Abstract
Introduction
We developed an experimental model in sheep femora to evaluate the process of cortical allograft incorporation.
Materials and methods
Twenty-four sheep were divided into four groups according to the various treatments of cortical allografts as follows: fresh, frozen, autoclaved, and frozen with perforation. Periodical radiographic and histological evaluations were performed for each group.
Results
Perforated frozen allograft proved to be superior radiographically in the first stage to fresh, frozen, and autoclaved forms. Revascularization was demonstrated by both Spalteholz’s technique and histological examination. Histological analysis also showed creeping substitution, from the host bone to the allograft, which increased the reabsorption to facilitate new bone penetration, including endochondral ossification at the host-graft interface.
Conclusion
We believe that endochondral ossification is probably a biological event occurring routinely during the bone healing process and that the processes of incorporation of variously treated cortical allografts differ only at the early phase of implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone is one of the most commonly transplanted tissues of the human body. Contemporary skeletal reconstruction incorporates bone transfers in the treatment of osseous discontinuity, defects subsequent to congenital malformation, traumatic injuries, tumor surgery, and in failures of osteosynthesis [4, 5, 8]. Bone grafts can be applied in contour augmentation and for strengthening and stabilization in various conditions. The osseous healing process is dynamic and unique, for the skeleton is one of the few organ systems capable of regeneration without the formation of scar tissue [2]. The current understanding of the process of bone allograft integration is mainly based on cell biology [3, 7, 12, 13], biomechanical studies [3, 9], immunobiological approach [15, 16, 17], and clinical applications [4, 5, 8, 10].
Previous clinical and experimental studies revealed that the incorporation of cortical bone grafts proceeds very slowly in comparison with that of cancellous bone grafts [4, 5, 12, 15, 16]. According to these studies, a large cortical allograft is extremely slowly remodeled by host bone, though osseous union at the host-graft interface occurred within a few weeks. Because the osteoblast progenitor cells and vessels, originating from host bone, are provided to the allograft extremely slowly, microfractures of the allograft cannot be healed adequately and result in gradual weakening of graft [3, 12]. These findings explain the high rate of clinical complications in massive bone allograft surgery [4, 5, 8]. The way to minimize such bone complications is to enhance the allograft incorporation. Limited understanding of the basic biological and biomechanical principles of bone graft repair and remodeling processes has made it difficult to improve the success rate of bone allograft surgery.
The incorporation of a bone graft is the result of creeping and substitutional events that reduce the grafted bone and replace it by newly formed bone from the host bone. We developed a sheep model of cortical allografts in order to compare the incorporation processes in the various conditions of cortical allografts. The current study focused on radiographic and histological processes during the incorporation of grafted cortical bone.
Materials and methods
We performed cortical bone grafts on the left femora in 24 sheep aged 4 months with an average weight of 20–25 kg at the time of operation. The study was approved by the Ethics Committee for Animal Research. All animal care was in accordance with our institutions’ Animal Laboratory Committee Guidelines and under the supervision of a veterinarian team. The 24 sheep were evenly divided into four groups according to the types of bone grafts in the following manner: fresh intercalary autograft, 6 sheep (group 1); frozen intercalary allograft, 6 sheep (group 2); autoclaved intercalary allograft, 6 sheep (group 3), and frozen intercalary allograft with four cortical perforations, 6 sheep (group 4).
The allografts were obtained under sterile conditions from donor animals. The left femur was extracted in the operating room, and the soft tissues and periosteum were removed. The bone was cut with a saw to obtain a diaphyseal cylinder 3 cm in length, which was stored according to the group.
In the case of the fresh grafts, these were extracted from the animal, cleaned of the soft tissues and periosteum, and inserted again in the same animal upside-down. In the groups with frozen allografts, the grafts were extracted and stored in two sterile bags. In one group, a 5 mm drill was used to make four perforations which crossed the two cortices of the graft. They were then kept in a freezer at –20°C for a minimum of 6 weeks. Finally, six grafts were autoclaved, at 134°C, for 8 min, in a Barnstead benchtop sterilizer (Bearnstead, Dubuque, IA, USA) and stored under sterile conditions until use.
Bone graft protocol
Intravenous atropine, tiobarbital and fentanyl were given at induction at a dosage of 0.5 mg/kg, 12 mg/kg, and 0.0015 mg/kg, respectively. General anesthesia consisted of tiobarbital (10 mg/kg) and fentanyl (0.0015 mg/kg) administered intravenously.
We performed a lateral skin incision on the left femur. After exposure of the femur by splitting between the vastus lateralis muscle and biceps femoris muscle, a 3 cm length of cylindrical diaphyseal bone was resected. The four types of variously treated cortical bone were grafted after modeling as fitted to defects, and then stably fixed by intramedullary nails.
The sheep were killed with an overdose of pentobarbital (500 mg) and potassium chloride (50 mEq) administered intravenously, and the operated femora were extracted for analysis.
Radiographic study
To assess osseous formation around the grafted bone, radiographs were taken and evaluated on the day of surgery and 2 months, 4 months, and 6 months after surgery according to a previously established scoring system (Table 1).
Histological studies
Once the animal had been killed, we extracted the femur and placed it in 10% buffered formaldehyde. Using a saw, we cut the femur in a longitudinal direction. After decalcification of all the specimens in EDTA for 2–3 weeks, which was confirmed radiolographically, we proceeded to place them in paraffin and cut them into 4-μm pieces. The site for histological evaluation was grafted cortical bone with both proximal and distal areas of host bone. Sections were stained with hematoxylin and eosin (H&E) and Masson’s trichrome.
To study the revascularization after bone grafting, Berlin blue solution was injected through the femoral artery before killing to perform the Spalteholz technique.
Statistical analysis
For comparison of the radiographic score in the different treatments, the nonparametric Kruskall-Wallis test was used, followed by the Mann-Whitney U-test. To study the evolution of the radiographic score throughout time, the Friedman test was used, followed by the Wilcoxon test. The p values were considered significant when less than 0.05. All the statistical analyses were performed using SPSS 9.0 for Windows.
Results
All 24 sheep survived and showed a good tolerance for experiments. The sheep showed a normal capacity of the operated leg at daily exercise. No wound problems, fractures, infections, or other problems were encountered.
Radiographic evaluation
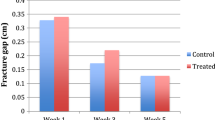
Bone formation and host-graft union could be seen on monitoring radiographs. Periosteal bone formation was predominant at 2 months after surgery; however, subsequent union and medullary consolidation were observed at both 4 and 6 months after surgery (Fig. 1). Scoring values of each group at the four periodical evaluations were obtained. When comparing these values at 2 months after surgery, the differences in group 4 to group 3 (p<0.01), group 4 to group 1, and group 4 to group 2 (p<0.05) were evaluated as significant. However, there was no evident difference in any comparison thereafter (Fig. 2).
Although the differences between day of surgery to 2 months and 2 to 4 months after surgery were both significant (p<0.05), those between 4 and 6 months were not significant in any group at the time course evaluations (Fig. 3).
Histological evaluation
At the host-graft interface, new bone formation was shown as invading into the irregular surface and resorbed cavities of the allografts, though these processes were delayed in group 3 (autoclaved allografts). Vessels were always involved in the new bone formation. The new bone formation was seen at the surface area of the allograft (Fig. 4a). The pattern of endochondral ossification was also seen, which was characterized by new bone formation just beside cartilage matrices, at both the intracortical and endomedullary gap. Osteoclastic activity was apparently observed around newly formed bone areas (Fig. 4b). At the periosteal surfaces of the host-graft interface, the pattern of intramembranous ossification was predominant, and the process of ossification from fibrous structures was evident (Fig. 4c,d). Those erosive areas and resorbed cavities were filled with new bone formation, together with the vascular invasion of the internal areas of the cortical allografts (Fig. 4e).
At the host-graft interface, new bone formation invaded into erosive areas and resorbed cavities of the allografts (a, H&E, x60). Osteoclastic bone resorption was seen around newly formed bone area (b, H&E, x300). At the periosteal surfaces of the host-graft interface, the pattern of intramembranous ossification was predominant (c, Masson’s trichrome, x60), and the process of ossification from fibrous structures was evident (d, Masson’s trichrome, x300). Those erosive areas and resorbed cavities were filled with new bone formation, together with the vascular invasion of the internal areas of the cortical allografts (e, H&E, x60)
The processes of revascularization of the host-graft interface after bone grafting are shown in Fig. 5. Apparent vascular anastomoses between periosteal and endomedullary vessels, penetrating the cortical bone, and reticular vascular provision within the allografts were demonstrated by Spalteholz’s technique (Fig. 5a). Endomedullary vascular system was repaired, and a minute vascular plexus was observed at irregular lacunar resorption pit areas on the internal surface of the allograft (Fig. 5b). These irregular resorption pit areas were correlated to those in the histologic picture (Fig. 4b).
Revascularization was assessed by Spalteholz’s technique. Apparent vascular anastomoses (arrow) between periosteal and endomedullary vessels, penetrating the cortical structure of the allograft, and reticular vascular provision within the grafted bone were demonstrated (a). Endomedullary vascular system was successfully repaired, and a minute vascular plexus was observed at the irregular lacunar resorption pit areas, which were formed by osteoclasts, on the internal surface of the allograft (b)
Discussion
The results of the current study show that, by means of a simple and reproducible surgical procedure, radiographic and histological evaluations of the incorporation of cortical bone allografts can be done in the model of sheep femora.
The factors that affect the main events of bone graft incorporation are host-graft union, revascularization, and new bone formation [12]. Although relatively high rates of nonunion have been reported in the clinical field, all of the cortical allografts were evaluated as united with host bone in our series. Periodical radiographs showed an abundant periosteal bridging callus over the allografts. Histological examination also revealed that new bone invaded into erosive areas and resorbed cavities at the periosteal and endosteal surfaces of the allografts, though these vascular and new bone invasions were seen only at the superficial area of the intercortical region. The union stage seemed not to correlate with the amount of endosteal bone formation but correlated well with the amount of periosteal callus formation.
As for revascularization and new bone formation, in most of the previously published literature, fresh autografts showed superior results to allografts in terms of qualitative histological findings and radiographic evaluation [12, 17]. However, a certain report described no statistical difference in histomorphometrical assessment between autograft and allograft, though it involved a flat bone (ilium) with developmental heterogeneity [1]. In the current study, radiographic scoring assessment showed that perforated frozen allograft was significantly superior to fresh, frozen, and also autoclaved allografts at just 2 months after surgery. Frozen allograft has osteoconductive but not osteoinductive potency despite its better mechanical strength than fresh or autoclaved cortical allograft at the time of implantation [9]. The disadvantage of autoclaved allograft may be explained by the fact that revascularization and bone formation tended to decrease as the temperature of the heat treatment rose [11]. These results were probably caused by degeneration of the cytokines associated with blood vessel and bone formation, such as transforming growth factor beta (TGF-β) and bone morphogenic protein. In addition, vascular invasion into the intertrabecular area was prevented by coagulation necrosis of the bone marrow, which was considered to delay bone conduction. On the other hand, the perforated frozen allograft tended to be superior to frozen allograft radiographically only in the first stage. The results might have been caused by constituted avenues for graft invasion by vessels, other host cells and enhanced incorporation by the mechanism of osteoconduction, although we could not show evidence of those processes. Radiographic scoring assessment also showed that the differences between the day of surgery to 2 months and 2 to 4 months after surgery were both significant, but those between 4 and 6 months were not significant in any group in the time course evaluations. These two results may indicate that the initial response of host bone to the graft was different between fresh allograft and treated allograft at an early phase of incorporation. Virolainen et al. described that the differences between autograft and allograft had markedly diminished by 8 weeks after surgery in histomorphological, biomechanical, and biochemical evaluations [15]. In comparison with the incorporation processes in variously treated cortical allografts, we concluded that the radiographically significant difference was found only at 2 months after surgery and diminished thereafter.
The comparatively earlier revascularization in fresh autografts is thought to be due to the production of vascular anastomoses at the interface between graft and host bone [14]. The delayed revascularization of fresh allografts is possibly due to early immune responses. It is likely that frozen allografts are revascularized not by anastomoses but by the invasion of vessels from the host bone [6, 14]. In our study, however, the vascular anastomoses were observed at the periosteal host-graft interface, and vascular invasions were also demonstrated within both the intramedullary space and intracortical area of all types of allografts.
The earlier new bone formation in fresh autografts is the result of the grafted bone providing its own progenitor cells at the initial stage [12]. The later increase in new bone formation produced by frozen allografts is probably due to their lower immunogenicity and osteoconduction occurring from the host bed [6, 18].
Regarding histological processes of bone incorporation, Virolainen et al. described that cortical allografts showed three different healing mechanisms with considerable overlap [15]. In most instances, however, the allograft seemed partially reabsorbed, and the remaining nonvascularized graft was enwrapped by a small amount of new bone. These findings are quite different from the healing pattern observed in cancellous allografts, which involved a progressive creeping substitution by means of vascular channels and resorbed cavities that were well covered by a layer of new bone. These differences can probably be explained by the structural difference between the cortical and the cancellous bone. The porous structures of the cancellous bone can provide constituted avenues for host-derived vessels and other mesenchymal cells, and then enhanced incorporation by the mechanism of osteoconduction. Several clinical and experimental studies have proved that perforated tracts of the cortical allografts were obviously enhanced by new bone formation [3, 10]. Since perforation of the cortical allograft raises the risk of fracture, we should have another option to enhance bone incorporation of the graft. Enneking and Campanacci described that when the autogenous graft was in contact with the allograft, there was not only intense new bone formation on the surface of the graft but also more extensive internal repair in the underlying cortex of the allograft [5]. Our histological examination showed the pattern of endochondral ossification, although these findings have not been observed in the other graft healing model [17]. Only one case presented with endochondral ossification at the cortical-cortical junction of retrieved allograft [5]. Virolainen et al. suggested that the microenvironment and the presence of other growth factors at the repair site, together with TGF-β, regulated the osteogenic and chondrogenic differentiation programs of the mesenchymal cells during skeletal repair [17]. Though it is now impossible to show whether endochondral ossification is the result of a biological or biomechanical event, we believe that this is probably a biological one occurring routinely during the bone healing process.
In conclusion, our study showed no significant difference in the processes of bone incorporation between four groups of variously treated cortical allografts except at the early phase after implantation. These results may indicate that any form of treatment for cortical allografts provides good results regarding bone incorporation, though clinical experience questions the use of perforated cortical allograft because of its risk of fracture. It is probably important to add supplementary autogenous cancellous bone grafts at the site of a cortical allograft in order to enhance cortical bone incorporation in clinical applications.
References
Anderson MLC, Dhert WJA, Bruijn JD de, Dalmeijer RAJ, Leenders H, Blitterswijk CA van, Verbout AJ (1999) Critical size defect in the goat’s os ilium. Clin Orthop 364:231–239
DeLacure MD (1994) Physiology of bone healing and bone grafts. Otolaryngol Clin North Am 27:859–873
Delloye C, Simon P, Nyssen-Behets C, Banse X, Bresler F, Schmitt D (2002) Perforations of cortical bone allografts improve their incorporation. Clin Orthop 396:240–247
Enneking WF, Mindell ER (1991) Observations on massive retrieved human allografts. J Bone Joint Surg Am 73:1123–1142
Enneking WF, Campanacci DA (2001) Retrieved human allografts. J Bone Joint Surg Am 83:971–986
Friedlaender GE (1983) Immune responses to osteochondral allografts: current knowledge and future directions. Clin Orthop 174:58–68
Goldberg VM, Stevenson S (1987) Natural history of autografts and allografts. Clin Orthop 225:7–16
Mankin HJ, Doppelt S, Tomford W (1983) Clinical experience with allograft transplantation. Clin Orthop 174:69–86
Moreno J, Forriol F (2002) Effects of preservation on the mechanical strength and chemical composition of cortical bone: an experimental study in sheep femora. Biomaterials 23:2615–2619
San-Julian M, Canadell J (1998) Fractures of allografts used in limb preserving operations. Int Orthop 22:32–36
Shimizu K, Masumi S, Yano H, Fukunaga T, Ikebe S, Shin S (1999) Revascularization and new bone formation in heat-treated bone grafts. Arch Orthop Trauma Surg 119:57–61
Stevenson S, Emery SE, Goldberg VM (1996) Factors affecting bone graft incorporation. Clin Orthop 323:66–74
Stevenson S, Li XQ, Davy DT, Klein L, Goldberg VM (1997) Critical biological determinants of incorporation of non-vascularized cortical bone grafts. J Bone Joint Surg Am 79:1–16
Urist MR (1980) Fundamental and clinical bone physiology. Lippincott Williams&Wilkins, Philadelphia
Virolainen P, Vuorio E, Aro HT (1993) Gene expression at graft-host interfaces of cortical bone allografts and autografts. Clin Orthop 297:144–149
Virolainen P, Perala M, Vuorio E, Aro HT (1995) Expression of matrix genes during incorporation of cancellous bone allografts and autografts. Clin Orthop 317:263–272
Virolainen P, Elima K, Metsaranta M, Aro HT, Vuorio E (1998) Incorporation of cortical bone allografts and autografts in rats. Expression pattern of mRNAs for the TGF-bs. Acta Orthop Scand 69:537–544
Yano H, Masumi S, Fukunaga T, Ikebe S (1993) Quantitative analysis of revascularization and new bone formation in experimental bone grafts. Int Orthop 17:109–112
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taira, H., Moreno, J., Ripalda, P. et al. Radiological and histological analysis of cortical allografts: an experimental study in sheep femora. Arch Orthop Trauma Surg 124, 320–325 (2004). https://doi.org/10.1007/s00402-004-0653-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-004-0653-x