Abstract
Introduction
One aim of the surgical treatment of acute Achilles tendon ruptures is to obtain a maximum primary stability of the sutured tendon. Therefore, we investigated the primary stability of sutured human Achilles tendons depending on different applied techniques.
Methods
The strength of 60 repaired cadaveric human Achilles tendons was tested depending on either the suture technique (Bunnell or Kessler), the suture material (PDS-thread or PDS-cord) or an additional plantaris tendon augmentation (PDS-thread with or without augmentation). Following anatomic reconstruction the repaired specimens were loaded to failure.
Results
The use of Bunnell's technique resulted in a stronger primary suture stability compared to Kessler's technique. Sutures carried out with a PDS-thread were of lower strength than those accomplished with a PDS-cord (Bunnell: thread 139 N ± 29.8; cord 291 N ± 55.2/Kessler: thread 137 N ± 37.3; cord 180 N ± 41.1). Sutures performed according to Bunnell's technique with a PDS-thread and an additional autologous plantaris tendon augmentation reached the highest primary stability (326 N ± 124.9).
Conclusions
The findings identify the Achilles tendon suture with a PDS-cord according to Bunnell's technique as a mechanically strong method. A plantaris tendon augmentation in addition to a PDS-thread can even add more stability to the Achilles tendon suture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ruptures of the Achilles tendon are steadily increasing in frequency due to the increase in sport activities of modern societies. Depending on the social environment about 18 out of 100,000 humans sustain a rupture of the Achilles tendon every year [1, 3, 15, 19, 22, 24–26].
The optimal therapy regime (i.e. surgical versus functional-conservative) of fresh Achilles tendon ruptures has been the subject of intensive debate for many years [2, 3, 6, 7, 13–20, 30]. However, in 88.7% the open surgical suture of the ruptured tendon is favored in Germany [16]. For Achilles tendon repair almost 60 different techniques have been described so far [8]. The techniques established by Kessler, Bunnell, Lange and Kirchmeyer are applied most frequently [8, 16, 30]. According to Lill [16], an additional augmentation of the repaired tendon by the plantaris tendon is only applied in about 30% of all trauma–surgical departments in Germany. The plantaris tendon, which exists in about 90% of the patients, is regularly used as an autologous transplant in reconstructive surgery [9, 18, 28].
On the basis of the enormous heterogeneity of surgical suture techniques in the repair of the Achilles tendon, a procedure which results in a maximum mechanical stability of the sutured Achilles tendon is desirable. This could also help to reduce the number of reruptures, which is observed in up to 5% of the patients treated with an open surgical suture [7, 17, 29].
Only few biomechanical studies have investigated the primary stability of sutured (human) Achilles tendons so far [10, 21, 27, 31]. None of these studies examined the stability of sutured human Achilles tendons under consideration of an additional plantaris tendon augmentation.
Therefore, the presented biomechanical study investigates the primary stability of human cadaveric ruptured Achilles tendons after suture–repair as a function of (1) the suture technique, (2) the suture material as well as (3) an additional plantaris tendon augmentation.
Materials and methods
Specimens
Sixty human cadaveric Achilles tendons were tested altogether. Tendons, namely the complete muscle–tendon–bone-units, were removed from 30 acutely deceased patients (74% males, 26% females) with an average age of 44.9 years (15–67 years) within 12 h post mortem and stored at −20°C until suture. In 83% of the preparations a plantaris tendon was found. The study was carried out according to existing rules and regulations of Hamburg University School of Medicine. Chronic cardiovascular or endocrine diseases, diabetes, corticoid therapy as well as previous ruptures of the Achilles tendon were considered as an exclusion criteria. Non of the patients had received an intratendinous injection. Ten preparations were randomly assigned to each of the six different subgroups (see below).
Achilles tendon suture
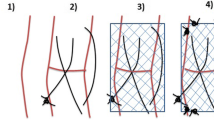
The Achilles tendons were transversely transected with a conventional scalpel 50 mm proximal of their insertion at the tuber calcanei. After dissection, the tendons were sutured according to Bunnell's (group A) or Kessler's (group B) technique, partly with an additional plantaris tendon augmentation (Fig. 1a–d). The suture material consisted of absorbable polydioxanone (PDS) and was either a thread (strength 1, metric 4, Ethicon, Norderstedt, Germany) or a cord of 0.7 mm diameter (Ethicon, Norderstedt, Germany). In addition to this thread suture a plantaris tendon augmentation was carried out in two subgroups (Fig. 1c), using a soft edged Jungbluth’s needle (Fig. 1d) for guiding the tendon through and to avoid destroying of the previously applied sutures. The most proximal and distal transverse passes of the suture material through the tendon was led 30 mm away from the transection plane. To ensure reliability as well as exact suturing and augmentation techniques all sutures were carried out by two experienced trauma surgeons.
Scheme of frequently applied open suture techniques in Achilles tendon repair: Kessler a, Bunnell b. A standardized open suture procedure is shown in c depicting an additional plantaris tendon augmentation carried out with Jungbluth's needle (d). For axial load testings, the muscle–tendon–bone-complex is placed into the Instron device and loaded under constant speed of 0.0166 m/s (e)
Test set-up
After the suture was carried out the muscle–tendon–bone-complex was directly clamped into a dynamic testing device (Instron Model 1195, Canton, MA, USA). According to Thermann, the calcaneus was bolted distally of the achillo-calcanear transition onto a steel plate (Fig. 1e) [24, 25]. The sutured triceps surae muscle was put into a special steel pot and fixed by rapid freezing with liquid nitrogen for 60 s. The entire clamping length amounted to approximately 150 mm. The dynamic testing took place under axial tension with a constant speed of 1.66 mm/s. Failure forces (N) were determined by the yield point in the stress strain curve at which the suture material failed or the suture pulled out from the tendon.
Statistics
Results are presented as mean value ± SD. Statistical analysis of the biomechanical data was performed with the Kruskal–Wallis One-Way ANOVA. A P < 0.05 was considered to be of statistically significance.
Results
All 60 muscle–tendon–bone-units were tested in the Instron device without any setup failure at the muscular or osseous fixation points (Fig. 1e).
The mean, maximum and minimum load to failure forces (N), the corresponding standard deviations as well as the number of suture ruptures and thread or cord pull outs from the tendon of the six tested groups are shown in Table 1 and Fig. 2. Tendons sutured with a PDS-thread had the lowest load to failure forces (Bunnell group 139 N ± 29.8, Kessler group 137 N ± 37.3) and six ruptures out of ten sutured tendons in the Bunnell group and three out of ten in the Kessler group occurred. In contrast, four threads pulled out the tendon in the Bunnell group, whereas in the Kessler group seven pulled out.
Sutures accomplished with a PDS-cord showed a higher primary stability (Bunnell group 291 N ± 55.2; Kessler group 180 N ± 41.1). As a consequence, five cord ruptures in the Bunnell group and one in the Kessler group were observed. In the Kessler PDS-cord group nine out of ten sutures failed by pulling out of the tendon, whereas in the Bunnell PDS-cord group five out of ten sutures pulled out of the tendon.
If in addition to a PDS-thread suture a plantaris tendon augmentation was performed, the tendon suture presented the strongest primary stability (Bunnell group 326 N ± 124.9; Kessler group 211 N ± 60.4). Here, the augmented Bunnell as well as Kessler PDS-thread sutures failed in all cases due to suture/plantaris tendon-pull out from the tendon after prior thread ruptures at lower force values.
If in addition to the PDS-thread suture in the Kessler group a plantaris tendon augmentation was carried out, the primary stability of the tendon could be increased by 54%. Similarily an increase of the primary suture stability of 134% was achieved by an additional plantaris tendon augmentation in the Bunnell group.
In our test series, the PDS-thread suture according to Bunnell’s technique under simultaneous plantaris tendon augmentation, represented the most stable treatment of the ruptured Achilles tendon.
Discussion
Until today the type of surgical treatment of ruptured Achilles tendons is still the subject of controversial debates. Even if—based on biomechanical studies—differentiated treatment concepts concerning the therapy of the freshly ruptured tendon exist, the majority of surgeons exclusively treat an Achilles tendon rupture by a primary open surgical suture [3, 17, 25, 30].
The biomechanical investigations presented here aimed to determine the Achilles tendon suture with the highest primary stability. Of all described different suture techniques, the two techniques described by Kessler and Bunnell were tested in this study which in the clinical practice are applied most frequently [8, 16, 30]. In the presented test series the PDS-thread showed the lowest maximum strength with six material ruptures in the Bunnell group and three in the Kessler group. Compared to that the PDS-cord reached a higher primary stability of the suture. In the Kessler group 90% of the sutures performed with a PDS-cord failed by pulling out of the tendon ends at an average of 180 N, whereas in the Bunnell group a cord pull-out occurred at an average force of 291 N. In a comparable study concerning the primary stability of 18 sutured human Achilles tendons, Watson et al. [27] determined a lower tear strength. Here, the average stability of the sutured tendon accounted for 85 N in the Kessler group and 93 N in the Bunnell group, whereby all sutures failed by thread rupture. The suture material used by Watson (No. 1 Ethibond) seems to be less stable than the suture material used in our study. In another study Yildirim performed a biomechanical test on the strength of the sutured sheep Achilles tendon and found lower suture pull out forces in the Kessler group (101 N) compared to those in the Bunnell group (197 N) [31]. The higher stability of the sutured tendons in the Bunnell group is caused by an increase of the coefficient of friction between the tendon and the thread surface. As a consequence, the Bunnell’s thread has a larger contact area with the proximal and distal tendon stumps [11, 31].
In our study the strongest tendon suture was obtained by using a PDS-thread with simultaneously performing an additional plantaris tendon augmentation. Here, the augmented Bunnell suture failed at an average of 328 N due to a suture pull out in all cases, whereas the underlying PDS-thread ruptured at lower force values. In the Kessler group an average maximum strength of 211 N was observed and the underlying PDS-threads likewise ruptured at lower force values.
The higher stability of the augmented suture also seems to be attributable to an increase of the coefficient of friction caused by a larger contact area of the suture material with the surrounding tendon tissue. Besides that the plantaris tendon extensively bridges the rupture area and thus can be regarded as a biological guide rail for the following reparative process.
Regarding the proprioceptive function of the plantaris tendon–muscle-unit, there is no data existing in the current literature. Even if there is evidence that tactile and proprioceptive information from the foot sole and the flexor ankle muscles might subserve the maintenance of errect stance and that patients with a previous history of Achilles tendon rupture display proprioception deficits, the role of the plantaris tendon within the neural triceps surae muscle–tendon-complex remains unclear [4, 5, 12, 23]. Thus, the consequences of plantaris tendon dissection during plantaris tendon augmentation for ankle joint proprioception cannot be predicted.
Summing up, the observations made in this study demonstrate that in addition to the used suture material the applied suture technique also has a crucial influence on the primary stability of the Achilles tendon suture. With the selection of an appropriate thread or cord, the suture technique must be individually adjusted to the applied suture material. Thus, the basically strong Bunnell technique can only develop a maximum strength if a sufficiently loadable suture material is selected. Further stability to the Achilles tendon can be added by an additional plantaris tendon augmentation suture which is likely to be attributable to an increase of the coefficient of friction.
References
Arner O, Lindholm Å (1959) Subcutaneous rupture of the Achilles tendon. A study of 92 cases. Acta Chir Scand 239(Suppl)
Assal M, Jung M, Stern R et al (2002) Limited open repair of Achilles tendon ruptures: a technique with a new instrument and findings of a prospective multicenter study. J Bone Joint Surg (Am) 84:161–170
Bhandari M, Guyatt GH, Siddiqui F et al (2002) Treatment of acute achilles tendon ruptures. A sytematic overview and metaanalysis. Clin Orthop 400:190–200
Bressel E, McNair PJ (2001) Biomechanical behavior of the plantar flexor muscle–tendon unit after an Achilles tendon rupture. Am J Sports Med 29:321–326
Bressel E, Larsen BT, McNair PJ et al (2004) Ankle joint proprioception and passive mechanical properties of the calf muscles after an Achilles tendon rupture: a comparison with matched controls. Clin Biomech 19:284–291
Buchgraber A, Pässler HH (1997) Percutaneus repair of Achilles tendon rupture: immobilization versus functional postoperative treatment. Clin Orthop 341:113–122
Cetti R, Christensen SE, Ejsted R et al (1993) Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med 21:791–799
Crolla RMPH, van Leeuwen DM, van Ramshorst B et al (1987) Acute rupture of the tendo calcaneus. Surgical repair with functional aftertreatment. Acta Orthop Belg 53:492–494
Daseler EH, Anson BJ (1943) The plantaris muscle. An anatomical study of 750 specimens. J Bone Joint Surg 25:822–827
Hockenbury RT, Johns JC (1990) A biomechanical in vitro comparison of open versus percutaneous repair of tendon achilles. Foot Ankle 11:67–72
Holmlund DEW (1977) Suture technique and suture holding capacity: a model study and a theoretical analysis. Am J Surg 134:616–621
Kavounoudias A, Roll R, Roll JP (2001) Foot sole and ankle muscle inputs contribute jointly to human erect posture regulation. J Physiol 532:869–678
Kocher MS, Bishop J, Marshall R et al (2002) Operative versus nonoperative management of acute achilles tendon rupture. Am J Sport Med 30:783–790
Lea RB, Smith L (1972) Non-surgical treatment of tendo achillis rupture. J Bone Joint Surg (Am) 54:1398–1407
Leppilahti J, Orava S (1998) Total Achilles tendon rupture. A review. Sports Med 25:79–100
Lill H, Moor C, Schmidt A et al (1996) Current status of treatment of Achilles tendon ruptures. Results of a nationwide survey in Germany. Chirurg 67:1160–1165
Lo IK, Kirkley A, Nonweiler B (1997) Operative versus nonoperative treatment of acute achilles tendon ruptures: a quantitative review. Clin Sports Med 7:207–211
Lynn TA (1966) Repair of the torn Achilles tendon, using the plantaris tendon as a reinforcing membrane. J Bone Joint Surg (Am) 48:268–272
Maffulli N (1999) Rupture of the Achilles tendon. J Bone Joint Surg (Am) 81:1019–1036
Möller M, Movin T, Granhed H et al (2001) Acute rupture of tendo Achillis. A prospective, randomized study of comparison between surgical and non-surgical treatment. J Bone Joint Surg (Br) 83:843–848
Mortensen NHM, Saether J (1991) Achilles tendon repair. A new method of achilles tendon repair tested on cadaverous materials. J Trauma 31:381–384
Pajala A, Kangas J, Ohtonen P et al (2002) Rerupture and deep infection following treatment of total achilles tendon rupture. J Bone Joint Surg (Am) 84:2016–2021
Sorensen KL, Hollands MA, Patla E (2002) The effects of human ankle muscle vibration on posture and balance during adaptive locomotion. Exp Brain Res 143:24–34
Thermann H, Zwipp H, Tscherne H (1995) Functional treatment concept of acute rupture of the Achilles tendon. 2 years results of a prospective randomized study. Unfallchirurg 98:21
Thermann H, Hüfner T, Tscherne H (2000) Achilles tendon rupture. Orthopäde 29:235–250
Thompson TC (1962) A test for rupture of the tendo Achillis. Acta Orthop Scand 32:461–465
Watson TW, Jurist KA, Yang KH et al (1995) The strength of Achilles tendon repair: an in vitro study of the biomechanical behavior in human cadaver tendons. Foot Ankle 16:191–195
Wening JV, Katzer A, Phillips F, et al (1996) Pre-operatively radiological imaging of musculus plantaris tendon—procedure and anatomical correlations. Unfallchirurgie 22:30–35
Winter E, Ambacher T, Maurer F et al (1995) Surgical therapy of Achilles tendon rupture. Unfallchirurg 98:468–473
Wong J, Barrass V, Maffulli N (2002) Quantitative review of operative and nonoperative management of achilles tendon ruptures. Am J Sport Med 30:565–575
Yildirim Y, Esemenli T (2002) Initial pull-out strength of tendon sutures: an in vitro study in sheep achilles tendon. Foot Ankle 23:1126–1130
Acknowledgments
We thank the Atomic Energy Research Institute, Fuel and Reactor Materials Department, Budapest, Hungary with Dr. Laslo Gillemot and Márta Horváth for the opportunity of biomechanical testing and their technical assistance. This study was supported by technical assistence and research grant from Ethicon GmbH, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gebauer, M., Beil, F.T., Beckmann, J. et al. Mechanical evaluation of different techniques for Achilles tendon repair. Arch Orthop Trauma Surg 127, 795–799 (2007). https://doi.org/10.1007/s00402-007-0325-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0325-8