Abstract
Introduction
This study was initiated to evaluate the reproducibility of a novel method for measuring the periacetabular bone density after insertion of cemented and uncemented acetabular cups using CT in vivo.
Materials and methods
CT scans were obtained from 20 patients after cemented polyethylene cup implantation (ZCA, Zimmer, USA) and 20 patients after uncemented titanium alloy cup fixation (Cerafit, Ceraver, France). A manual segmentation of cancellous and cortical pelvic bone ventral, dorsal and cranial to the cup was undertaken. Values are given in Hounsfield units. Inter- and intraobserver studies were conducted using a special analysis software tool. To define the reproducibility of the method, all measurements were evaluated according to Bland and Altman.
Results
For both cemented and uncemented acetabular cups, reproducibility of bone density measurement for cortical and cancellous bone cranial, ventral and dorsal to the cup was high. There was no significant difference between the intraobsever study (two repeated measurements) and the interobserver study (two investigators), indicating the reproducibility of the method independent of the investigator.
Conclusion
In conclusion, the periacetabular bone density measurement as conducted in this CT study is a new reproducible method for in vivo evaluation of cortical and cancellous pelvic bone after cemented and uncemented acetabular cup implantation. In vivo CT measurements will allow a thorough assessment of periacetabular stress-shielding phenomena.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Compared with numerous investigations of femoral bone stress shielding in total hip arthroplasty (THA), little is known about the periprosthetic pelvic bone after press-fit cup implantation, and there are no data available concerning bone remodeling after cemented cup fixation.
Periprosthetic bone loss is a common problem of THA. Loss of periprosthetic bone mineral density can compromise the outcome of hip arthroplasty and may predispose to loosening and migration of the prosthesis, periprosthetic fracture, and problems during revision arthroplasty [2, 6].
Periacetabular bone density (BD) changes after THA have been evaluated in vivo after press-fit cup implantation using conventional dual X-ray absorptiometry (DXA) [20, 22, 26]. In the presence of cement, no reliable measurements are obtained with DXA [15, 18].
A distinctly better assessment of the bone structures surrounding the prosthesis can be achieved using sectional views generated by CT by virtue of the higher resolution [5] allowing a separate evaluation of cortical and cancellous bone in vivo.
The objective of the present study was to evaluate the reproducibility of BD values for manual segmentation of periacetabular cortical and cancellous bone after cemented and uncemented cup implantation using CT in vivo.
Patients and methods
To evaluate the reproducibility of our newly designed method, we conducted inter- and intraobsever pilot studies. Such investigations are usually analysed inappropriately, notably by using correlation coefficients. For this study, an alternative approach, based on Bland and Altman [1], was used to assess the agreement and reproducibility of our method.
Forty hips (40 patients) with osteoarthritis of the hip joint were operated on by one surgeon. Twenty patients (group 1; 12 men and 8 women; average age 58.38 years, range 39–65 years) received an uncemented total hip prosthesis with a pure titanium hemispherical press-fit acetabular component, an alumina-alumina pairing, and a tapered stem (Cerafit, Ceraver Osteal, Paris, France). The other 20 patients (group 2; 8 men and 12 women, average age 76.6 years, range 73–90 years) received a cemented polyethylene cup (ZCA, Zimmer, USA) with polyethylene-alumina pairing and a cemented stem (Heritage, Zimmer, USA). CT examinations were performed within the first 12 days after surgery. The study was approved by the local ethics committee. All patients signed an informed consent sheet.
The patient was placed in a supine position. On the frontal scout images, pelvic rotation within the axial plane was assessed by analysing the morphology of the obturator foramen and the alignment between the symphysis pubis and the lumbar spinous processes. For future follow-up examinations, the patients were repositioned until the position of the pelvis matched the postoperative analysis.
Sequence CT examinations (Somatom Plus 4, Siemens, Erlangen, Germany) were performed. A standardized scan mode was used with 140 kV, 206 mA, extended CT scale, field of view of 150×150 mm, slice thickness 2 mm, table feed (distance between two scans) 5 mm, start 30 mm above the cup to the lower limp of the cup.
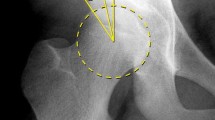
For this study, cancellous and cortical bone of a CT scan taken 10 mm cranial to the cup (Fig. 1, Fig. 2) and one CT scan taken at the level of the cup (divided into a dorsal and a ventral region by drawing a horizontal line through the centre of the cup) was evaluated (Fig. 1, Fig. 3). After segmentation of cancellous and cortical bone, Hounsfield unit (HU) values were assigned automatically to the defined bone portion. The elaboration of data was performed with a special software tool (CAPPA_postOP, CAS Innovations AG, Erlangen, Germany).
CT scans of 20 patients were analyzed for each group by two observers separately (interobserver) and by one observer (intraobserver) again after an interval of 2 weeks based on HU. The agreement between the two raters (interobserver analysis) and between two repeated measurements (intraobserver analysis) was evaluated according to Bland and Altman [1]. The plot of difference between the two observers against their mean allows the investigation of any possible relationship between the measurement error and the true value. We do not know the true value, and the mean of the two measurements is the best estimate we have. In addition, we evaluated the correlation coefficient (Pearson) for all measurements.
All statistical tests were two-sided. The significance level was set at α=0.05. Calculations were made using SPSS Version 10 (Chicago, USA).
Results
The agreement and reproducibility of manual segmentation for the evaluation of cortical and cancellous pelvic bone was high in both the intra- and interobserver study for uncemented as well as cemented acetabular fixation cranial, ventral and dorsal to the cup.
The mean bone density, the mean difference between the two measurements, the measured interval (limits of agreement, ±1.96 SD) between the two measurements (intraobsever) and between two observers (interobserver), the standard deviation, and the correlation coefficient are given in Tables 1 and 2.
The measured interval is described by Bland and Altman [1] as ‘limits of agreement’. How far apart measurements can be without making reproducibility of the method unacceptable is a matter of judgement [1]. We defined in advance that a difference of the measured interval should not exceed ±2 SD of the mean BD to consider the method reproducible.
For Fig. 4 (dorsal sector, uncemented cup, cortical bone, interobserver study), observer 1 may be up to 24.03 HU above or 19.37 HU below observer 2. This is acceptable for our purposes considering that the difference is within ±2 SD of the mean BD of 567.7 HU. The plot of difference against mean allows us to investigate any possible relationship between the measurement error and the true value. The true value remains unknown, and the mean of the two measurements is the best we have. In this case, the mean difference between the two observers is 2.34 HU.
Bland and Altman diagram of interobserver pilot study, press-fit cup, cortical bone, dorsal. The average of the two measurements by the two raters is plotted against the difference between the two measurements. The dashed-dotted line represents the mean value of all differences (+2.34 HU) between the two raters and the dotted line indicates the 95% limits of agreement
As shown in Tables1 and 2, the results of our measurements were quite similar for intra- and interobserver studies of all evaluated sectors for both cortical and cancellous bone of cemented and uncemented cups. Figure 5 displays a representative selection of our results.
Discussion
The etiology of bone loss adjacent to an implant is multifactorial and includes age-related changes, stress shielding [7, 8, 25], osteolysis [9, 13, 23], micromotion [14], inadequate cementing technique and thermal necrosis due to cement polymerisation [8], false orientation of the endoprosthesis [19].
Periprosthetic bone loss after THA may compromise the long-term clinical outcome of the prosthesis. Bone loss has in the past been assessed by serial plain radiographs, DXA measurements, and finite element studies. Especially for the periacetabular bone, the results are conflicting [3, 7].
Considerable errors arise from the analysis of sequential radiographs. Nonuniformity of exposure, variations in the intensity of the radiation field, target distance and variations in femoral rotation led to significant errors in quantitative densitometric evaluation [16].
DXA measurements are only capable of investigating the implant in the anteroposterior (2D measurements) view. DXA is technically unable to distinguish between cortical and cancellous bone surrounding the implant and is limited due to low resolution [4, 24]. Especially for the periacetabular region surrounding the cup, the measured regions of interest are large, and therefore accuracy as well as the spatial relationship of elaborated data are poor [22, 26]. In the presence of cement, no reliable DXA measurements are obtained [18].
While the advantages of CT-assisted osteodensitometry over DXA analysis concerning high resolution and accuracy are obvious, the disadvantage of comparatively high radiation has to be mentioned. CT images are degraded by metal artifacts which generally cause a systematic error in the measurement of BD without an increase in the variability of measurements [18, 21].
Finite element analysis in combination with bone remodeling theories has tried to predict density distribution after THA, but such theoretical models are never able to consider all relevant parameters involved in the process of periacetabular stress shielding after THA. This explains the conflicting results of finite element analysis presented by different authors. While Huiskes et al. [10, 11, 12] observed load transfer to the peripheral bone cephaled to the acetabulum and a decreased stress distribution to the central bone, Levenston et al. [17] saw little change to the BMD of the ilium.
To evaluate the reproducibility and accuracy of the presented method, we conducted an inter- and intraobserver pilot study. Such investigations are usually analysed inappropriately, notably by using the correlation coefficient only [27]. The correlation coefficient measures the strength of a relationship between two variables, not the agreement between them, thus the test of significance may show that the measurements relate, but this is irrelevant to the question of agreement. Data which are in poor agreement can produce quite high correlation [1].
For this study, in addition to the correlation coefficient an alternative approach, based on Bland and Altman [1], was used to assess the agreement and reproducibility of our method. It is most unlikely that the two observers will agree exactly, by giving identical results for all 20 CT scans measured for each group. We wanted to know how much one observer is likely to differ from the other. The plot of difference between the two observers against their mean allows the investigation of any possible relationship between the measurement error and the true value.
We were able to demonstrate sufficient agreement for the intra- and interobsever study for cortical and cancellous bone for both cemented and uncemented cups to consider our method accurate and reproducible for all measured parameters.
CT imaging presents a good differentiation between cortical and cancellous bone, cancellous bone and the implant, and between cancellous bone and cement. This newly designed CT-assisted method aims to quantify overall, cortical and cancellous pelvic bone at the acetabular dome as well as ventral and dorsal to the cup.
By analysing the BD changes with CT-assisted osteodensitometry, a precise and differentiated statement of the in vivo success of an implant is possible. We will be able to distinguish the real distribution of bone-load and stress-shielding phenomena of the pelvis and indirectly the quality of fixation and pattern of loosening after cemented and uncemented cup implantation in vivo. Further improvements will be achieved with artifact reduction by means of image reconstruction methods from raw data. We hope that these artifact-reduced images will provide additional information concerning the bone-implant interface area.
Ultimately, the presented method should be capable of demonstrating the impact of cup positioning, subchondral bone removal, different cup designs and materials on stress transfer mechanisms of the ilium after cup insertion and on the long-term results of the implant. Investigations with this method will show if any of the predicted results of computer modeling techniques and DXA around the cup are precise.
References
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Engh CA, Massin P, Suthers KE (1990) Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop 257:107–128
Engh CA, McGovern TF, Bobyn JD, Harris WH (1992) A quantitative evaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. J Bone Joint Surg Am 74:1009–1020
Engh CA, McGovern TF, Schmidt LM (1993) Roentgenographic densitometry of bone adjacent to a femoral prosthesis. Clin Orthop 292:177–190
Gluer CC, Faulkner KG, Estilo MJ, Engelke K, Rosin J, Genant HK (1993) Quality assurance for bone densitometry research studies: concept and impact. Osteoporos Int 3:227–235
Gruen TA, McNeice GM, Amstutz HC (1979) ‘Modes of failure’ of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141:17–27
Harris WH (1992) The first 32 years of total hip arthroplasty. One surgeon’s perspective. Clin Orthop 274:6–11
Harris WH (1992) Will stress shielding limit the longevity of cemented femoral components of total hip replacement? Clin Orthop 274:120–123
Harris WH (1994) Osteolysis and particle disease in hip replacement. A review. Acta Orthop Scand 65:113–123
Huiskes R (1987) Finite element analysis of acetabular reconstruction. Noncemented threaded cups. Acta Orthop Scand 58:620–625
Huiskes R, Weinans H, Dalstra M (1989) Adaptive bone remodeling and biomechanical design considerations for noncemented total hip arthroplasty. Orthopedics 12:1255–1267
Huiskes R, Weinans H, Rietbergen B van (1992) The relationship between stress shielding and bone resorption around total hip stems and the effects of flexible materials. Clin Orthop 274:124–134
Jasty M, Bragdon C, Jiranek W, Chandler H, Maloney W, Harris WH (1994) Etiology of osteolysis around porous-coated cementless total hip arthroplasties. Clin Orthop 308:111–126
Karrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J (1997) Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop 344:94–110
Kiratli BJ, Checovich MM, McBeath AA, Wilson MA, Heiner JP (1996) Measurement of bone mineral density by dual-energy x-ray absorptiometry in patients with the Wisconsin hip, an uncemented femoral stem. J Arthroplasty 11:184–193
Kroger H, Venesmaa P, Jurvelin J, Miettinen H, Suomalainen O, Alhava E (1998) Bone density at the proximal femur after total hip arthroplasty. Clin Orthop 352:66–74
Levenston ME, Beaupre GS, Schurman DJ, Carter DR (1993) Computer simulations of stress-related bone remodeling around noncemented acetabular components. J Arthroplasty 8:595–605
Markel MD, Gottsauner-Wolf F, Bogdanske JJ, Wahner HW, Chao EY (1993) Dual energy x-ray absorptiometry of implanted femora after cemented and press-fit total hip arthroplasty in a canine model. J Orthop Res 11:452–456
Pellicci PM, Salvati EA, Robinson HJ (1979) Mechanical failures in total hip replacement requiring reoperation. J Bone Joint Surg Am 61:28–36
Reiter A, Sabo D, Simank HG, Buchner T, Seidel M, Lukoschek M (1997) Periprosthetic mineral density in cement-free hip replacement arthroplasty (in German). Z Orthop 135:499–504
Robertson DD, Magid D, Poss R, Fishman EK, Brooker AF, Sledge CB (1989) Enhanced computed tomographic techniques for the evaluation of total hip arthroplasty. J Arthroplasty 4:271–276
Sabo D, Reiter A, Simank HG, Thomsen M, Lukoschek M, Ewerbeck V (1998) Periprosthetic mineralization around cementless total hip endoprosthesis: longitudinal study and cross-sectional study on titanium threaded acetabular cup and cementless Spotorno stem with DEXA. Calcif Tissue Int 62:177–182
Santavirta S, Hoikka V, Eskola A, Konttinen YT, Paavilainen T, Tallroth K (1990) Aggressive granulomatous lesions in cementless total hip arthroplasty. J Bone Joint Surg Br 72:980–984
Schmidt R, Freund J, Hirschfelder H, Pitto RP (2000) Osteodensitometry in uncemented total hip arthroplasty using computer tomography. Biomed Tech (Berl) 45:70–74
Schmidt R, Muller L, Kress A, Hirschfelder H, Aplas A, Pitto RP (2002) A computed tomography assessment of femoral and acetabular bone changes after total hip arthroplasty. Int Orthop 26:299–302
Wilkinson JM, Peel NF, Elson RA, Stockley I, Eastell R (2001) Measuring bone mineral density of the pelvis and proximal femur after total hip arthroplasty. J Bone Joint Surg Br 83:283–288
Wright JM, Pellicci PM, Salvati EA, Ghelman B, Roberts MM, Koh JL (2001) Bone density adjacent to press-fit acetabular components. A prospective analysis with quantitative computed tomography. J Bone Joint Surg Am 83:529–536
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmidt, R., Pitto, R.P., Kress, A. et al. Inter- and intraobserver assessment of periacetabular osteodensitometry after cemented and uncemented total hip arthroplasty using computed tomography. Arch Orthop Trauma Surg 125, 291–297 (2005). https://doi.org/10.1007/s00402-005-0812-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-005-0812-8