadvantage of DXA is that although it is available worldwide it is restricted to specialized centres. Peripheral measurement devices are widely available and are therefore a more convenient way in establishing BMD [1]. The dual energy X-ray and laser absorptiometry of the calcaneus [Calscan (DXL Calscan; Demetech AB, Solna, Sweden)] is one of these peripheral measurement devices. The Calscan measures BMD at the calcaneus. As the calcaneus is a weight-bearing bone which consists of 95% of metabolic active trabecular bone this might provide an optimal site for the diagnosis of osteoporosis [2]. Combining dual energy X-ray absorptiometry with laser leads to a 10–20% better accuracy compared to conventional DXA technology [9].
The BMD measured, by both DXA and Calscan, is expressed as a T-score, which is the standard deviation (SD) in bone mass compared with the peak bone mass of young adults [8, 9, 19]. Kullenberg et al. [10] have already shown that the age-related decline in T-scores measured with Calscan and DXA are in close concordance and that the diagnostic capabilities of the Calscan are high in diagnosing osteoporosis.
The primary purpose of this study was to compare BMD measured in the calcaneus using the Calscan to BMD measured with DXA of the hip and spine in order to define threshold T-scores on the Calscan that could exclude or predict osteoporosis correctly. The secondary purpose was to diminish the need for DXA examination by measuring BMD with the Calscan.
Materials and methods
Study protocol
Patients ≥50 years who were admitted to our emergency department with a low-energy fracture—for example a fall from standing position or from less than 1 m—were invited to our FO-Clinic. Two research nurses checked the electronic files of all patients admitted to our emergency department on a daily basis and invited all patients fulfilling the inclusion criteria for the FO-Clinic. At the FO-Clinic a standard screening program for osteoporosis was used. This included an intake, blood tests and measurement of BMD by DXA. All data were stored in a database. All 240 patients admitted to this FO-Clinic during the period of March 2005 until June 2005 and from August 2006 until January 2007 were enrolled in this study. In these two periods BMD was measured with both DXA and Calscan. Patients who did not agree after informed consent was given were excluded (Fig. 1).
The study has been conducted in two different periods because we did not have the disposal of a Calscan between June 2005 and August 2006. As nothing changed in the inclusion criteria for the FO-Clinic, the things done when patients were included or the type of Calscan used between both periods all patients were analyzed as one group. A total of 226 patients (94%) underwent bone densitometric evaluation using DXA and 194 (81%) using the Calscan (Fig. 1). No DXA evaluation was performed in 14 patients because these patients refrained from making an appointment for the DXA. No Calscan was performed in 46 patients, due to several reasons. In two patients a Calscan was not performed due to physical deformities and in 44 patients it was not performed due to scheduled service or technical malfunction. Because this is a retrospective study it was not possible to retrieve the exact reasons why Calscans were missed but technical malfunction was never that serious that the Calscan had to be replaced. A total of 182 patients were evaluated with both Calscan and DXA and could be included for further analysis (Fig. 1). Of the 182 patients, 75 were seen in the first study period and 107 in the second study period. A total of 136 patients (75%) were female. The mean age was 66 years ranging from 50 to 86 years. The general data are expressed in Table 1. As can be seen in Table 2 the fractures upon entry into the study were heterogeneous.
Definition of osteoporosis
As this study concerned a fracture population we used the definition of manifest osteoporosis in classification of patients (Table 3). This meant that all patients with a T-score ≤−2.0 SD measured by DXA were classified as osteoporotic [6, 12]. Because most studies comparing Calscan with DXA use the diagnostic World Health Organization (WHO) criteria for osteoporosis, we also calculated the general patient characteristics and threshold T-scores on the Calscan using these criteria (Table 3) [19].
BMD measurement
All Patients admitted to the FO-Clinic were referred to our radiology department for BMD measurement of the hip and lumbar spine using DXA (Hologic Discovery A; Hologic, Bedford, MA, VS). DXA of the left hip and lumbar vertebrae 1–4 was performed unless contraindicated. Both the T-score of hip and spine was stored in our database. In this study the lowest of these two T-scores was used for further analysis and comparison with the Calscan T-score. Scanning time on the DXA took about 20 min and the machine was calibrated automatically on a daily basis using a phantom.
The Calscan (DXL Calscan; Demetech AB, Solna, Sweden) measured BMD at the calcaneus. The Calscan automatically defined the ideal scanning site at the heel, making the results operator independent and follow-up measurements more accurate. An internal phantom automatically calibrated the Calscan before each new patient. The Calscan performance was not affected by normal range of temperature or movement of the device [18]. Scanning time took up to 5 min and could be performed at the FO-Clinic. Results were immediately available.
Establishing threshold T-scores for the Calscan
According to the United Kingdom National Osteoporosis Society (NOS) the Calscan T-score should be interpreted using an upper and lower threshold [1, 4, 18]. These thresholds should be defined in a way that patients with osteoporosis of the hip or spine are identified with 90% sensitivity and 90% specificity [18].
The upper threshold for the Calscan (Tcal-normal) is therefore the Calscan T-score under which 90% of patients with osteoporosis were classified by the Calscan as having osteoporosis (sensitivity). All patients with a Calscan T-score above Tcal-normal were considered not to suffer from osteoporosis. The lower threshold for the Calscan (Tcal-osteoporosis) is the Calscan T-score above which 90% of the patients without osteoporosis were classified by the Calscan as not having osteoporosis (specificity). All patients with a Calscan T-score under or equal to Tcal-osteoporosis were considered to suffer from osteoporosis. These thresholds were calculated using the definition of manifest osteoporosis and using the diagnostic WHO criteria for osteoporosis.
Statistical analysis
Statistical analysis was performed by an independent statistician using SPSS software program (version 14.1 for Windows XP, SPSS, Chicago, Ill., USA). Results were expressed as mean (range) and percentages. A Pearson correlation coefficient was used to assess the relationship between BMD measured by DXA and Calscan. Cross tabulations were performed to assess the thresholds for the Calscan. A 95% CI was calculated for both the sensitivity and specificity.
Results
General data
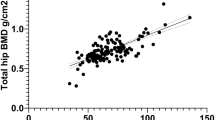
The mean T-score for BMD measured by DXA was −1.63 SD (range −4.9 to 2.1) and by Calscan −1.91 SD (range −5.3 to 1.4). The correlation between DXA and Calscan was r = 0.47 (P < 0.0001) as illustrated in Table 4.
Thresholds on the Calscan using the definition of manifest osteoporosis
A total of 75 out of 182 patients did have a DXA T-score ≤−2.0 SD and could be classified as manifest osteoporotic. As can be seen in Fig. 2 and Table 5, the Tcal-normal is −1.3 SD as 89.3% (95% CI) 80.0–95.3%) of manifest-osteoporotic patients did indeed have a Calscan T-score ≤−1.3 SD and were therefore correctly classified as manifest osteoporotic by the Calscan. Thus all patients with a Calscan T-score >−1.3 SD could be classified as non-manifest-osteoporotic, hereby misclassifying only 10.7% of manifest-osteoporotic patients. The Tcal-osteoporosis must be −2.9 SD as 90.7% of non-manifest-osteoporotic patients did indeed have a Calscan T-score >−2.9 SD (95% CI 83.5–95.4%) (Fig. 2 and Table 5). All patients with a Calscan T-score ≤−2.9 SD could be classified as manifest osteoporotic, hereby misclassifying only 9.3% of non-manifest-osteoporotic patients.
Calscan T-score related to DXA T-score. Patients on the left side of the vertical line crossing the DXA-axis at −2.0 SD do have manifest osteoporosis. Patients on the right side of this line do not suffer from manifest osteoporosis. Tcal-normal: the Calscan T-score under which 90% of manifest osteoporotic patients are classified correctly as manifest osteoporotic (a). Tcal-osteoporosis: the Calscan T-score above which 90% of the patients without manifest osteoporosis are classified correctly as non-manifest-osteoporotic (b)
When both thresholds were used 47 out of 182 (26%) patients did not have to be assessed by DXA because of the low probability of manifest osteoporosis and 34 out of 182 (19%) patients did not need DXA evaluation because of the high probability of manifest osteoporosis.
Thresholds on the Calscan using the diagnostic WHO criteria for osteoporosis
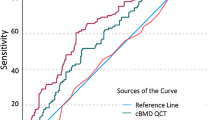
A total of 45 out of 182 patients did have a DXA T-score ≤−2.5 SD and could be classified as osteoporotic. In Fig. 3 and Table 6 one can see that with an upper threshold of −1.4 SD on the Calscan 91.1% (95% CI 78.8–97.5%) of osteoporotic patients were classified correctly by the Calscan. Using a lower threshold on the Calscan of −2.9 SD 90.5% (95% CI 84.3–94.9%) of non-osteoporotic patients were correctly classified.
Calscan T-score related to DXA T-score. Patients on the left side of the vertical line crossing the DXA-axis at −2.5 SD do have osteoporosis. Patients on the right side of this line do not suffer from osteoporosis. Tcal-normal: the Calscan T-score under which 90% of osteoporotic patients are classified correctly as osteoporotic (a). Tcal-osteoporosis: the Calscan T-score above which 90% of the patients without osteoporosis are classified correctly as non-osteoporotic (b)
When both thresholds were used 52 (29%) patients did not have to be assessed by DXA because of the low probability of osteoporosis and 34 (19%) patients did not need DXA evaluation because of the high probability of osteoporosis.
Discussion
As osteoporosis is a common health problem it has been established that diagnosing and treating osteoporosis is necessary. Therefore the need for measurement of BMD is growing. Although in most clinics DXA is the preferred method of examination in assessing BMD, this method is not available in every clinic, whereas peripheral densitometers are widely available [3]. Although DXA measurement of the hip is the best predictor for the chance of a hip fracture, previous studies showed that peripheral densitometers are equally effective in predicting the chance of an osteoporotic fracture at any site in the skeleton compared to DXA of hip and spine [11]. Therefore, a peripheral densitometer like the Calscan seems to be a worthwhile device at the FO-Clinic as the goal at a FO-Clinic is to predict fracture risk due to osteoporosis.
Nevertheless, the diagnosis of osteoporosis is based on the T-scores measured by DXA and cannot be simply applied to T-scores measured by Calscan. Although correlation between DXA and different measurement devices like the Calscan is poor and there is a lack of agreement about different devices, the NOS posed a consensus on how peripheral densitometers could be used in decision making about patient treatment based on measured BMD by peripheral densitometers [1, 3, 14]. By incorporating the revised NOS guidelines it was possible at the FO-Clinic to calculate treatment thresholds for the Calscan. Using a Tcal-osteoporosis of −2.9 SD and a Tcal-normal of −1.3 SD, 45% of the patients could be classified as manifest-osteoporotic or non-manifest-osteoporotic based on the Calscan T-score only with a sensitivity and specificity of 90%, as suggested by the NOS guidelines [14]. In our study 55% of all patients still needed DXA examination to exclude whether or not manifest osteoporosis is present. This is in close concordance with the present literature stating that around 50% of patients require DXA [1].
The above-mentioned thresholds are calculated using the definition of manifest osteoporosis to classify patients as osteoporotic or not. The definition of manifest osteoporosis was chosen because we studied a fracture population. Using the T-score ≤−2.5 SD would have led to the diagnosis severe osteoporosis according to the WHO criteria. This would have underestimated the problem of osteoporosis in our population. Nevertheless, because most studies comparing DXA to Calscan use the diagnostic WHO criteria for osteoporosis the thresholds on the Calscan and general data are also given in the “Results” using these diagnostic WHO criteria for good comparison to other studies. As can be seen in Tables 5 and 6 thresholds on the Calscan do not differ very much with either definition.
Previous studies in calculating thresholds for the Calscan are not widely available. Thorpe et al. [18] calculated a Tcal-osteoporosis of −2.7 SD and Tcal-normal of −1.4 SD. Blake et al. [1] calculated a Tcal-osteoporosis of −2.7 SD (95% CI −2.5 to −3.5) and a Tcal-normal of −1.4 SD (95% CI −0.9 to −1.6). The small differences from our calculations, a Tcal-osteoporosis of −2.9 SD and a Tcal-normal of −1.3 SD, can probably be explained by the populations studied. Both Thorpe and Blake included only postmenopausal Caucasian women between 55 and 70 years of age whereas we included all patients aged 50 years or more attending our emergency department with a low-energy fracture. Another difference is that both Thorpe and Blake used a DXA T-score ≤−2.5 SD as the definition for osteoporosis, whereas we used the definition of DXA T-score ≤−2 SD. As can be seen in Table 6 the lower threshold in our study is the same when the diagnostic WHO criteria for osteoporosis are used.
An explanation for the wide range in both thresholds might be the relatively low correlation of r = 0.47 (P < 0.0001) between the Calscan and DXA. This correlation is comparable to the correlation found in literature [1]. The low correlation might be explained by the different percentages of trabecular bone at the calcaneus, hip or spine which are 95, 40 and 66%, respectively [2, 17]. Trabecular bone is metabolically active in contrast to cortical bone and it is reasonable to expect that this leads to different measurements of BMD. A second reason for the low correlation might be the more accurate technique of measuring BMD by the Calscan. Combining DXA with laser will diminish the errors in measuring BMD, related to small non-uniform changes in soft tissue composition and thickness as well as to variable bone marrow composition [4].
A limitation of this study is that an a priori sample size calculation was not performed. Nevertheless, because we found a significant result the sample size must have been big enough. Another limitation was that the timing of performing the DXA and Calscan was random and not established in a protocol. The last limitation of this study is the relatively small group of patients studied compared to the extensive research done with DXA. Therefore it is questionable whether or not these results can be implemented in daily clinical practice. Nevertheless, because of the clinical importance of screening high risk patients for osteoporosis and the limited access to DXA we think that the Calscan is a worthwhile tool at the FO-Clinic and it should be considered to use as a screening device.
In conclusion, as stated in the literature, osteoporosis is a major health problem. To overcome this problem an active approach in case finding osteoporosis by means of a FO-Clinic is necessary. In this study we proved the Calscan to be a promising technique to use at a FO-Clinic in assessing BMD. This study suggests that if the Calscan is incorporated in the routine screening for manifest osteoporosis almost half of the sum total of patients will only need one visit to such a FO-Clinic, resulting in correct diagnosis and if necessary treatment without DXA measurement. This is time saving and patient-friendly. Nevertheless, before DXA can be really omitted more research on the Calscan needs to be done.
References
Blake GM, Chinn DJ, Steel SA, Patel R, Panayiotou E, Thorpe J et al (2005) A list of device-specific thresholds for the clinical interpretation of peripheral X-ray absorptiometry examinations. Osteoporos Int 16:2149–2156
Bonnick SL (2004) Bone densitometry in clinical practice: application and interpretation. Humana Press Inc., Totowa
Faulkner KG, von Stetten E, Miller P (1999) Discordance in patient classification using T-scores. J Clin Densitom 2:343–350. doi:10.1385/JCD:2:3:343
Hakulinen MA, Saarakkala S, Toyras J, Kroger H, Jurvelin JS (2003) Dual energy X-ray laser measurement of calcaneal bone mineral density. Phys Med Biol 48:1741–1752
Hegeman JH, Oskam J, van der Palen J, Ten Duis HJ, Vierhout PA (2004) The distal radial fracture in elderly women and the bone mineral density of the lumbar spine and hip. J Hand Surg [Br] 29:473–476
Hegeman JH, Willemsen G, van Nieuwpoort J, Kreeftenberg HG, van der Veer E, Slaets JPJ et al (2004) Effective case finding of osteoporosis in a fracture and osteoporosis clinic in Groningen; an analysis of the first 100 patients. Ned Tijdschr Geneeskd 148:2180–2185
Institute for Quality in Public Healthcare CBO (2002) Osteoporosis, Second revised guideline. Utrecht
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int 4:368–381. doi:10.1007/BF01622200
Kullenberg R (2003) Reference database for dual X-ray and laser Calscan bone densitometer. J Clin Densitom 6:367–372. doi:10.1385/JCD:6:4:367
Kullenberg R, Falch JA (2003) Prevalence of osteoporosis using bone mineral measurements at the calcaneus by dual X-ray and laser (DXL). Osteoporos Int 14:823–827
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034. doi:10.1007/s00198-003-1507-z
Nakamura T, Liu JL, Morii H, Huang QR, Zhu HM, Qu Y et al (2006) Effect of raloxifene on clinical fractures in Asian women with postmenopausal osteoporosis. J Bone Miner Metab 24:414–418. doi:10.1007/s00774-006-0702-3
National Osteoporosis Society Position Statement on the use of peripheral X-ray absorptiometry in the management of osteoporosis (2004). National Osteoporosis Society, Bath, England
Osteoporose stichting http://www.osteoporosis.nl. Accessed 20 March 2006
Placide J, Martens MG (2003) Comparing screening methods for osteoporosis. Curr Womens Health Rep 3:207–210
Salminen H, Saaf M, Ringertz H, Strender LE (2005) Bone mineral density measurement in the calcaneus with DXL: comparison with hip and spine measurements in a cross-sectional study of an elderly female population. Osteoporos Int 16:541–551
Thorpe JA, Steel SA (2006) The DXL Calscan heel densitometer: evaluation and diagnostic thresholds. Br J Radiol 79:336–341
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. 843:1–129
Acknowledgments
The authors would like to thank Mrs. I. ter Beek and Mrs. H. Kroeze, specialized trained nurses of the FO-Clinic, for their work in taking care of all patients ≥50 year, admitted to our emergency department with a low-energy fracture to be invited to the FO-Clinic and arranging all necessary examinations. Research funds for acquiring the Calscan: Sanofi-Aventis, Merck Sharp & Dohme, Procter&Gamble, Nycomed, Roche.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Klerk, G., van der Velde, D., van der Palen, J. et al. The usefulness of dual energy X-ray and laser absorptiometry of the calcaneus versus dual energy X-ray absorptiometry of hip and spine in diagnosing manifest osteoporosis. Arch Orthop Trauma Surg 129, 251–257 (2009). https://doi.org/10.1007/s00402-008-0755-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-008-0755-y