Abstract
Parkinson’s disease primarily affects the central nervous system, but autopsy and small patient studies have revealed autonomic nervous system pathology in most cases. We looked for α-synuclein pathology in routinely acquired biopsies from patients and matched controls. Immunocytochemistry was performed and assessed blind to the clinical diagnoses. One hundred and seventeen gastrointestinal tissue samples from 62 patients, and 161 samples from 161 controls, were examined. Twelve biopsies from seven patients showed accumulation of α-synuclein within mucosal and submucosal nerve fibres, and ganglia, which was more extensive with an antibody to phosphorylated, than with an antibody to non-phosphorylated, α-synuclein. These included gastric, duodenal and colonic biopsies, and were taken up to 8 years prior to the onset of motor symptoms. All patients with positive biopsies had early autonomic symptoms and all controls were negative. This large scale study demonstrates that accumulation of α-synuclein in the gastrointestinal tract is a highly specific finding that could be used to confirm a clinical diagnosis of Parkinson’s disease. We have shown that α-synuclein accumulation occurs prior to the onset of motor symptoms in the upper, as well as the lower gastrointestinal tract, remains present in serial biopsies until the onset of motor symptoms and is predominantly composed of phosphorylated α-synuclein. Accumulation of α-synuclein in the bowel therefore offers an accessible biomarker which allows further study of the early stages of the disease and could be of value in the assessment of disease modifying treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease is one of the most common neurodegenerative disorders affecting the ageing population across the world [11, 31]. Classical features of Parkinson’s disease include tremor, bradykinesia, rigidity and postural instability [24] which are secondary to neuronal degeneration within the central nervous system. In recent years there has been growing interest in the extranigral components of the disease [25], and in particular the involvement of the peripheral autonomic nervous system [9]. A number of autonomic symptoms may occur, including orthostatic hypotension, upper gastrointestinal dysmotility, constipation, urinary symptoms and erectile dysfunction [9, 25], some of which may pre-date the onset of the classical central signs by 10–20 years [1, 41, 42]. Autopsy studies have confirmed the widespread distribution of α-synuclein pathology in the peripheral autonomic nervous system of Parkinson’s disease patients [5, 6], including the gastrointestinal tract [5, 6, 29, 30], submandibular glands [4], skin [19], and endocrine glands[5] with evidence of centripetal spread of pathology in the cardiac sympathetic nerves[32]. Involvement of the bowel has been replicated in colorectal biopsies taken from patients during life, including three patients in whom the biopsies were taken prior to the onset of central nervous system symptoms [22, 23, 36–38]. Gastrointestinal dysfunction is seen in over 80 % Parkinson’s disease cases [10, 20, 21, 35]. However, the mechanism of gastrointestinal dysfunction in Parkinson’s disease is not entirely clear; one small study has found a reduction in the number of dopaminergic neurons of the myenteric plexus of patients [39], another found a non-significant correlation between the severity of α-synuclein pathology in the colon and constipation [23], and another did not find any reduction in the density of myenteric ganglia in Parkinson’s disease [3].
Neuropathological staging of central nervous system pathology in Parkinson’s disease, with the early involvement of the dorsal motor nucleus of the vagus [8], has led to the suggestion that the disease may begin in the bowel [17], which is supported by the early onset of bowel symptoms in some cases [1, 41].
Previous small scale studies looking for α-synuclein pathology in the bowel have been undertaken on symptomatic patients with Parkinson’s disease, but have only evaluated samples taken from the large intestine [22, 23, 36–38], and in only three biopsies were the samples taken from patients prior to the onset of motor symptoms [37]. This study has investigated the presence of abnormal α-synuclein aggregation in bowel tissues taken from a much larger series of patients with Parkinson’s disease as part of their routine investigations for gastrointestinal symptoms, both before and after the onset of motor symptoms. The aims of the study were to assess the specificity of α-synuclein accumulation within the bowel for Parkinson’s disease (by using a large number of controls), the suitability of routinely acquired biopsies for the detection of abnormal α-synuclein pathology and to determine as to how long prior to the onset of motor symptoms, pathology may be seen within the bowel. In addition, we examined tissue samples from the full length of the gastrointestinal tract in order to assess the relative sensitivity of different regions for detecting α-synuclein pathology, and unlike previous studies, we have compared the relative sensitivities of antibodies to both phosphorylated and non-phosphorylated forms of α-synuclein.
Methods
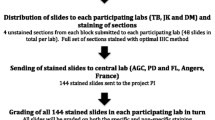
Patients were identified from the hospital’s computerised database of medical codes (admitted within the last 5 years with a diagnosis of Parkinson’s disease) and cross referenced with the histopathology laboratory’s computerised database. Those who had had previous bowel biopsies were considered for inclusion in the study; their case notes were reviewed to ensure they fulfilled UK Parkinson’s Disease Brain Bank clinical diagnostic criteria for a diagnosis of Parkinson’s disease [18]. In addition, as part of the case note review, the presence of non-motor symptoms was recorded and their date of onset. For each included patient, at least one matched control was identified from the histopathology computerised database which was from a patient of a similar age, the same gender and had the same tissue biopsied to the Parkinson’s disease patient. Where possible, the control sample was chosen to also be matched for year of removal. The case notes from all control cases were reviewed to ensure that none had clinical features of Parkinson’s disease. For all cases found to be positive, any other tissue samples within the laboratory archives were retrieved and examined. The study has South West UK research ethics committee approval.
Cases were immunostained with antibodies to phosphorylated [22] and non-phosphorylated [38] α-synuclein. In order to determine the suitability of the tissue for assessment, an antibody to S100 protein was used to identify nerve fibres and ganglia [26].
Immunohistochemistry
Four micro meter paraffin sections were de-waxed, re-hydrated and incubated with primary antibodies on an automated Leica Bond max with the following pre-treatments and titres: antibody to phosphorylated α-synuclein at Serine 129 (014–20281, WAKO, Osaka, Japan) 1:10,000, 4 min Formic acid followed by 5 min manufacturer’s enzyme pre-treatment at half strength (AR9551, Bond Enzyme pre-treatment); antibody to α-synuclein (NCL-L-ASYN, Leica Biosystems, Newcastle Upon Tyne, U.K.) 1:400, 4 min Formic acid followed by 30 min epitope retrieval pre-treatment (AR9640 Bond Epitope Retrieval Solution 2); antibody to S100 protein (Z0311, DAKO, Glostrup, Denmark), 1:3,000, 10 min enzyme pre-treatment (AR9551, Bond Enzyme pre-treatment). Bond max reagents supplied by Leica Biosystems, Newcastle Upon Tyne, U.K. A positive control autopsy brain sample from a patient with dementia with Lewy bodies was used in each immunohistochemical run. Negative controls, omitting the primary antibodies, were used to validate positive staining.
In addition, in selected cases, double labelling using fluorescent secondary antibodies was undertaken. Pre-treatments were as above and autofluorescence was quenched with Sudan black (10 mg/ml in ethanol) for 5 min. Secondary antibodies consisted of goat anti-rabbit 488 (Alexa Fluor, Invitrogen, Cat.-no A11008), visible with a FITC filter, and goat anti-mouse 594 (Alexa Fluor, Invitrogen, Cat.-no A11005), visible with a Texas Red filter, which were applied at 1:200 for 120 min.
All sections were given an anonymised study number and were reviewed by the pathologist (DAH) blind to the diagnosis. Cases and controls without any nerve fibres visible with S100 immunocytochemistry were excluded from the study.
Results
A total of 117 gastrointestinal tissue samples from 62 Parkinson’s disease patients (Supplementary Fig. 1) and 161 tissue samples from 161 control patients were included in the study. These consisted of a mixture of upper and lower gastrointestinal biopsies and cholecystectomies. The ages of the Parkinson’s disease patients at time of diagnosis were 46–85 years (mean 68 years) and of controls at the times of biopsy were 44–90 years (mean 71 years). It was noted that many of the biopsies were small and superficial due to prior extensive examination. A total of 39 (12 %) biopsies were excluded due to the lack of any visible nerve fibres with S100 immunocytochemistry. There were more cases excluded from the Parkinson’s disease group (31 compared with 8 controls), which is probably related to the higher rate of abnormal biopsy in this group, which often resulted in more extensive examination at the time of histological reporting, leaving less tissue for the study. A summary of the biopsies examined from Parkinson’s disease patients is given in Table 1. Of the biopsies from Parkinson’s disease patients 41 were histologically normal, 41 had inflammatory changes, and there were 22 adenomas, 5 adenocarcinomas, 4 hyperplastic polyps, 2 Barrett’s oesophagus, 1 gastrointestinal stromal tumour and 1 was ischaemic. Of the 161 controls included, there were 14 oesophageal biopsies, 45 gastric biopsies, 26 small intestinal biopsies, 69 colorectal biopsies and 6 gall bladders. The controls were largely histologically normal (113 cases), with 30 showing inflammatory changes and 18 adenomas. It was noted that in many of the Parkinson disease and control samples where submucosal ganglia were present in the biopsy, fine granular cytoplasmic immunoreactivity was seen with both antibodies, similar to that reported previously [7, 14], however, this was interpreted as normal α-synuclein expression and not scored.
Of the 117 Parkinson’s disease samples, 12 contained α-synuclein positive neurites within the lamina propria (Fig. 1), and in some of the deeper biopsies there was irregular staining of submucosal myenteric nerve fibres and small rounded inclusions within submucosal ganglia (Fig. 2). Double labelling with antibodies to phosphorylated α-synuclein and S100 protein confirmed that the immunoreactive structures were neurites. The distribution of positive immunoreactivity was variable, and in some cases was very focal. In all cases there was immunoreactivity with the antibody to phosphorylated α-synuclein, and in all but one positive biopsy (the gastric biopsy from PD3 which had very few positive neurites), the non-phosphorylated antibody showed similar staining, although was much less extensive (Fig. 1).
Duodenal (a, b) and colonic (c, d) biopsies taken from case PD10, 1 year before diagnosis, showing accumulation α-synuclein in the form or linear neuritic and larger rounded deposits in the mucosal and submucosal nerves. More extensive accumulation is seen with antibodies to phosphorylated α-synuclein (a, c), compared with parallel sections stained with an antibody to non-phosphorylated α-synuclein (b, d) gastric biopsy from case PD3 taken 8 years before diagnosis showing occasional linear deposits of phosphorylated α-synuclein (e)
Of the positive biopsies from the pre-symptomatic phase, the two positive gastric biopsies (PD3 and PD85) showed helicobacter-associated gastritis, and the positive colonic biopsy (P10) showed mild non-specific inflammation; the patient had a clinical diagnosis of ulcerative colitis. However, many of the positive biopsies did not show any inflammation.
Although the number of positive samples was small, the proportions of positive biopsies in both the upper and lower gastrointestinal tract were similar (see Table 1). When assessing the biopsies in relation to the time of diagnosis of Parkinson’s disease a similar proportion of positive biopsies was seen in those taken pre-biopsy to those post-biopsy (see Table 2).
All patients with positive biopsies had autonomic symptoms (see Table 3), sometimes prior to the onset of motor symptoms (more detail about the clinical features of the patient cohort is presented in Supplementary Table 1).
Examination of tissue taken from outside of the gastrointestinal tract in positive cases did not reveal any α-synuclein immunoreactivity (see Table 3).
None of the controls showed any α-synuclein immunoreactive neurites or cytoplasmic bodies.
Discussion
Our study has confirmed the early and persistent accumulation of α-synuclein in the gastrointestinal tract of patients with Parkinson’s disease. Previous studies have demonstrated α-synuclein accumulation in the colon and rectum from living patients [22, 38], although pathology is known to be more widespread in the gastrointestinal tract at autopsy [5, 6]. Our study has confirmed the involvement of the stomach and duodenum in the early stages of the disease, and therefore offer alternative sites to biopsy for diagnosis. Although we cannot be entirely confident that neurological motor signs were not present, in two of our patients immunoreactivity was seen in gastric biopsies taken 6 and 8 years prior to the onset of the first motor symptoms as noted by the patients, which extends the findings from the recent report which identified abnormal α-synuclein immunoreactivity in the colon from three patients up to 5 years prior to the onset of symptoms [37]. The proportion of positive biopsies in our study is lower than that has been reported in previous studies [22, 38]; however in these latter studies the biopsies were taken specifically to look for α-synuclein accumulation and were examined extensively by thick sections [38], or whole mount preparations [22], allowing far more neural tissue to be assessed. A major limitation of our approach is that all of the biopsies that we have used were taken as part of the patient’s investigation for a variety of symptoms, and had often been extensively examined for this purpose, leaving relatively little tissue remaining for α-synuclein assessment. In addition the samples included a significant number of tumours and adenomas, which contained nerve fibres that developed as part of the lesion, and there were several gall bladders, which have not been assessed in autopsy studies. These factors are likely to have contributed to the relatively low rate of positive findings in our study. However, even with our rate of positive α-synuclein immunoreactivity of around 10 %, we feel that review of archived biopsies may be worthwhile in order to try and confirm a diagnosis of idiopathic Parkinson’s disease in some cases where there is diagnostic doubt. We might have expected to find some positives in our control group, due to cases of incidental Lewy body disease [5, 6, 28], however, the lower sensitivity of using archival material suggests that positive findings with this approach are highly specific for Parkinson’s disease. Although some of the positive gastrointestinal biopsies showed inflammation, this was related to an associated inflammatory bowel disorder, and a previous study specifically included a control group with inflammatory bowel disease which all were negative [38], suggesting that the α-synuclein accumulation is not secondary to inflammation.
Our findings of early gastrointestinal involvement lend support to the hypothesis that Parkinson’s disease may originate within the gastrointestinal tract [16]. In patients from whom there were serial biopsies present once immunoreactivity is detectable we have shown that it remains so throughout the course of the disease, and although not formally quantified, there was no obvious increase in the number of immunoreactive fibres throughout the course of the disease. Double-labelling confirmed the presence of α-synuclein within neurites, and previous studies have suggested that the majority of these positive fibres express tyrosine hydroxylase [23]. The proportion of biopsies positive pre- and post-diagnosis was not significantly different, which in keeping with early and persistent gastrointestinal immunoreactivity. Autopsy studies have shown that gastrointestinal involvement is present in the majority of cases of incidental Lewy body disease [5, 6], with a rostro-caudal decrease in density of pathology [5, 43]. A single study of surgical specimens demonstrated α-synuclein accumulation in the autonomic nerves of both the urogenital system and gastrointestinal tract of neurologically unimpaired individuals, suggesting early pre-symptomatic involvement [28]. These findings lend some support to the hypothesis that α-synuclein pathology occurs early in the gastrointestinal tract and may extend along the peripheral autonomic nervous system to the dorsal motor nucleus of the vagus [16]. Large scale autopsy studies looking for pre-symptomatic gastrointestinal α-synuclein accumulation have not been undertaken, but a small study did not find any cases of bowel involvement without central nervous system in 40 patients [5], and a larger autopsy study looking for α-synuclein pathology in the adrenal gland found only one case out of over 570 patients without central nervous system pathology [12]. We did not find any positive samples of skin or prostate; however, the number of cases examined was too small to draw conclusions about whether these sites are involved early in the disease. However, two previous studies have demonstrated α-synuclein pathology in 2 out of 20 skin biopsies and none out of seven olfactory epithelium biopsies from living patients [27, 44].
Other support for a gastrointestinal origin comes from animal studies which have shown that chronic oral ingestion of low dose rotenone can lead to accumulation of α-synuclein in the enteric nervous system, followed by the dorsal motor nucleus of the vagus [33], and that the central nervous system involvement can be prevented by vagotomy [34]. Chronic rotenone models have been shown to result in gastrointestinal motility [2, 15]; however, gastrointestinal disturbance is less marked with high dose treatment [40]. There are experimental data to suggest that abnormal α-synuclein may spread from cell to cell and along nerves, with accumulating evidence for template mediated transformation in a prion-like manner (see review [13]).
This study for the first time demonstrates accumulation of phosphorylated α-synuclein in the autonomic nervous system of both the upper and lower gastrointestinal tract in living patients with Parkinson’s disease, and has shown it to be present at least 8 years prior to the onset of motor symptoms, remaining detectable throughout the course of the disease. This pre-symptomatic presence of α-synuclein in the bowel may represent either the initial site of pathology prior to its spread into the central nervous system, or an early site of involvement due to the selective vulnerability of bowel plexus neurons. Although our approach using archival samples has a relatively low sensitivity for reasons discussed above, studies using prospectively collected biopsies allow examination of more tissue and a much greater sensitivity [23, 36, 38]. Further study of these observations may allow a better understanding of the factors influencing the development of early α-synuclein aggregation in the bowel. In addition, the high specificity of α-synuclein accumulation in the bowel for Parkinson’s disease will allow confirmation of diagnosis during life, a potential means of the identification of at risk individuals and also offers the possibility of monitoring the effects of future disease modifying treatments at the cellular level.
References
Abbott RD, Petrovitch H, White LR et al (2001) Frequency of bowel movements and the future risk of Parkinson’s disease. Neurology 57:456–462
Anderson G, Noorian AR, Taylor G et al (2007) Loss of enteric dopaminergic neurons and associated changes in colon motility in an MPTP mouse model of Parkinson’s disease. Exp Neurol 207:4–12
Annerino DM, Arshad S, Taylor GM, Adler CH, Beach TG, Greene JG (2012) Parkinson’s disease is not associated with gastrointestinal myenteric ganglion neuron loss. Acta Neuropathol 124:665–680
Beach TG, Adler CH, Dugger BN et al (2013) Submandibular gland biopsy for the diagnosis of Parkinson disease. J Neuropathol Exp Neurol 72:130–136
Beach TG, Adler CH, Sue LI et al (2010) Multi-organ distribution of phosphorylated alpha-synuclein histopathology in subjects with Lewy body disorders. Acta Neuropathol 119:689–702
Bloch A, Probst A, Bissig H, Adams H, Tolnay M (2006) Alpha-synuclein pathology of the spinal and peripheral autonomic nervous system in neurologically unimpaired elderly subjects. Neuropathol Appl Neurobiol 32:284–295
Böttner M, Zorenkov D, Hellwig I et al (2012) Expression pattern and localization of alpha-synuclein in the human enteric nervous system. Neurobiol Dis 48:474–480
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Cersosimo MG, Benarroch EE (2012) Autonomic involvement in Parkinson’s disease: pathology, pathophysiology, clinical features and possible peripheral biomarkers. J Neurol Sci 313:57–63
Cersosimo MG, Benarroch EE (2012) Pathological correlates of gastrointestinal dysfunction in Parkinson’s disease. Neurobiol Dis 46:559–564
Dorsey ER, Constantinescu R, Thompson JP et al (2007) Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology 68:384–386
Fumimura Y, Ikemura M, Saito Y et al (2007) Analysis of the adrenal gland is useful for evaluating pathology of the peripheral autonomic nervous system in lewy body disease. J Neuropathol Exp Neurol 66:354–362
George S, Rey NL, Reichenbach N, Steiner JA, Brundin P (2013) Alpha-synuclein: the long distance runner. Brain Pathol 23:350–357
Gold A, Turkalp ZT, Munoz DG (2013) Enteric alpha-synuclein expression is increased in Parkinson’s disease but not Alzheimer’s disease. Mov Disord 28:237–240
Greene JG, Noorian AR, Srinivasan S (2009) Delayed gastric emptying and enteric nervous system dysfunction in the rotenone model of Parkinson’s disease. Exp Neurol 218:154–161
Hawkes CH, Del Tredici K, Braak H (2007) Parkinson’s disease: a dual-hit hypothesis. Neuropathol Appl Neurobiol 33:599–614
Hawkes CH, Del Tredici K, Braak H (2009) Parkinson’s disease: the dual hit theory revisited. Ann N Y Acad Sci 1170:615–622
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Ikemura M, Saito Y, Sengoku R et al (2008) Lewy body pathology involves cutaneous nerves. J Neuropathol Exp Neurol 67:945–953
Jost WH (2010) Gastrointestinal dysfunction in Parkinson’s disease. J Neurol Sci 289:69–73
Jost WH, Eckardt VF (2003) Constipation in idiopathic Parkinson’s disease. Scand J Gastroenterol 38:681–686
Lebouvier T, Chaumette T, Damier P et al (2008) Pathological lesions in colonic biopsies during Parkinson’s disease. Gut 57:1741–1743
Lebouvier T, Neunlist M, des Varannes Bruley S et al (2010) Colonic biopsies to assess the neuropathology of Parkinson’s disease and its relationship with symptoms. PLoS One 5:e12728
Lees AJ, Hardy J, Revesz T (2009) Parkinson’s disease. Lancet 373:2055–2066
Lim SY, Fox SH, Lang AE (2009) Overview of the extranigral aspects of Parkinson disease. Arch Neurol 66:167–172
MacKenzie JM, Dixon MF (1987) An immunohistochemical study of the enteric neural plexi in Hirschsprung’s disease. Histopathology 11:1055–1066
Miki Y, Tomiyama M, Ueno T et al (2010) Clinical availability of skin biopsy in the diagnosis of Parkinson’s disease. Neurosci Lett 469:357–359
Minguez-Castellanos A, Chamorro CE, Escamilla-Sevilla F et al (2007) Do alpha-synuclein aggregates in autonomic plexuses predate Lewy body disorders?: a cohort study. Neurology 68:2012–2018
Mu L, Sobotka S, Chen J et al (2013) Alpha-synuclein pathology and axonal degeneration of the peripheral motor nerves innervating pharyngeal muscles in Parkinson disease. J Neuropathol Exp Neurol 72:119–129
Mu L, Sobotka S, Chen J et al (2013) Parkinson disease affects peripheral sensory nerves in the pharynx. J Neuropathol Exp Neurol 72:614–623
Nussbaum RL, Ellis CE (2003) Alzheimer’s disease and Parkinson’s disease. N Engl J Med 348:1356–1364
Orimo S, Uchihara T, Nakamura A et al (2008) Axonal alpha-synuclein aggregates herald centripetal degeneration of cardiac sympathetic nerve in Parkinson’s disease. Brain 131:642–650
Pan-Montojo F, Anichtchik O, Dening Y et al (2010) Progression of Parkinson’s disease pathology is reproduced by intragastric administration of rotenone in mice. PLoS ONE 5:e8762
Pan-Montojo F, Schwarz M, Winkler C et al (2012) Environmental toxins trigger PD-like progression via increased alpha-synuclein release from enteric neurons in mice. Sci Rep 2:898
Pfeiffer RF (2003) Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol 2:107–116
Pouclet H, Lebouvier T, Coron E et al (2012) A comparison between rectal and colonic biopsies to detect Lewy pathology in Parkinson’s disease. Neurobiol Dis 45:305–309
Shannon KM, Keshavarzian A, Dodiya HB, Jakate S, Kordower JH (2012) Is alpha-synuclein in the colon a biomarker for premotor Parkinson’s disease? Evidence from 3 cases. Mov Disord 27:716–719
Shannon KM, Keshavarzian A, Mutlu E et al (2012) Alpha-synuclein in colonic submucosa in early untreated Parkinson’s disease. Mov Disord 27:709–715
Singaram C, Ashraf W, Gaumnitz EA et al (1995) Dopaminergic defect of enteric nervous system in Parkinson’s disease patients with chronic constipation. Lancet 346:861–864
Tasselli M, Chaumette T, Paillusson S et al (2013) Effects of oral administration of rotenone on gastrointestinal functions in mice. Neurogastroenterol Motil 25:e183–e193
Ueki A, Otsuka M (2004) Life style risks of Parkinson’s disease: association between decreased water intake and constipation. J Neurol 251(Suppl 7):vII18–vII23
Verbaan D, Marinus J, Visser M, van Rooden SM, Stiggelbout AM, van Hilten JJ (2007) Patient-reported autonomic symptoms in Parkinson disease. Neurology 69:333–341
Wakabayashi K, Takahashi H, Takeda S, Ohama E, Ikuta F (1988) Parkinson’s disease: the presence of Lewy bodies in Auerbach’s and Meissner’s plexuses. Acta Neuropathol 76:217–221
Witt M, Bormann K, Gudziol V et al (2009) Biopsies of olfactory epithelium in patients with Parkinson’s disease. Mov Disord 24:906–914
Acknowledgments
This study was supported by research funding from the South West Neurosciences Association.
Conflict of interest
None of the authors has any conflicts of interest in relation to this work.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hilton, D., Stephens, M., Kirk, L. et al. Accumulation of α-synuclein in the bowel of patients in the pre-clinical phase of Parkinson’s disease. Acta Neuropathol 127, 235–241 (2014). https://doi.org/10.1007/s00401-013-1214-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-013-1214-6