Abstract
Background
The combination of the reconstruction of the coracoclavicular ligaments with the resection arthroplasty of the distal end of the clavicle is a commonly used technique in acromioclavicular separations.
Hypothesis
The purpose of the current study was to quantify the reduction parameters using 3-D CT and to analyze their effects on clinical outcomes.
Study design
Case series.
Methods
The patients with chronic symptoms after acromioclavicular dislocation (type III) were treated with reconstruction of the coracoclavicular ligaments. The average follow-up was 69.5 months. The patient group consisted of 21 men and 8 women. The initial treatment at the time of injury was nonoperative in 26 of 29 patients. CT was used to document anteroposterior (APD), craniocaudal (CCD) and mediolateral (MLD) acromioclavicular reduction parameters. Constant Shoulder scoring system was used.
Results
The mean preoperative Constant score was 56.62 ± 18.63 points while the postoperative score was 89.93 ± 10.79 points. The mean APD was 9.2 mm, the mean CCD was 1.1 mm and the mean MLD was 8.4 mm. There was no correlation between the APD, MLD and the Constant Scores. However, an inverse correlation between the CCD and the postoperative Constant Scores was found.
Conclusions
CCD plays an important role on the postoperative function. If the CCD is larger, the Constant score is lower.
Clinical relevance
The reduction loss is a distinctive parameter of the functional outcome, even when the reconstructed coracoclavicular ligament is intact. Secure fixation may be achieved with techniques preserving CCD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The classification system devised by Allman and Tossy, and revised by Rockwood, defines the extent of injury to the acromioclavicular (AC) joint and helps to guide management of AC joint injuries. Although AC joint separations are fairly common, the occurrence of high grade separations that require surgery is low. Type I and II injuries may be treated nonoperatively with a sling for a short period of time. Treatment of type III injuries is controversial, but nonoperative management of the acute injury is most currently preferred. Type IV–VI injuries should be operatively reduced and stabilized [5]. Arthritis due to the dislocated AC joint and instability associated with the disruption of the coracoclavicular ligaments result in symptoms of chronic aching and shoulder weakness. Therefore, there is a need for treatment of patients with symptomatic chronic complete dislocations of the AC joint [1, 6, 21].
The combination of the surgical reconstruction of the coracoclavicular ligaments with the resection arthroplasty of the distal end of the clavicle is the most commonly used surgical technique. Although the goal of the surgery was to restore stability between the clavicle and the scapula, the possible relation between reduction loss and the clinical outcome has not been previously evaluated. However, with the suspicion of reduction loss as a cause of poor clinical outcome, different fixation methods were used in maintaining reduction of the clavicle to an anatomic position in relation with the coracoid in both the vertical and horizontal planes [23, 33]. In this study, 29 patients with chronic complete acromioclavicular dislocation were treated with the Weaver–Dunn procedure between the years 1989–2001. The purpose of the current study was to quantify the reduction parameters using 3-D CT and to analyze their effects on clinical outcomes.
Patients and methods
Thirty-three patients with chronic symptoms more than 2 months after injury, secondary to complete acromioclavicular dislocation were treated in our clinic with reconstruction of the coracoclavicular ligaments. This was accomplished by securing the clavicle to the coracoid with Ethibond (Ethicon Products, Johnson & Johnson Company, Westwood, MA) passed around the base of the coracoid and the medial clavicular segment, and substituting the coracoacromial ligament for the coracoclavicular ligaments. Four patients were lost to follow-up and 29 patients were observed for at least 2 years, with an average follow-up of 69.48 ± 35.41 months (range, 25–143 months). The patient group consisted of 21 men and 8 women. The average age was 29.83 ± 8.31 years (range, 19–47 years). The dominant shoulder was involved in all but nine patients. The interval from injury to reconstruction averaged 25.59 ± 15.71 months (range, 2–63 months). This interval was 21.44 ± 12.23 for satisfied patients and 51.50 ± 8.35 for unsatisfied cases. All patients had radiographs that showed a complete acromioclavicular dislocation.
All patients included in this study were type III acromioclavicular dislocation according to Rockwood classification. The initial treatment at the time of injury was nonoperative in 27 of 29 patients [6]. Two patients had percutaneous pin fixation of the acromioclavicular joint. All patients reported chronic pain, deformity, and exertion weakness that interfered with activity. At the time of initial evaluation, active motion of the shoulder was limited in all patients secondary to pain and discomfort.
Initial evaluation included anteroposterior (AP), axillary and lateral radiographs of the involved shoulder and bilateral standard stress radiographs of the acromioclavicular joints. The patients were evaluated at the first, second, and third months while being followed up regularly every 6 months after surgery. AP radiographs were obtained to assess the acromioclavicular joint position after reconstruction. Stress radiographs of both shoulders were obtained to assess maintenance of reduction. Computerized tomography was used to document anteroposterior, craniocaudal and mediolateral acromioclavicular reduction parameters. For the evaluation of functional status Constant Shoulder scoring system was used [8]. None of the patients had glenohumeral arthritis, associated instability, impingement or rotator cuff insufficiency on initial or follow-up radiographs.
Operative technique
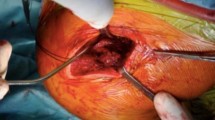
A 7-cm incision began 2 cm posterior to the clavicle and crossed the clavicle 2 cm medial to the acromioclavicular joint in Langer’s lines. The distal 1 cm of the clavicle was resected, and the medullar canal was opened by a curette. The coracoacromial ligament was identified and detached from the anterior and inferior surface of the acromion. If the ligament appeared to be of insufficient length, anterior attachment of the ligament could be released from the coracoid process. 1-mm cotton Dacron tape suture (Deknatel, Coventry, CT) was woven through and out of the detached end of the ligament after which the tape was passed through drill holes on the clavicle. A number 2 Ethibond suture was passed around the base of the coracoid while the medial clavicular segment was used to stabilize the clavicle in its reduced position in relation to the coracoid process as well as to protect the transferred coracoacromial ligament from stretching or rupture. The sutures were tied over the top of the cortical bone.
Postoperative management
After surgery, the patient’s arm was supported in a sling. Gentle exercises with limited ranges of motion were begun the day after surgery. After 3 weeks, patients used their arm for ordinary activities. They raised their arm within the limits of discomfort and were told to avoid any strenuous pushing, pulling or lifting activities until the third month. Radiographs obtained to determine the clinical appearance of clavicle indicates loss of reduction, or patient had sudden increase in symptoms of pain or discomfort. After the third month, a stretching program was initiated and when full range of motion was achieved, the patient was instructed in a series of progressive, resistive strengthening exercises for stabilization of the rotator cuff, deltoid, and scapular muscles.
Patients were evaluated at their latest follow-up by a surgeon who was not involved in patient care. Overall patient satisfaction was based on individual willingness to have the procedure again.
The primary goal of the surgery was to restore stability between the clavicle and the scapula while maintaining reduction. During the last follow-up, stress radiographs of both acromioclavicular joints and computerized tomography of the operated joints were obtained [28].
On evaluating the stress radiographs, the joint was graded as reduced, subluxed and dislocated. The joint was classified as subluxed if the clavicle was subluxed 3 mm or more in AP stress radiographs. Instability has been determined in the dislocated joint on the stress radiographs [28].
The measurements were made from 3-D models of the bony structures obtained from standardized CT examinations as the patient was laying supine, elbow in extension, and the arm attached to the body in adduction with stress. The CT scans were obtained on a Hi-Speed CT/I scanner (GE Medical Systems, Milwaukee) and 120 kV, 350 mA, 1-mm slice thickness, zero inter-slice gap, 512 × 512-matrix and bone algorithm scan parameters were used. The axial scans were parallel to the acromioclavicular joint. The image data were transferred to a GE Advantage Windows version 2.0 workstation (GE Medical Systems). Direct axial images transferred to GE Advantage Windows were used to make 3-D models of the bony structures. This enabled us to take full advantage of the 3-D analysis in every plane for desired measurements. The detailed spatial relationships between the bony structures were carefully identified, and the anteroposterior acromioclavicular distance (APD), the craniocaudal acromioclavicular distance (CCD), and the mediolateral acromioclavicular distance (MLD) was measured. APD is the distance between the anterior margin of the acromion medial border and the anterior margin of the clavicle lateral border in the transverse plane, and was measured on the craniocaudal view (Fig. 1 a–b). CCD is the distance between the superior margin of the acromion and superior margin of the clavicle in the sagittal plane, and was measured on the sagittal view (Fig. 2 a–b). MLD is the smallest distance from the lateral border of the clavicle to the medial border of the acromion in the coronal plane, and was measured on the anteroposterior view (Fig. 3 a–b) [38]. The measurements were done by digital calipers.
Statistical analysis of the data was conducted with the SPSS software (version 12.0; SPSS, Chicago, IL). Mann–Whitney U test was performed to determine whether there was a significant association between variables of satisfied and unsatisfied patients. The Spearmen correlation coefficient (r) was used to evaluate the relationship between variables. A P value of < 0.05 was considered to be significant.
Results
The mean preoperative Constant score was 56.62 ± 18.63 points (range, 22–77) while the postoperative score was 89.93 ± 10.79 points (range: 63–100). A significant difference was observed between the preoperative and postoperative Constant scores. (P < 0.0001).
The stress radiographs of both shoulders revealed the maintenance of the clavicle reduction to be rated at 89.7%. Twenty-six of the 29 patients maintained normal interval between the coracoid and the clavicle. Three patients had the clavicle in a slightly superior subluxed position.
All patients were capable of doing overhead activities. The preoperative daily activity score was 11.4 points (range, 4–16) and found to be improved to 17.7 points (range, 14–20) at the latest follow-up (P < 0.0001).
The mean preoperative strength score was 17.58 points (range, 10–25) which increased to 22.58 points (range, 15–25). Normal strength was achieved in 21 of 29 patients at the latest follow-up. Although four patients had symptoms of discomfort, all patients were able to return to their previous level of activity and employment.
The mean preoperative pain score was 6 points. The mean amount of pain at the last follow-up visit was 13.6 points (range, 10–15). 21 patients had no pain at follow-up, whereas 4 had mild pain with strenuous activity. The remaining 4 patients were unsatisfactory with regard to pain.
The mean APD was 9.24 ± 1.06 mm (range, 8–11), the mean CCD was 1.10 ± 0.86 mm (range, 0–3) and the mean MLD was 8.38 ± 0.98 mm (range, 7–10) (Table 1). When the Total Constant Score and its parameters were evaluated, the difference was found to be statistically significant between the preoperative and the postoperative scores (P < 0.0001). There was no correlation between the APD, MLD and the Constant Scores. However, an inverse correlation between the CCD and the postoperative Constant Scores was found (r , −0.64; P < 0.0001). That means as CCD decreases, postoperative Constant score increases. On the other hand, there is positive correlation between preoperative interval and CCD which means as interval from injury to operation increases the reduction becomes more difficult (r, 0.54; P, 0.003).
Twenty-five of the 29 (87%) patients stated that they would have the surgery again, while 4 patients stated that they would not have surgery if they had been under the same situation. An increased CCD was found in those 4 unsatisfied patients. There was no significant difference between APD and MLD when compared to the satisfied patients. The mean preoperative Constant Score of the unsatisfied patients was 30.75 ± 7.80 points (range, 22–41), and the postoperative score was 71.25 ± 6.18 points (range, 63–76).
None of the patients had coracoclavicular subluxation clinically. Two patients had draining fistulas over the clavicle which healed with appropriate antibiotic treatment (cephalexin 1g/bid). There were no neural or vascular complications.
Discussion
Type III injuries of coracoclavicular ligaments have stirred the most controversial debate regarding treatment options, with numerous proponents of both closed and open surgical methods [2, 3, 17, 27]. Jacobs and Wade [18] believed that the long-term result depended more on the nature of the damage to the joint than on the form of the treatment. However, they also believed that a retained damaged articular disc would influence the outcome and recommended surgery for complete injuries. Therefore, the surgical procedure is successful in most patients but fair or poor results were also reported in up to 20% of the patients in different series [2, 8, 12]. Glick et al. believed that incomplete rehabilitation was the main reason for weakness and pain after complete AC dislocation. They concluded that complete reduction of the AC joint is not necessary for satisfactory function. However, subjective evaluation in the study by Walsh et al. indicated that Grade III dislocations treated conservatively had more pain and stiffness despite substantial strength [5, 12, 16, 36]. It is still not clear which treatment option will be the best solution. It is important to remember that a patient with poor anatomical result may have no symptoms, whereas anatomical restoration of the joint does not always relieve symptoms [2, 22].
Although, the primary goal of the surgery was to restore stability between the clavicle and the scapula, the possible relationship between reduction loss and the clinical outcome has not been previously evaluated. However, with the suspicion of reduction loss as a cause of poor clinical outcome, different fixation methods such as screws, suture, hook-plate wire or tape were used in maintaining reduction of the clavicle to an anatomic position in relation with the coracoid in both the vertical and horizontal planes [8, 14, 19, 20, 35]. In a review about the treatment of Grade III acromioclavicular joint injuries, it was emphasized there was no correlation between radiographic appearance and the clinical outcome; and also concluded that nonoperative treatment is superior to operative [32]. On the other hand, Gstettner et al. [14] found significantly better results in the operated group. The postoperative Constant shoulder score findings (89.93 ± 10.79) of current study are very similar to Gstettner et al’s (90.4 ± 12.9). Contrary to the review [32], our study showed a significant correlation between radiographic finding (CCD) and clinical outcome.
Weaver and Dunn described an operative technique that combined stabilization of the clavicle by means of the coracoacromial ligament with resection arthroplasty of the acromioclavicular joint [37]. Despite reports of excellent results with the Weaver–Dunn coracoacromial ligament transfer, some authors recommend augmenting the transfer with supplemental fixation. Deshmukh et al. did biomechanical testing of various surgical techniques in a cadaver model. According to this study, when performing acromioclavicular reconstruction, supplemental fixation should be used to provide more stability and pullout strength than the Weaver–Dunn reconstruction alone [10, 33]. Since patients had good clinical results in most series, the capability of the Weaver–Dunn technique in restoration of joint reduction in three planes was not tested. The advantage of CT in comparison to standard X-ray is the ability to measure in three planes. This was the first study in which reduction parameters were quantified by 3-D CT and their effects on clinical outcomes were analyzed. The original aspect was quantification of the CCD and analysis of its effect on functional shoulder scores. A drawback of CT scan is the difficulty of evaluation of acromioclavicular joint under stress. Although position during CT examinations were standardized as patients were laying supine, elbow in extension and arm attached to the body in adduction, there was no weight at their arms which probably influenced the values of AC joint reduction parameters. A method, enabling stress CT scan by application of weight traction on arms, will provide more accurate and reliable measurement of parameters for the evaluation of reduction.
According to our findings, CCD plays an important role on the postoperative function. When CCD increases, the postoperative function becomes worse. All unsatisfactory results in this study had at least 3 mm of CCD. During the surgery, the distance should be preserved and reconstructed anatomically. The reduction loss should not exceed 2 mm for good results. Therefore, it can be said that if the increase of CCD is larger than 2 mm, the postoperative functional status of the patients may be lower. If the CCD is larger, the Constant score is lower.
The limited number of patients can be seen as a shortcoming of the present study. Only 4 of 29 patients had unsatisfactory results. The explanation for their dissatisfaction could be that the scores they started with was their lowest and did not improve as much as they thought it would. Another and probably more accurate explanation, Rolf et al. [29] point out in their study that early reconstruction of acromioclavicular joint avoids the inferior clinical results of delayed reconstructions. These unsatisfied patients were the most delayed cases of the current study. In present study, we also found that reduction and clinical outcome are better in early operated cases. Because of the small patient series, the measurements were done mostly in patients with good results. It is a point of question of how the CCD changes in patients with bad results in larger series. Due to the limited number of patients, we are unable to correlate treatment with patient demands, e.g., the throwing athlete. The other shortcoming is that, we do not know the normal variances of the CCD without any pathology and also there is no reference data in literature. The patients may have wider CCD because of anatomical variances and the measured values of patients of the present study might be their normal parameters or were not alone influenced from the surgery. Measurements of parameters, especially CCD levels, of normal population and AC dislocated individuals preoperatively would probably provide better evaluation and comparison of the reduction.
The Weaver–Dunn technique is a popular technique for the treatment of type III injuries and thus, we prefer this technique in our clinic [37]. More secure fixation may be obtained with other methods such as screw, wire, hook plate, or tape in maintaining reduction. This study is limited by the fact that only one operative procedure was examined. Some authors prefer screw fixation to other methods such as suture, wire and hook plate or tape, because the screw is more reliable in maintaining reduction in the vertical and horizontal planes [11, 15]. Although it seems to be a more secure fixation, it is technically demanding with a need for wide exposure and added difficulty in controlling the screw. Also, loosening of the Bosworth coracoclavicular screw was reported [26]. When the K wire/tension band wiring method was used, the technique was limited due to removal of the wire, a much more extensive dissection was needed, usually requiring general anesthesia. Also, complications such as migration of the K wires to the lungs had been reported [24]. However, some authors propose that augmented Weaver–Dunn reconstruction yields more functional and less painful joint [10, 39]. Besides augmentation, coracoclavicular reconstruction using autogenous tendon grafts like semitendinosus and gracilis even arthroscopically assisted techniques achieved good to excellent results [9, 31, 34].
It is a question that the slight residual deformity should make a big difference in shoulder girdle function, particularly when the distal clavicle has been resected [13, 25, 30]. The patients who requested the surgery were very demanding and if they were unhappy with the cosmetic or radiographic appearance, they were unhappy overall and perceived themselves as less well. We should be aware that every slight deformity does not lead to shoulder dysfunction. This is unlikely based upon observations of good shoulder girdle function after complex trauma with residual deformity in a substantial number of patients.
Even though this study seems to be a radiological study, it has very significant clinical results. Radiographs including anteroposterior, lateral, axillary and Zanca views were used and also advised to be obtained for evaluation of clinical and radiological outcomes in many studies [4, 7, 14, 29, 31, 34, 39]. Except stress graph, CT scan is a better way of assessment of instability as it can determine instability parameters in three planes easily and more accurately. However, the present study finds out that the success of the operation is only affected from the craniocaudal instability. That means standard anteroposterior X-ray is good and very valuable modality in evaluation and diagnosis of instability. These objective findings support the idea that reduction loss is a cause of functional outcome decrease. More secure fixation may be achieved with techniques preserving CCD. Therefore, results of the current study may bring new sound for evaluation and development of new repair and reconstruction techniques. Supplemental fixation methods should be tested to provide more stability and pullout strength than the Weaver–Dunn reconstruction alone.
References
Adam FF, Farouk O (2004) Surgical treatment of chronic complete acromioclavicular dislocation. Int Orthop 28(2):119–122. doi:10.1007/s00264-003-0520-3
Allman FL Jr (1967) Fractures and ligamentous injuries of the clavicle and its articulations. J Bone Joint Surg 49A:774
Bailey RW, Metten CF, O’Connor GA et al (1975) A dynamic method of repair for acute and chronic acromioclavicular disruption. Am J Sports Med 4:58. doi:10.1177/036354657600400203
Bishop JY, Kaeding C (2006) Treatment of the acute traumatic acromioclavicular separation. Sports Med Arthrosc Rev 14(4):237–245. doi:10.1097/01.jsa.0000212330.32969.6e
Bjerneld LH et al (1983) Acromioclavicular separations treated conservatively. Acta Orthop Scand 54:743
Bradley JP, Elkousy H (2003) Decision making: operative versus nonoperative treatment of acromioclavicular joint injuries. Clin Sports Med 22(2):277–290. doi:10.1016/S0278-5919(02)00098-4
Calvo E, Lopez-Franco M, Arribas IM (2006) Clinical and radiologic outcomes of surgical and conservative treatment of type III acromioclavicular joint injury. J Shoulder Elbow Surg 15(3):300–305. doi:10.1016/j.jse.2005.10.006
Constant CR, Murley AHG (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Costic RS, Labriola JE, Rodosky MW, Debski RE (2004) Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med 32:1929–1936. doi:10.1177/0363546504264637
Deshmukh AV, Wilson DR, Zilberfarb JL et al (2004) Stability of acromioclavicular joint reconstruction: biomechanical testing of various surgical techniques in a cadaveric model. Am J Sports Med 32(6):1492–1498. doi:10.1177/0363546504263699
Faraj AA, Ketzer B (2001) The use of a hook-plate in the management of acromioclavicular injuries: report of ten cases. Acta Orthop Belg 67(5):448–451
Glick JM, Milburn LJ, Haggerty JT et al (1977) Dislocated acromioclavicular joint: follow-up with study of 35 unreduced acromioclavicular dislocations. Am J Sports Med 5:264. doi:10.1177/036354657700500614
Grutter PW, Petersen SA (2005) Anatomical acromioclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med 33(11):1723–1728. doi:10.1177/0363546505275646
Gstettner C, Tauber M, Hitzl W, Resch H (2008) Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg, Epub ahead of print
Guy DK, Wirth MA, Griffin JL (1998) Reconstruction of chronic and complete dislocations of the acromioclavicular joint. Clin Orthop Relat Res 347:138–149. doi:10.1097/00003086-199802000-00017
Horn JS (1954) The traumatic anatomy and treatment of acute acromioclavicular dislocation. J Bone Joint Surg Br 36-B:194–201
Imatani RJ, Hanlon J, Cody GW (1975) Acute complete acromioclavicular separation. J Bone Joint Surg 57A:328
Jacobs B, Wade PA (1966) Acromioclavicular joint injury. J Bone Joint Surg 48A:475
Jari R, Costic RS, Rodosky MW, Debski RE (2004) Biomechanical function of surgical procedures for acromioclavicular joint dislocations. Arthroscopy 20(3):237–245. doi:10.1016/j.arthro.2004.01.011
Jerosch J, Filler T, Peuker E (1999) Which stabilization technique corrects anatomy best in patients with AC separation? An experimental study. European Society for Shoulder and Elbow Meeting SECEC/ESSSE, The Netherlands, Hague
Klonz A, Loitz D (2005) The acromioclavicular joint. Unfallchirurg 108(12):1049–1060. doi:10.1007/s00113-005-1034-9
Lancaster S, Horowitz M, Alonso J (1987) Complete acromioclavicular separations: a comparison of operative methods. Clin Orthop Relat Res Mar(216):80–88
Laprade RF, Hilger B (2005) Coracoclavicular ligament reconstruction using a semitendinosus graft for failed acromioclavicular separation surgery. Arthroscopy 21(10):1277. doi:10.1016/j.arthro.2005.07.020
Mazet RJ (1943) Migration of a Kirschner wire from the shoulder region to the lung. J Bone Joint Surg 48A:477
Mazzocca AD, Santangelo SA, Johnson ST et al (2006) A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med 34(2):236–246. doi:10.1177/0363546505281795
Pavlik A, Csepai D, Hidas P (2001) Surgical treatment of chronic acromioclavicular joint dislocation by modified Weaver–Dunn procedure. Knee Surg Sports Traumatol Arthrosc 9(5):307–312. doi:10.1007/s001670100222
Pettrone FA, Nirschl RP (1978) Acromioclavicular dislocation. Am J Sports Med 6:160. doi:10.1177/036354657800600403
Rockwood CA (2001) Injures to the acromioclavicular joint. In: Rockwood CA, Green DP (eds) Fractures in adults. 5th edn. Lippincott Williams & Wilkins, Philadelphia, vol 2, pp 1220–1221
Rolf O, Hann von Weyhern A, Ewers A, Boehm TD, Gohlke F (2008) Acromioclavicular dislocation Rockwood III–V: results of early versus delayed surgical treatment. Arch Orthop Trauma Surg, Epub ahead of print
Sahara W, Sugamoto K, Murai M et al (2006) 3D kinematic analysis of the acromioclavicular joint during arm abduction using vertically open MRI. J Orthop Res 24(9):1823–1831
Scheibel M, Ifesanya A, Pauly S, Haas NP (2008) Arthroscopically assisted coracoclavicular ligament reconstruction for chronic acromioclavicular joint instability. Arch Orthop Trauma Surg, Epub ahead of print
Spencer EE Jr (2007) Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res 455:38–44. doi:10.1097/BLO.0b013e318030df83
Su EP, Vargas JH 3rd, Boynton MD (2004) Using suture anchors for coracoclavicular fixation in treatment of complete acromioclavicular separation. Am J Orthop 33(5):256–257
Tauber M, Eppel M, Resch H (2008) Acromioclavicular reconstruction using autogenous semitendinosus tendon graft: results of revision surgery in chronic cases. J Shoulder Elbow Surg, Epub ahead of print
Tossy JD, Mead NC, Sigmond HM (1963) Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res 28:111–119
Walsh MW, Peterson DA, Shelton G, Neumann R (1985) Shoulder strength following acromioclavicular injury. Am J Sports Med 13:152. doi:10.1177/036354658501300302
Weaver JK, Dunn HK (1972) Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg 54A:1187–1194
Wickiewicz TL (1983) Acromioclavicular and sternoclavicular joint injuries. Clin Sports Med 2(2):429–438
Wilson DR, Moses JM, Zilber farb JL, Hayes WC (2005) Mechanics of coracoacromial transfer augmentation for acromioclavicular joint injuries. J Biomech 38(3):615–619. doi:10.1016/j.jbiomech.2004.04.015
Conflict of interest statement
No financial support or personal relation by any of authors has been received which could inappropriately influence the outcome of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bezer, M., Saygi, B., Aydin, N. et al. Quantification of acromioclavicular reduction parameters after the Weaver–Dunn procedure. Arch Orthop Trauma Surg 129, 1017–1024 (2009). https://doi.org/10.1007/s00402-008-0723-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-008-0723-6