Abstract
Introduction
In spite of carpal tunnel release’s prevalent good postoperative results, the number of revision surgeries needed should not be underestimated. In this study, subjective and functional results after carpal tunnel revision surgery were determined.
Materials and methods
Thirty-eight patients were examined approximately 2 years after their revision surgery of the carpal tunnel release. The subjective outcome of the patients was assessed using two different questionnaires (Amadio and DASH). A clinical examination was undertaken on selected patients who had persistent complaints. The clinical assessment analyzed grip strength, thumb opposition, pulp-to-pulp-pinch, key-pinch, hook-grip, Moberg-Pickup-test, two-point-discrimination, Phalen-test, and the Hoffmann–Tinel-sign.
Results
The subjective assessment showed that after the revision surgery, patients experienced load induced pain that occurred during daytime. However, the revision was able to improve the impaired sensibility. The functional outcome showed a persistent lack of strength when performing daily activities. The clinical assessment of the patients with relevant complaints confirmed the subjective outcome.
Conclusion
The revision surgery can improve the impaired sensibility, particularly, paresthesia nocturna. The persistent weakness of the hand can only partly be improved. In spite of remaining complaints, revision surgery can yield satisfactory results for the patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The carpal tunnel syndrome represents the most common nerve compression syndrome of a peripheral nerve and, simultaneously, constitutes the most frequent neurological disorder of the hand [2, 9]. A careful estimate shows that revision surgeries after carpal tunnel release are needed in about 0.5% of cases [4]. Since carpal tunnel release surgeries are performed so frequently, it follows that their revision surgeries are quite relevant from a clinical point view.
In this study, we examined patients who underwent revision surgery due to postoperative complaints after carpal tunnel release. Using two questionnaires (Amadio, DASH) the subjective results after revision surgery could be determined. Moreover, patients with relevant persistent complaints after revision were again clinically examined evaluating the aspects of function, sensibility and strength.
Materials and methods
Patients
Of the 43 patients who were contacted, 38 patients (average age 61 years) were able to be examined 2 years after the revision surgery was performed (14 men, 24 women). Thirty-two carpal tunnel release surgeries were performed in other hospitals, six in our own hospital. All in all 35 were performed using an open technique and 3 endoscopically. The open release was done in 21 cases by making a short incision that did not exceed 3 cm in length and that reached from the middle hand to the rascetta. In eight operations, a long incision was made by opening all the way from the middle hand to the forearm including the fascia on the radial or ulnar side. Due to the excellent healing of the scars it was impossible to determine the kind of surgical cuts made in six cases. The endoscopic operations were performed in accordance with the two portal method after Chow [5]. Thirty-four patients underwent revision surgery. Two patients were in need of an additional third surgical intervention. Two females were even in need of a fourth and fifth operation, respectively.
Pre-operative complaints (before revision surgery)
A total of 95% of patients suffered from impaired sensibility in the area innervated by the median nerve. Pain in the hand and wrist area during daytime was experienced by 53% of patients, whereas 34% indicated that they were bothered with typical paresthesia nocturna; 47% of patients expressed concern over a reduction of strength in the affected hand. In over half of the patients the complaints persisted and remained unchanged after the first carpal tunnel release surgery had been performed and 42% of the patients even indicated that they experienced a renewed worsening of symptoms after an initial improvement had occurred following the surgery. Two patients reported an immediate postoperative deterioration of symptoms. Intra-operative complications with a resultant iatrogenic injury of the median nerve occurred in one female patient. Carpal tunnel syndrome on both sides was diagnosed in 36% of cases.
Revision surgery
The indication for revision surgery was the recurrence of the typical carpal tunnel symptoms. Before the revision surgery the patients were examined using electro diagnostic tools. This examination was performed by a neurologist. The latency and velocity of the median nerve was found to be pathologically increased, but there was no correlation between postoperative outcome and nerve latency/velocity.
In 26 patients, the carpal tunnel release was performed on the right hand and in 12 patients on the left. The revision surgery was performed 1 month to 4 years after the initial surgery. Within 6 months, 15 patients underwent revision surgery. Fifteen other patients had revision surgery in the time interval between 6 months and 2 years after the first surgery. Eight patients waited even more than 2 years to have their revision done.
The revision surgery was always performed using axillary plexus anesthesia and tourniquet. The incision was done in the extension of the fold of the third interdigital region reaching from the middle hand to the rascetta and then extending diagonally to the ulnar side of the forearm.
During the operation 32 patients had synovitis in the carpal tunnel. As a result, 32 synovectomies were performed. In cases where the median nerve was found to be freely exposed, we performed a hypothenar-fat-padflap to cover the nerve. This occurred in four patients. In three patients, a resection of the palmar cutaneous branch of the median nerve was made due to the occurrence of neuroma. The tendon of the palmaris longus was resected in one case. A Z-plastic was required in ten cases so that scar tissue could be dissolved.
Intra-operative findings
See Table 1 for the intra-operative findings.
Questionnaires
Patients were asked to complete two different questionnaires: the Amadio questionnaire [1] and the DASH questionnaire [7]. The Amadio questionnaire is made up of 29 questions pertaining to symptom related complaints, limitations of function and post-operative satisfaction. The patient can choose from five possible answers (e.g., none, hardly, some, significant, great difficulties). The DASH questionnaire assesses the global functioning of the upper extremity and is divided into three parts asking the patient to provide information on function, symptoms and special activity. Up until the analysis of the questionnaires and the clinical re-examinations none of the patients had undergone a further surgical intervention. Five patients who had undergone several pre-operations were asked to provide information with regards to their last surgery.
Selection of patients for clinical re-examination
Patients were chosen for clinical re-examination based on their answers of the Amadio questionnaire section called “symptom related complaints” (persistent pain, dysesthesia, limitations of function). We selected those patients who indicated a value of 4 = poor or 5 = very poor at least once in this particular section.
Eighteen patients were contacted to participate in the clinical re-examination. Sixteen patients (11 women, 5 men) with an average age of 58 years were re-examined (88%; see Table 2 for intra-operative results). These 16 patients were part of the group “patients with significant remaining complaints” (wRB) and compared with the other 20 patients that make up the group “successful operation” (OPE).
Clinical examination of the patients with significant persistent complaints
The methods employed for clinical re-examination are described in Table 3. Patients were asked to evaluate post-operative improvement and surgical result. In addition, an inquiry was made to find out whether or not the patient, judging retrospectively, would undergo surgery again.
Statistics
The statistical calculations were made using SPSS® 7.5 (SPSS Inc., Chicago, USA). The Mann–Whitney-U-test, the logical regression and the correlation coefficient were determined according to Spearman.
Results
Amadio questionnaire
Symptoms related to pain
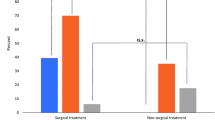
In spite of 57% of patients being free of pain 18% reported persistent, very strong pain during day- and nighttime. All in all, 84% of patients indicated experiencing no, little, or only moderate pain. Therefore, the revision surgery can be considered a significant success regarding the reduction of pain. In comparison with the OPE group a significant difference (P < 0.001) can be determined (Fig. 1).
Impaired sensibility and weakness
Thirty-six patients were free of paresthesia nocturna or experienced it only slightly (94%). Thirty-five patients reported that they either never or only infrequently awoke during the night due to paresthesia nocturna (92%). Eleven patients (28%) indicated strong or even very strong persistent symptoms of weakness. Nine patients still complained of a moderate weakness (23%) and only 17 of patients (44%) had none or only slight symptoms of weakness. The values indicating strong or very strong symptoms of weakness were chosen by patients who also suffered from impaired sensibility. The poor values regarding symptoms of weakness were found mostly in patients who at the same time suffered from impaired sensibility. All in all, it could be shown that there was a significant improvement in the symptoms of paresthesia while symptoms of weakness partly persisted.
Limitations of function
A total of 26% of patients complained of strong or very strong limitations of function. The fact that function was impaired became evident when patients performed daily tasks that require strength, such as opening a bottle or carrying a bag. Additionally, activities that necessitate relatively little strength, for example writing a letter, were reported to be severely or even very severely limited in 23% of patients. Patients with “successful operations” (OPE) showed significantly decreased values in the Amadio-score in comparison to “patients with significant remaining complaints” (wRB) in the category function (Fig. 2).
Scale of satisfaction
The majority of patients were sufficiently satisfied with the post-operative results. A total of 94% of patients were completely or sufficiently content with the symptoms they experienced at nighttime. Regarding the paresthesia 76% of patients indicated that they were completely or sufficiently satisfied. The results concerning the aspects of the pulp-to-pulp pinch, strength and ability to do daily activity show a distinct dissatisfaction. The results in postoperative strength showed that 36% of patients were entirely dissatisfied. Of those patients, 31% were concerned about the pulp-to-pulp pinch and 23% were worried about their ability to do work around the house.
DASH
The median value of the overall DASH was 35. Part A, which concerned the limitations of function, yielded a median value of 34. Part B, providing the information on symptoms, arrived at a value of 41. Comparing the median values of part A and B becomes evident that the results for part B are distinctly worse. Symptoms of pain that are induced by load and occur during daytime dominate the complaints in the section on symptoms. In the part of the questionnaire covering the limitations of function, patients were mainly concerned with a persistent weakness that resulted in further limitation when carrying out tasks requiring strength. Patients with good post-operative results (OPE) showed significantly lower DASH values overall, part A and part B, in comparison with patients with poor post-operative results (wRB; Figs. 3–5).
Clinical examination
Solely one female patient exhibited the phenomenon of the incomplete fist. The other 15 patients were able to make a fist. The ability to extend the fingers was present in ten patients. In four patients, extension of the fingers was borderline limited and in two patients impossible. The thumb opposition was possible in all patients. Tests examining the ability to grip revealed that three patients were unable to make a pulp-to-pulp pinch. In one of those three patients the hook and key pinch was also not possible. The hook pinch was borderline pathological in four patients, the key pinch only in one patient. Measuring the strength in the operated hand using Jamar setting 2 (Jamar, Sammons Preston Inc., Bollingbrook, IL, USA) it could be shown that it was between 45 and 67% weaker (P < 0.05) than the opposite hand.
Only one female patient experienced severely impaired sensibility in the dynamic two-point-discrimination. The clinical re-examination of that patient included the test on dynamic two-point-discrimination in the area being innervated by the median nerve. The result of it was a median value of 15 mm. In contrast, all other patients undergoing this test produced a median value of 6 mm for that same area.
The Hoffmann–Tinel-sign and the Phalen-test yielded positive results in over half of all patients. Paresthesia in the area of palmar cutaneous branch of the median nerve during daytime and also a pain induced by pressure in the area of the distal wrist crease were still present in 7 out of 16 patients. When questioning patients during the clinical re-examination, eight patients indicated a post-operative improvement of symptoms, whereas, only four answered in the negative. Asked if they would undergo the last surgery again, 12 answered in the affirmative in contrast to four who would refuse it. Six patients reported the operative results to be poor. However, ten patients provided very good or satisfactory marks for the post-operative results.
Discussion
The revision of the release of the carpal tunnel is underestimated in terms of the number performed and the technical difficulty required. A recently published study by a clinic specializing in hand surgery showed that in a time frame of 26 months, 108 revisions were necessary due to incomplete severance of the flexor retinaculum [11]. This high number highlights the clinical relevance of the revision surgery.
Assmus reported an incomplete severance occurring in 49.2% of patients [2]. In our group of patients this even happened in 68% of cases. Baranowski et al. reported an incomplete severance in 60% [12]. Typically, an incomplete severance clinically entails an immediate worsening of symptoms or a re-occurrence of symptoms after several weeks of experienced improvement. An incomplete severance occurred in the group of patients with good post-operative results, as well as, in the group of patients who still suffered from persistent symptoms. Both groups had a similar percentage of cases in which an incomplete severance was present. Our data was able to show that prompt revision surgery after incomplete severance yields good post-operative results. We noted that a majority of patients with incomplete severance also exhibited poor post-operative results had let several years pass between the initial surgery and the revision. As a result, poor post-operative results could be avoided if a revision was performed soon after the initial surgery. Similar results were found by Baranowski et al. They recommend that patients with persistent or early recurrent complaints after carpal tunnel release should undergo revision surgery after a neurophysiological and clinical diagnosis [12]. Most often an intra- or postoperative complication is the cause of the persistent or early recurrent complaints [12].
In their study of 56 revisions of the carpal tunnel release Büchler et al. describe an early onset of an epineural fibrosis in terms of an “overshooting scarring reaction”. The authors speculate that the reason for this occurrence is an individual predisposition. Regarding the post-operational course of healing the group with the early fibrosis showed a significantly worse result than the other patients [4]. A manifestation of early fibrosis took place in eight cases in our group of patients. Of those eight cases, five occurred in patients with persistent complaints and three in patients who experienced good post-operative results. Our experience shows that good results in patients with early onset of fibrosis can be achieved when a hypothenar-fat-padflap [6] is done to cover the median nerve. Frank et al. speculate that usage of this kind of a padflap allows the median nerve to better be movable along a longitudinal axis and to adhere less to surrounding tissue. The increased mobility and flexibility of the nerve may lead to better post-operative results [6].
In cases of correct carpal tunnel release, the flexor retinaculum can sometimes close up again, as a part of the healing process. This situation is called a “real” recurrence. “Real” recurrence can necessitate revision, too. Assmus found 58 “real” recurrences in his group of 185 patients (31.4%). In 80% of those 58 patients relapse occurred in patients undergoing dialysis treatment [2]. Assmus and Staub were able to achieve improved results in patients with carpal tunnel recurrence and who are simultaneously undergoing long-term hemodialysis. They brought about better results by performing a resection of the superficial flexor tendon [3]. The authors recommend that this kind of excision is done in patients who have received dialysis treatment for more than 20 years or have tendo- and arthropathy. At the very latest, a resection should be performed when they have experienced their second carpal tunnel relapse. In our study, cases with “real” recurrence showed good results regarding the recovery of sensibility, as well as, function. The results are similar to the results of recovery of sensibility of late fibrosis.
When we evaluated the Amadio questionnaire, we found that patients were almost completely free of complaints regarding paresthesia nocturna. Pain occurred mostly during daytime and when patients performed tasks requiring strength. The reduction of available strength can mainly be explained by atrophy in the thenar muscle. This particular region functions as an opposition in many hand activities and plays a significant role even when the thenar musculature is not directly involved in the activity.
When comparing the results of the Amadio with the DASH questionnaire we saw that the results of Amadio were mostly confirmed. However, the DASH questionnaire clearly emphasizes complaints regarding symptoms.
The results of the clinical re-examination correlate to a large extent with the analysis of the questionnaires. It was noticeable that next to the reduction of strength in the affected hand people also experienced limitations when performing tasks requiring fine motor skills.
Pain stemming from scars in the area of the incision and simultaneous discomfort occurring in the area of the annular ligaments [13] must be clinically differentiated from neurological symptoms derived from the carpal tunnel recurrence. In patients undergoing dialysis treatment carpal tunnel syndrome and trigger finger concurred frequently [10]. Another study showed that patients with diabetes mellitus and/or patients with high blood pressure also have a tendency to suffer of carpal tunnel relapse [8]. When patients only suffer of discomfort due to scarring and exhibit no neurological symptoms, the usage of silicon sheets and information on the healing process of scars have been proven practice [14].
The revision of the carpal tunnel release shows a good prognosis in improving impaired sensibility, in particular, paresthesia nocturna. The ability to achieve good results concerning the complaints of persistent weakness and reduction of strength is rather limited. Revision surgery should be especially considered in cases with complaints lasting several weeks or in cases where a recurrence of symptoms after initial improvement has taken place. An electrophysiological examination is prerequisite for the diagnosis. A revision in open technique should follow. The hypothenar-fat-padflap provides a solid coverage of soft tissue and yields good results in cases where adhesion and scarring of the median nerve is present. Pain derived from skin scarring processes does not represent an indication for surgery. It should be dealt with employing conservative methods, such as silicon sheet and massaging the scars.
References
Amadio PC, Silverstein MD, Ilstrup DM, Schleck CD, Jensen LM (1996) Outcome assessment for carpal tunnel surgery: the relative responsiveness of generic, arthritis-specific, disease-specific, and physical examination measures. J Hand Surg (Am) 21:338–346
Assmus H (1996) Correction and reintervention in carpal tunnel syndrome. Report of 185 reoperations. Nervenarzt 67:998–1002
Assmus H, Staub F (2005) Recurrences of carpal tunnel syndrome in long-term haemodialysis patients. Handchir Mikrochir Plast Chir 37:158–166
Buchler U, Goth D, Haussmann P, Lanz U, Martini AK, Wulle Ch (1983) Karpaltunnelsyndrom: Bericht über 56 Nachoperationen. Handchir Mikrochir Plast Chir 15:3–12
Chow JC (1989) Endoscopic release of the carpal ligament: a new technique for carpal tunnel syndrome. Arthroscopy 5:19–24
Frank U, Giunta R, Krimmer H, Lanz U (1999) Relocation of the median nerve after scarring along the carpal tunnel with hypothenar fatty tissue flap-plasty. Handchir Mikrochir Plast Chir 31:317–322
Germann G, Wind G, Harth A (1998) The DASH(Disability of Arm–Shoulder–Hand) questionnaire—a new instrument for evaluating upper extremity treatment outcome. Handchir Mikrochir Plast Chir 30:1–4
Schreiber JE, Foran MP, Schreiber DJ, Wilgis EF (2005) Common risk factors seen in secondary carpal tunnel release. Ann Plast Surg 55:262–265
Skorpik G, Zachs I (1998) Carpal tunnel syndrome. Orthopade 27:583–598
Staub F, Dombert T, Assmus H (2005) Carpal tunnel syndrome in haemodialysis patients: analysis of clinical and electrophysiological findings in 268 patients (395 hands). Handchir Mikrochir Plast Chir 37:150–157
Stutz N, Gohritz A, van Schoonhoven J, Lanz U (2006) Revision surgery after carpal tunnel release—analysis of the pathology in 200 cases during a 2 year period. J Hand Surg (Br) 31:68–71
Baranowski D, Klein W, Grunert J (1993) Secondary surgery for carpal tunnel syndrome. Handchir Mikrochir Plast Chir 25:127–132
Unglaub F, Kall S, Reiter A, Hahn P (2005) Stenosing tenovaginitis—is injection therapy beneficial? Z Orthop Ihre Grenzgeb 143:475–478
Ziegler UE (2004) International clinical recommendations on scar management. Zentralbl Chir 129(4):296–306
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Unglaub, F., Wolf, E., Goldbach, C. et al. Subjective and functional outcome after revision surgery in carpal tunnel syndrome. Arch Orthop Trauma Surg 128, 931–936 (2008). https://doi.org/10.1007/s00402-007-0451-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0451-3