Abstract
Introduction
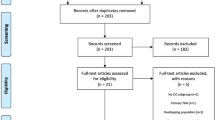
The number of revision hip arthroplasties is increasing but several aspects of this procedure could be improved. One method of reducing intra-operative complications is the cement-in-cement technique. This procedure entails cementing a smaller femoral prosthesis into the existing stable cement mantle. The aim of this systematic review is to provide a concise overview of the existing historical, operative, biomechanical and clinical literature on the cement-in-cement construct.
Results
Four biomechanical publications exist in authoritative journals and these were reviewed. Simple specimens were produced and these were tested by static means. Although these published tests support the cement-in-cement technique, they cannot be regarded as conclusive. Areas which could be subject to further research are identified. Five clinical publications on patients undergoing cement-in-cement revisions were also reviewed. Patient numbers were generally low (7–53) apart from one study containing 354 patients. Long-term patient follow-up was not available except in Hubble’s study (41 patients followed for 8 years). Outcomes of these patients were very satisfactory for the period of follow-up. Three expert reviews of cemented femoral revisions outline the cement in cement procedure. If other Orthopaedic Centres can emulate the results of the clinical research presented, complication rates, operative times and financial costs may be decreased.
Conclusion
The analysis presented in this paper consolidates the latest biomechanical and clinical information on cement-in-cement revision hip arthroplasty. Although we find evidence to support the use of the method clinically, we do note that the scientific basis needs further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of revision hip replacements will increase in line with the rise in number of primary hip replacements due to ageing of our population. The number of revision hip arthroplasties in the US is estimated to rise by 137% in the next 25 years [15]. Similar trends are seen in other countries [12]. Fourteen percentage of total hip arthroplasties were revision hip procedures in public hospitals in Ireland in 2005 [6].
The removal of the cement mantle in the revision of cemented femoral implants causes considerable surgical difficulty. It can lead to numerous significant complications. These include substantial bleeding, perforation of the femoral cortex or even fracture of the femur [20]. Loss of bone stock can occur from mechanical removal [2] or damage to the bone that remains from the rasping procedure [8]. Removal of the cement mantle is also time consuming; it can lengthen the procedure by 2 h or more [13, 23]. This has both medical and financial implications; prolonged anesthetic times can lead to increased medical complications and morbidity both intra-operatively and post-operatively and the increased theatre time required is also costly. This further increases the expenditure of an already costly endeavor.
Many different methods exist for the removal of the cement mantle, suggesting that there is no completely satisfactory procedure [2]. Thus, it is clinically important to develop ways to improve or avoid this difficult and hazardous step of the revision and thereby enhance the clinical outcomes of patients undergoing revision surgery. The cement-in-cement revision hip arthroplasty completely avoids removal of the cement mantle and thus the above complications.
The procedure is started in a similar way to other revision techniques. The surgical incision is made through the scar of the previous operation. A standard approach (e.g., posterior) is utilized to expose the femoral component [2]. (A radiograph of a femoral component that was revised by cement-in-cement revision is shown in Fig. 1a.) The proximal cement above the shoulder of the prosthesis is cleared prior to attempts at stem removal [23]. Following this the prosthesis is “tapped out” [21]. This allows direct intra-operative inspection of the cement mantle (Fig. 1b). The proximal cement is removed using a burr if it is cracked or if there is a concern over the cement bone bond at this level. The cement is cleared to a depth were osseointegration of the cement–bone interface can be confirmed [23]. If any crack in the cement is visible beyond the initial 2 cm of mantle (or beyond the lesser trochanter) all the cement is removed and an alternate revision procedure is performed [21]. Some advocate preparation of the inner surface of the cement mantle with a rasp, burr or ultrasonic device [7, 17–19], whereas others do not. The cement mantle is thoroughly cleaned using pulsed lavage [23]. It is carefully dried. A double mix of cement is prepared in a vacuum-mixed bowl and, while still in a low state of viscosity, is inserted into the femur using a cement insertion gun with a thin nozzle (Stryker Howmedica Osteonics, Limerick, Ireland). This early introduction of fresh cement is endorsed by Lieberman, as it is thought to promote integration between the new and old cement. Suction and compression techniques are employed to ensure that maximal cement pressurization is achieved [23]. Following this, the new femoral component is inserted. A radiograph of this is shown in Fig. 1c.
Series of images of a patient who underwent a cement-in-cement revision. a This pre-operative radiograph shows a cemented total hip replacement. The acetabular component was loose and caused significant pain to the patient. b This operative photograph shows an intact femoral cement mantle after the femoral stem had been removed. c Post-operative radiograph showing the Exeter stem that was used [procedure performed by the Senior Clinical Author (P.J.K.)]
Greenwald et al. [10] undertook a biomechanical experiment investigating the bonding of “old and new polymerized acrylic bone cements”. The first full operative description of cement-in-cement revision is available in the book “Principles of total hip arthroplasty” [7]. There have been other publications over the years which are discussed later. In the last 2 years, there has been renewed interest in the technique. Three publications were published in this time in both the biomechanical and clinical aspects of this procedure. The aim of this paper is to provide a concise overview of the existing historical, operative, biomechanical and clinical literature on the cement within cement construct. The clinical outcomes of the patients who have undergone this procedure will be evaluated. Furthermore the results of the biomechanical research will be assessed to determine if there is scientific evidence to support this technique.
The cement-in-cement operative procedure
In the early 1970s, Smith Petersen (verbal communication reported in Nabors et al.) suggested a method for obtaining exposure to the acetabulum that involves removing the well-fixed femoral component from its intact cement mantle. The same stem was reinserted at the conclusion of the acetabular reconstruction [21]. Around this time also, Professor Sir John Charnley was employing this technique in revision of non-infected femoral prostheses. Greenwald et al. [10] possibly came up with the idea of cement within cement revision from this “tap out–tap in” method. They report the earliest description of bonding “old and newly polymerized acrylic bone cements” in a published abstract from the 61st Clinical Congress of the American College of Surgeons (ACS) in 1975. In the first operative description, Eftekhar [7] described “rechannelization of the femur” where in a revision procedure the old prosthesis was removed but the cement mantle was left in situ. The inner surface of the old cement was reamed, irrigated and carefully dried. Thereafter fresh bone cement was inserted and a new prosthesis was implanted.
Indications to perform cement-in-cement revisions and its current usage
The cement-in-cement revision can be undertaken in a number of common revision situations. It provides exposure for visualization and access of instrumentation for revision of an acetabular component (Fig. 1) [13, 17, 23]. It can be used to replace a broken component with an intact distal mantle [13, 23] or in the exchange of a mono-block stem with damage to the head. It can be used in the correction of a mal-positioned component for recurrent dislocation [17] or leg length discrepancy or even to convert a well-fixed cemented hemiarthroplasty to a total hip arthroplasty [13, 23]. It is not in widespread use worldwide.
The advantages of the cement-in-cement technique
It is a simpler technique and is less time consuming [13, 23]. The arduous task and complications of removal of the entire cement mantle are avoided. For acetabular revisions, the removal of the femoral component allows excellent exposure to the acetabulum [13, 21]. Due to this reduction in operative and anesthetic time, it may go on to decrease peri-operative morbidity and mortality. Further advantages are that there is preservation of bone stock [13] and reduced blood loss with no apparent detrimental effect on femoral component fixation [11, 24]. Costs are reduced due to decreased theatre time. This method also allows earlier post-operative full weight bearing mobilization for the patient [13].
Disadvantages of cement-in-cement revision
The cement-in-cement construct could undergo early failure if the original cement mantle is compromised. It is therefore essential to determine the suitability of this cement radiologically and intra-operatively. Correct alignment of the new prosthesis may be difficult [23]. The new implant may adapt the version or offset of the old prosthesis and that may have been incorrect in the first instance. However, to prevent this, the existing mantle can be modified by using a rasp, burr, or ultrasonic device to trim the cement in the areas of concern. This should be undertaken without the disruption of the existing cement–bone interface.
The cement–cement interface may become contaminated by blood and marrow fat, despite modern lavage techniques. This may act as a stress riser, facilitating the formation of fatigue cracks in the cement.
Requirements and contraindications of this operation
An intact femoral cement mantle is essential for this type of revision procedure [17, 23]. This may be assessed pre-operatively using radiography, and intra-operatively by inspection as described previously. Collarless, polished, straight or slightly curved tapered stems lend themselves to this technique, as they can be easily knocked out of their cement mantle, without imparting damage to the mantle.
Radiolucencies at the bone cement interface in neither Gruen zone 1 nor 7 are contraindications [18, 23]. A radiolucency between the cement and the prosthesis proximally is also not a contraindication. However, stems that have a matted finish or which are precoated are not ideal as they may be difficult to remove [21].
Biomechanical aspects of the cement-in-cement technique
A total of four biomechanical studies have been published on the cement-in-cement construct. These are listed in Table 1 along with some of their features. The objective of these studies was to assess the strength of the interface of the fresh and pre-polymerized cements under a variety of different conditions. These conditions included the effect on the interface of using cement mixed for varying times before insertion [11], the effect of post-cure duration [27], the effect of rasping the surface of the pre-polymerized cement [11, 16], the effect of antibiotic impregnated cement [27] and the effect of contamination at the interface [11, 16, 24].
Greenwald et al. found that introducing the new cement earlier rather than after a delay of up to 8 min strengthened the bond between the new and old cement. Rasping the surface of the old cement also improved its strength. Contamination of the interface weakened the bond.
Rosenstein’s study used 15 mm high fragments of femur. It compared the strength of the bone–cement interface of constructs of the traditional cemented revisions to constructs of the cement within cement revisions. These were assessed using the push out technique. His study concluded that the cement within cement technique maintained a stronger bone–cement interface. This was whilst maintaining a bond between the inner and outer cement mantles.
Li et al. evaluated the effect of contamination on the strength of the cement–cement interface. This study used blood and marrow from patients who had hip arthroplasties to contaminate the interface. They concluded that it was not possible to eliminate contamination from the interface and that this weakened the strength of the cement bond. Li et al. tested the interfaces that they created in two ways, by shear and tensile experiments. These are static testing modalities. They also undertook photomicrography on some of their interfaces to analyze the interfaces that they produced.
In a well-designed and detailed study, Weinrauch et al. tested the shear strength (a static test) of 5 mm thick specimens of the cement–cement interface. Through analysis of the interfacial cement region, they have been able to advance the understanding of the possible chemical reaction that takes place between the old cement mantle and the “fresh” cement. They have hypothesized that diffusion of cement monomer from the fresh cement into the old cement could lead to formation of polymer chains across the interfacial region. This research supported the cement within cement construct.
Whilst all studies used appropriate research methods, a number of aspects may be criticized. These include the lack of a realistic three-dimensional model and, perhaps more importantly, the lack of testing under cyclic loading. Therefore, although published tests support the cement-in-cement technique, they cannot be regarded as conclusive.
Review of clinical publications on cement-in-cement revisions
Four case series, one case report and three expert reviews describe patients undergoing this type of surgery. The details of the case series are included in Table 2. Whilst the majority of these clinical studies contained small patient numbers, Hubble et al. studied 354 patients. Long-term patient follow-up was not available except in Hubble’s study (41 patients followed for 8 years). Completeness of follow-up was excellent with only one patient for all the studies being lost to review. Outcome measurement was established using well-recognized and validated scoring systems. The outcome of the vast majority of the patients at an early to mid-term stage of their revision procedure was deemed very satisfactory. Only 1 patient of a total of 432 patients from all four studies needed revision of the femoral component within the period of the follow-up [19]. This revision was undertaken for recurrent dislocation and not for failure of the cement–cement construct. Therefore the clinical data so far available supports the cement-in-cement technique.
The case report cautions the use of Corin Taper-Fit Congenital Dysplasia of the Hip (CDH) stems with the cement-in-cement technique [1]. This is due to the fact that two patients suffered fracture of the stems. This occurred at 9 and 15 months, respectively, following low-demand activity.
Three expert reviews include the cement within cement procedure in their discussions [3, 17, 22]. These experts briefly outline some indications of the technique and some points on the operative steps.
Discussion
Three of the four biomechanical publications concluded in support of the cement within cement construct. Most of the biomechanical studies reviewed, however, do not reproduce the in vivo cement-in-cement construct nor do they represent current operative techniques (Table 2). Greenwald [11] and Li et al. [16] tested specimens that contained a two-dimensional cement–cement interface whereas the cement-in-cement technique forms a complex three-dimensional annular cement–cement interface (Fig. 2). Whilst testing of a two-dimensional interface gives an indicator of the strength and characteristics of the cement–cement interface, it does not validly replicate the in vivo situation. Furthermore static tests of the cement–cement interfaces have been employed and these are less than ideal. Because the cement within cement construct undergoes cyclical loading in vivo, fatigue testing rather than static testing is the more appropriate testing mode [4].
Illustration demonstrating the formation of the cement specimens in 11. The cylinders of bone cement will be bonded “end on” to the previously harderned cement. This will produce a two-dimensional cement–cement interface
The outer cement mantle can also be 10–15 years old at the time of the cement within cement revision. This mantle could be reproduced in vitro by using a similar cement mixing and introduction techniques similar to those used 10–15 years before the study date. Cement prepared in such a fashion will have different mechanical properties to cement prepared with the most modern cement mixing generation. Emphasis should also be placed on using the same operative instruments in vitro that are used in the operation in vivo.
Greenwald et al. and Weinrauch et al. did not test all of their specimens, citing that an accurate surface area of the interface could not be calculated if pores were present. This is in accordance with current recommendations from the American Society for Testing and Materials (ASTM) International group (ASTM International Subcommittee F04.15, 2003). Pores will also occur when cementing in the in vivo procedure. If they do occur, there is no opportunity to revise that prosthesis straight away. Thus this practice of discarding specimens due to porosity is a questionable experimental technique [25] and this should be taken into account when interpreting the results of Greenwald et al. and Weinrauch et al.
Rosenstein et al. tested their specimens only 90 min after their formation. Polymerization of the cement would still be occurring at a relatively high rate at this time. A hardening period of 24 h is recommended in the International standards before the commencement of testing (International Organisation for Standardization and British Standards [14]).
Future biomechanical research could concentrate on the above areas to analysis the cement within cement construct. This would produce results that depicted the in vivo situation more accurately. The conditions that have been previously studied (effect of rasping of the “old” cement, etc.) could be reassessed in the more complex testing.
The clinical research was well conducted and we argue can be taken as supportive of the cement-in-cement technique. However, future research could attempt to follow a larger cohort of patients for a longer length of time. An expertise based prospective randomized controlled trial with paired comparison could be undertaken [5, 26]. This trial could compare patient outcomes of the cement-in-cement procedure to a comparable group of patients undergoing either conventional cemented revisions or uncemented revisions. This study modality has been successful conducted in Orthopedic surgery in the past [9, 28, 29]. The operative time, blood loss, financial cost and rehabilitation time for patients undergoing cement-in-cement procedures could be further investigated to delineate these advantages of the procedure more clearly.
The analysis presented in this paper consolidates the latest biomechanical and clinical information on cement-in-cement revision hip arthroplasty. Although we find evidence to support the use of the method clinically, we do note that the biomechanical basis needs further investigation.
Revision hip arthroplasty is difficult and will become more prevalent in the future. Cement within cement revisions, when indicated, have a number of advantages over other revision methods. We conclude that if other Orthopaedic centres can emulate the results of the clinical research presented, complication rates, operative times and financial costs of revision hip arthroplasty may be decreased.
References
Briant-Evans TW, Norton MR, Fern ED (2007) Fractures of Corin ‘Taper-Fit’ CDH stems used in ‘cement-in-cement’ revision total hip replacement. J Bone Joint Surg Br 89:393–395
Canale ST (2003) Campbell’s operative orthopaedics. Mosby, St Louis
Cook SM, Huo MH (2002) Revision of the femoral stem using cement fixation. Curr Opin Orthop 13:53–55
Davies JP, Harris WH (1993) Strength of cement–metal interfaces in fatigue: comparison of smooth, porous and precoated specimens. Clin Mater 12:121–126
Devereaux PJ, Bhandair M, Clarke M, Montori VM, Cook DJ, Yusuf S, Sackett DL, Cina CS, Walter SD, Haynes B, Schunemann HJ, Norman GR, Guyatt GH (2005) Need for expertise based randomised controlled trials. BMJ 330:88–93
Economic and Social Research Institute (2007) Hospital In-Patient Enquiry Scheme files. Discharges that had a revision of arthroplasty of hip procedure, Dublin, Ireland (http://www.esri.ie/health_information/hipe/)
Eftehar NS (1978) Principles of total hip arthroplasty. Mosby, St Louis
Feith R (1975) Side-effects of acrylic cement, implanted into bone. Acta Orthop Scand 161:1–136
Finkemeier CG, Schmidt AH, Kyle RF, Templeman DC, Varecka TF (2000) A prospective, randomised study of intramedullary nails inserted with and without reaming for the treatment of open and closed fractures of the tibial shaft. J Orthop Trauma 14:187–193
Greenwald AS, Combs SP, Wilde AH, Fleck WG, Black JD (1975) Comparative studies of the bonding strength of new and old acrylic bone cements. Surg Forum Proceedings of the ACS, San Francisco 26:505–506 (Proceedings of the ACS, San Francisco)
Greenwald AS, Narten NC, Wilde AH (1978) Points in the technique of recementing in the revision of an implant arthroplasty. J Bone Joint Surg Br 60:107–110
Herberts P, Karrholm J, Garellick G (2005) Annual Report, The Swedish National Hip Arthoplasty Register
Hubble M, Patten A, Duncan W, Howell J, Timperley AJ, Gie G (2005) Cement in cement femoral revision with the Exeter hip. EFORT (Lisbon), abstract no. F213
International Organisation for Standardization and British Standards (2002) Implants for surgery-acrylic resin cements, 2nd edn
Kurtz SM, Lau E, Zhao K (2006) The future burden of hip and knee revisions: US projections from 2005 to 2030. AAOS 73rd Annual meeting Chicago SE-53
Li PL, Ingle PJ, Dowell JK (1996) Cement-within-cement revision hip arthroplasty; should it be done? A biomechanical study. J Bone Joint Surg Br 78:809–811
Lieberman JR (2005) Cemented femoral revision, lest we forget. J Arthroplasty 20:72–74
Lieberman JR, Moeckel BH, Evans BG, Salvati EA, Ranawat CS (1993) Cement-within-cement revision hip arthroplasty. J Bone Joint Surg Am 75:869–871
McCallum JD, Hozack WJ (1995) Recementing a femoral component into a stable cement mantle using ultrasonic tools. Clin Orthop Relat Res 319:232
Meek RM, Garbuz DS, Masri BA, Greidanus NV, Duncan CP (2004) Intraoperative fracture of the femur in revision total hip Arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am 86:480–485
Nabors ED, Liebelt R, Mattingly DA, Bierbaum BE (1996) Removal and reinsertion of cemented femoral components during acetabular revision. J Arthroplasty 11:146–152
Nelson CL (2002) Cemented femoral revision: technique and outcome. Am J Orthop 31:187–189
Quinlan JF, O’Shea K, Doyle F, Brady OH (2006) In cement technique for revision hip arthroplasty. J Bone Joint Surg Br 88:730–733
Rosenstein A, MacDonald W, Iliadis A, McLardy-Smith P (1992) Revision of cemented fixation and cement–bone interface strength. Proc Inst Mech Eng [H] 206:47–49
Prendergast PJ, Murphy BP, Taylor D (2000) Discarding specimens for fatigue testing of orthopaedic bone cement: a comment on Cristofolini et al. Fatigue Fract Eng Mater Struct 25:953–957
Van der Linden W (1980) Pitfalls in randomized surgical trials. Surgery 87:258–262
Weinrauch P, Bell C, Wilson L, Goss B, Lutton C, Crawford R (2007) Shear properties of bilaminar polymethylmethacrylate cement mantles in revision hip joint arthroplasty. J Arthroplasty 22:394–403
Wihlborg O (1990) Fixation of femoral neck fractures. A four-flanged nail versus threaded pins in 200 cases. Acta Orthop Scand 61:415–418
Wyrsch B, McFerran MA, McAndrew M, Limbird TJ, Harper MC, Johnson KD, Schwartz HS (1996) Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Joint Surg Am 78:1646–1657
Acknowledgments
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keeling, P., Prendergast, P.J., Lennon, A.B. et al. Cement-in-cement revision hip arthroplasty: an analysis of clinical and biomechanical literature. Arch Orthop Trauma Surg 128, 1193–1199 (2008). https://doi.org/10.1007/s00402-007-0470-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0470-0