Abstract
Introduction
The aim of an intraosseous application of electromagnetic alternating fields is to speed up both the regeneration of osteonecroses and bone regeneration. In clinical studies, the efficiency of the technique could be successfully proven by using a transducer coil. The advantage of the traditional technique was the variety of its applications in connection with various osteosynthesis systems; the disadvantage was a possible failure of the contacting leads and the resulting functional breakdown.
Materials and methods
A newly developed BISS screw (bipolar induction screw system) with integrated coil and electrodes was compared to a standard cannulated screw used in the traditional technique. The strength of BISS screws (n=6) and of cannulated screws (n=6) was evaluated in comparative biomechanical tests. Examinations consisted of torsional and static and dynamic cantilever tests. All screws were made of the same material (TiAl6V4) and had identical outer dimensions.
Results
No significantly lower strengths could be observed when we compared BISS screws with cannulated screws. The BISS screws even showed significantly higher mechanical values due to a reinforcing effect by the attached electrode.
Conclusion
In the modified concept of the new BISS screw, both coil and electrodes are housed in only one cannulated screw. No negative effects concerning mechanical strength and durability were associated with the new screw concept. This provides for a simpler implantation and makes removal easier, while the risk of a cable tear is avoided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The technique of magnetically induced electro-osteostimulation provides osteoinductive functional stimuli via electromagnetic alternating fields. The effectiveness of this method was shown in vitro and in animal experiments subsequent to examining the electrical properties of living and dead bone tissue [1]. Clinical studies were able to show the effects of electromagnetic alternating fields in disturbed healing of bone fractures [22] and in necrosis of the head of the femur [19].
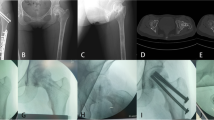
The disadvantages of the traditional principle (Fig. 1) were:
-
fatigue failure of the connecting wires as well as mechanical disconnections at the contact elements due to friction against the bordering tissue could be observed during clinical application;
-
additional implants (separate transducer system with cables) were necessary and
-
a minimum of two osteosynthesis parts were required which served as electrodes (e.g. two screws).
Thus, improvement of the technique was needed to achieve the following objectives:
-
reduction of potential functional defects, caused by the above-mentioned failures such as cable tears (Fig. 1);
-
simplified application and removal of the implant;
-
a more consistent arrangement of electrodes to each other in order to guarantee a correct and reproducible handling of the system.
By inserting both electrodes and the induction coil into a single screw (as a one-screw system), it is possible to realize the above-mentioned requirements by what is called the bipolar induction screw system (BISS).
The remaining potential risks of using the BISS screw include cartilage perforation or dislocation of the flattened part of the femoral head as known from core decompression or during implantation of fibular grafts.
Another limitation using the BISS screw is that MRI is not recommended until the BISS screw is removed (after 12 weeks). This has also been advised for the former principle of the electro-inducible system.
The aim of the study was to prove the mechanical stability of the BISS system. In order to determine the mechanical strength of bipolar induction screws and of electrical isolation of the adhesive film between the tip and shaft of the screw, static and dynamic bending tests were carried out. We also determined the static torsion shearing strength of the adhesion film.
Materials and methods
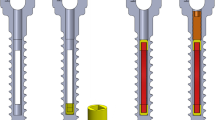
The basic body of a BISS screw is a cannulated spongiosa screw (titanium basic alloy, TiAl6V4), with a transducer coil being inserted into its hollow space. The cannulated screw (including screw head, shaft and thread face) is used as the first electrode. Subsequent to implanting the coil, the tip of the screw (without thread) is adapted as the second electrode, using an adhesive which is electrically isolating (epoxy resin, named Hysol, Dexter Co., USA) into the other part of the screw (Fig. 2). The BISS screw (GEOT, Germany) is available in different lengths and diameters. A size suitable for the treatment of necrosis of the femoral head was tested in the examinations relevant for this study. In a control group, cannulated spongiosa screws—the body of the BISS screws—with a length of 80 mm, an external diameter of 6.5 mm, a (tapping) spongiosa thread length of 44 mm, and a core diameter of 5 mm (manufactured by DePuy, UK) were used.
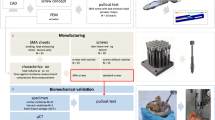
The static bending tests were carried out on six BISS screws and six cannulated spongiosa screws (hollow core screws; HS) using a universal testing machine (Wolpert TZZ 707, load cell 50 kN) (Fig. 3). The screws were set in a drill chuck, with the screw’s longitudinal axis orthogonally adjusted to the inspection stamp (radius 3 mm) and strain direction. The load of the bipolar induction screws was fixed to the end of the screw, with a free clamping length of 25.5 mm. In order to avoid a localised, uni-sided, plastic deformation of the thin-walled end of the spongiosa screws, a journal of 13 mm length was fitted into the end of the screw to allow for a more even introduction of force. The strain was exerted at the same free clamping length of 25.5 mm at a test velocity of 5 mm/min until the extension maximum was reached. During the test a force-deformation diagram was recorded.
For the dynamic free bending tests we also used six cannulated (HS) and six BISS screws. The dynamic bending tests were carried out in a servo-hydraulic test machine (Roell Amsler 2151, load cell 20 kN) at room temperature in air. The test set-up was identical to that for the static bending tests. However, the load on the bipolar induction screws was applied to the end of the screw in a pulsating manner, with a test frequency of 5 Hz. The test was continued until the level of endurance determined prior to the test was reached or the screw burst. During the test, maximum and minimum loads as well as maximum and minimum lowering of the inspection stamp were recorded. The maximum loads applied were around 400 N, which equals a maximum bending moment of 10.2 Nm. This corresponds to about 50% of the average bending moment obtained during static tests as far as the extension maximum was concerned (20.5 Nm for BISS screws, 18.7 Nm for cannulated screws).
In order to test the effects of the dynamic load on the electric function, the ohmic resistance between tip and shaft of the screw was measured with a digital multimeter (Voltcraft M-4660A, measuring capacity 20 MΩ) prior and subsequent to the test.
The static torsion shearing strength was determined using a universal testing machine (Wolpert TZZ 707, load cell 50 kN) at room temperature. The samples (n=7) were fixed between two drill chucks, one of which was connected with the machine crosshead, the other with a torque detector (Burster 8628, max. torque 100 Nm) and a swing angle provider (Megatron MA 751) (Fig. 3). Apart from that, the specimens were exposed to an axial tension load of 10 N using an universal testing machine. The load on the samples was introduced at an angular velocity of 0.1°/s until the adhesive film came apart. Torsional moment and torsional angle were recorded for the whole test period by using a personal computer.
Biomechanical variables were analyzed statistically by the Wilcoxon test for paired samples with the software SPSS (version 11.5).
Results
All screws were strained during a static bending test until the extension maximum was reached. All samples showed a ductile material behaviour (Fig. 4). During static bending tests there was one case of screw destruction (sample BISS 3), with a bending moment, however, also being reached at a maximum bending moment of 20.7 Nm.
The average bending moment at extension maximum was 20.5±0.9 Nm (range 19.3–21.6) for BISS screws and 18.7±0.6 Nm (range 18.3–19.5) for cannulated screws. For flexural strength the following values were measured: 230±9 N/mm (range 223–245) for BISS screws and 182±6 N/mm (range 174–189) for cannulated screws. The BISS screws thus showed significantly higher values with respect to the bending moment at extension maximum than the cannulated screws (HS) (p<0.05) (Fig. 4). The flexural strength of the BISS series was significantly higher by 26% than the strength of the hollow screws (p<0.001). Both effects are due to the end of the screw being reinforced by the attached electrode.
During dynamic bending load no fatigue-tested specimens without failure were discovered, either for hollow or for BISS screws beyond a maximum bending moment of 9.7 Nm. At a maximum bending moment of 9.7 Nm (maximum load 350 N), fatigue-tested specimens with as well as without ruptures were discovered in both sample groups. With lower bending moments, no ruptures were detected within the applied endurance (Fig. 5: Wöhler’s diagram) in these groups.
The ohmic resistance measured between the tip and shaft of the BISS screws prior and subsequent to the test, for all fatigue-tested specimens without rupture, was above the maximum measuring range of the multimeter used (20 MΩ). With respect to the two BISS screws that broke under a high bending moment, in one case an electrical conductibility between tip and shaft of the screw occurred, with the resistance being 0.53 MΩ subsequent to the occurrence of a fatigue fracture.
In the static torsion test all seven BISS screws examined showed a brittle characteristic of failure at the adhesive film (Fig. 6). A mean moment of failure of 7.64±1.17 Nm was calculated. These torsion moments clearly exceeded those torsion moments to be expected in clinical applications. For example, Ryken et al. state a value of 0.367±0.243 Nm as the insertion moment of bone screws into vertebral bodies [19]. A mean moment of failure of 7.68±0.20 Nm was calculated for the group of control specimens.
Discussion
A variety of biological, joint-preserving, surgical procedures like core decompression, osteotomy, free and vascularized bone grafts have been devised with varying success. Cement filling as another alternative procedure [11] has the disadvantage of additional, thermically induced bone necrosis in the surrounding bone up to 2.8 mm [3, 27]. Core decompression has a low success rate and fails in severe cases (up to 56% [26]).
Bone transplants showed differing results, partially with high percentages of progressive collapse (up to 56%) [10]. The rate of necessary reoperation with a total hip replacement is obviously lower using vascularized fibula than after core decompression [12, 20], but the failure rate of vascularized grafts also reaches 20% after 2 years [12] and 30% after 5 years [24]. Vascularized transplants from the iliac crest showed satisfying clinical results in only some cases after 4.4 years [21]. Therefore, when use of vascularized bone transplants like iliac crest or fibula is being considered, the high co-morbidity at the donor site must be seen in relation to the benefits [5, 25].
In essence, no ideal method showing low co-morbidity is currently known for the treatment of avascular necrosis of the femoral head.
Depending on elastic deformation, electrical phenomena play an important role in the regeneration and remodelling of bones [6, 9]. Based on cell culture conditions, it was possible to show that electromagnetic fields influence differentiation, metabolism, and synthesis performance of human cells [16]. The frequency and strength of the electromagnetic field are, in this context, of essential importance [15, 23]. It is a well-known fact that in most cases, sinusoidal fields with low frequency induce osteogenetic reparative cellular mechanisms [18], with fields below 10 µV/cm for 1 h a day being sufficient to increase the bone mass.
Electrical potential differences in the bone can—just like with the BISS system—be produced by way of athermic electromagnetic induction at low frequencies. From these results, in a bone with normal blood flow at an alternating current conductance of about 10-3 Ω-1 cm-1, a current conduction of about 1 µA and in the atrophic bone, of about 10-6 to 10-8 Ω-1 cm-1 can occur [1, 13].
The new BISS system is based upon the technical foundations of the electroinduction method introduced by Kraus and Lechner [14] and Ascherl [1] (frequency 20 Hz, magnetic induction 5 mT, actual voltage 700 mV, internal resistance <100 Ω). Also in this context, extracorporeally applied electromagnetic alternating fields create a flow of current intracorporeally in the target tissue by way of the transformer principle. The successful utilisation of this principle in the context of bony tissue requires a reproducible application of the electrodes. By using the newer system, it is possible to reduce the parts to be implanted (Fig. 7), which results in a simpler application method and last but not least in a much easier way of removing the implants.
It was, however, necessary to prove that the new system is sufficiently stable from the biomechanical point of view. While the BISS screws do indeed serve for electro-osteoinduction, they need to withstand the local mechanical load in the bone tissue, e.g. in the femoral neck and head, which comes mainly as a bending force [7]. The well-tried application duration of the electroinduction system used to date is, in clinical application, restricted to 3 months, which means that also when using the BISS system the implant can be removed after this period of time. The results available, from static and dynamic bending tests, show a sufficient bending strength since they are similar to those gained in tests with cannulated screws made of titanium-alloy TiAl6V4. The isolation within the BISS screw, which constitutes one foundation of the electroinductive effect, was not compromised by a dynamic load below the screws’ permanent fatigue limit.
The induction screws are not primarily designed to serve as osteosynthetic stabilisation of a femoral neck fracture but may, in case of a subsequent fracture of the femoral head or neck, theoretically be exposed to loads similar to those after osteosynthesis of a femoral neck fracture of Pauwels type 3 [4, 8]. For this reason the mechanical examination, in particular of the bending load [17], was of essential importance for the clinical use of the system.
The BISS concept thus constitutes a pioneering approach to improve the traditional method of magnetically induced electro-osteoinduction in connection with osteosynthesis implants. The decisive factor, however, will be the correct diagnosis and positioning of the screws to achieve the desired clinical effect, in particular in cases of necroses of the femoral head.
References
Ascherl R (1976) Experimentelle Untersuchungen über den elektrischen Widerstand und den Leitwert am lebenden und toten Knochengewebe unter physiologischen Bedingungen sowie nach pathologischen Veränderungen. Thesis, Technische Universität, Munich
Ascherl R, Walz H, Geißdörfer K, Schmeller M-L, Lechner F, Blümel G (1989) Förderung der Knochenheilung durch extrem niederfrequente elektromagnetische Wechselfelder im Experiment. In: Lechner F (ed) Elektrostimulation und Magnetfeldtherapie: Anwendung, Ergebnisse und Qualitätssicherung. Schattauer, Stuttgart, pp 1–9
Berman AT, Reid JS, Yanicko DR Jr, Sih GC, Zimmerman MR (1984) Thermally induced bone necrosis in rabbits. Relation to implant failure in humans. Clin Orthop 186:284–292
Blair B, Koval KJ, Kummer F, Zuckerman JD (1994) Basicervical fractures of the proximal femur: a biomechanical study of 3 internal fixation techniques. Clin Orthop 306:256–263
Bohay DR, Manoli A (1995) Clawtoe deformity following vascularized fibula graft. Foot Ankle Int 16:607–609
Brighton CT, Friedenberg ZB, Black J, Esterhai L, Mitchell JE, Montique F (1981) Electrically induced osteogenesis: relationship between charge, current density and the amount of bone formed. Clin Orthop 161:122–132
Cristofolini L, Viceconti M, Toni A, Giunti A (1996) Influence of thigh muscles on the axial strains in a proximal femur during early stance in gait. J Biomech 28:617–624
Deneka DA, Simonian PT, Stankewich CJ, Eckert D, Chapman JR, Tencer AF (1997) Biomechanical comparison of internal fixation techniques for the treatment of unstable basicervical femoral neck fractures. J Orthop Trauma 11:337–343
Fukada E, Yasuda J (1957) On the piezoelectric effect of bone. J Physiol Soc Jpn 12:1158–1162
Hasegawa Y, Iwata H, Torii S, Iwase T, Kawamoto K, Iwasada S (1997) Vascularized pedicle bone-grafting for nontraumatic avascular necrosis of the femoral head. A 5- to 11-year follow-up. Arch Orthop Trauma Surg 116:251–258
Hernigou P (1999) Treatment of hip necrosis by sequestrectomy and replacement with bone cement. Acta Orthop Belg 65 [Suppl 1]:89–94
Kane SM, Ward WA, Jordan LC, Guilford WB, Hanley EN Jr (1996) Vascularized fibular grafting compared with core decompression in the treatment of femoral head osteonecrosis. Orthopedics 19:869–872
Kraus W (1984) Magnetfeldtherapie und magnetisch induzierte Elektrostimulation in der Orthopädie. Orthopäde 13:78–92
Kraus W, Lechner F (1972) Die Heilung der Pseudarthrosen und Spontanfrakturen durch strukturbildende elektrodynamische Potentiale. Münch Med Wochenschr 114:1814–1819
Loschinger M, Thumm S, Hammerle H, Rodemann HP (1999) Induction of intracellular calcium oscillations in human skin fibroblast populations by sinusoidal extremely low-frequency magnetic fields (20 Hz, 8 mT) is dependent on the differentiation state of the single cell. Radiat Res 151:195–200
Rodemann HP, Bayreuther K, Pfleiderer G (1989) The differentiation of normal and transformed human fibroblasts in vitro is influenced by electromagnetic fields. Exp Cell Res 182:610–621
Rouleau JP, Blasier RB, Tsai E, Goldstein SA (1994) Cannulated hip screws: a study of fixation integrity, cut-out resistance, and high-cycle bending fatigue performance. J Orthop Trauma 8:293–299
Rubin CT, Donahue HJ, Rubin JE, McLeod KJ (1993) Optimization of electric field parameters for the control of bone remodeling: exploitation of an indigenous mechanism for the prevention of osteopenia. J Bone Miner Res 8 [Suppl 2]:573–581
Ryken TC, Clausen JD, Traynelis VC, Goel VK (1995) Biomechanical analysis of bone mineral density, insertion technique, screw torque, and holding strength of anterior cervical plate screws. J Neurosurg 83:325–329
Scully SP, Aaron RK, Urbaniak JR (1998) Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am 80:1270–1275
Solonen KA, Rindell K, Paavilainen T (1990) Vascularized pedicled bone graft into the femoral head—treatment of aseptic necrosis of the femoral head. Arch Orthop Trauma Surg 109:160–163
Stuermer KM, Schmit-Neuerburg KP (1985) Indications and clinical results of electromagnetically-induced alternating current stimulation of poorly reacting pseudarthroses. Unfallchirurgie 11:197–203
Thumm S, Loschinger M, Glock S, Hammerle H, Rodemann HP (1999) Induction of cAMP-dependent protein kinase A activity in human skin fibroblasts and rat osteoblasts by extremely low-frequency electromagnetic fields. Radiat Environ Biophys 38:195–199
Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA (1995) Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am 77:681–694
Vail TP, Urbaniak JR (1996) Donor-site morbidity with use of vascularized autogenous fibular grafts. J Bone Joint Surg Am 78:204–211
Yoon TR, Song EK, Rowe SM, Park CH (2001) Failure after core decompression in osteonecrosis of the femoral head. Int Orthop 24:316–318
Yun YH, Kim NH, Han DY, Kang ES (1993) An investigation of bone necrosis and healing after cryosurgery, phenol cautery or packing with bone cement of defects in the dog femur. Int Orthop 17:176–183
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mittelmeier, W., Lehner, S., Kraus, W. et al. BISS: concept and biomechanical investigations of a new screw system for electromagnetically induced internal osteostimulation. Arch Orthop Trauma Surg 124, 86–91 (2004). https://doi.org/10.1007/s00402-003-0594-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-003-0594-9