Abstract
The amyloid cascade hypothesis of Alzheimer’s disease (AD) is testable: it implies that interference with Aβ aggregation and plaque formation may be therapeutically useful. Aβ42 immunisation of amyloid precursor protein (APP) transgenic mice prevented plaque formation and caused removal of existing plaques. The first clinical studies of Aβ immunisation in AD patients (AN1792, Elan Pharmaceuticals) were halted when some patients suffered side effects. Since our confirmation that Aβ immunisation can prompt plaque removal in human AD, we have performed a clinical and neuropathological follow up of AD patients in the initial Elan Aβ immunisation trial. In immunised AD patients, we found: a lower Aβ load, with evidence that plaques had been removed; a reduced tau load in neuronal processes, but not in cell bodies; and no evidence of a beneficial effect on synapses. There were pathological “side effects” including: increased microglial activation; increased cerebral amyloid angiopathy; and there is some evidence for increased soluble/oligomeric Aβ. A pathophysiological mechanism involving effects on the cerebral vasculature is proposed for the clinical side effects observed with some active and passive vaccine protocols. Our current knowledge of the effects of Aβ immunotherapy is based on functional information from the early clinical trials and a few post mortem cases. Several further clinical studies are underway using a variety of protocols and important clinical, imaging and neuropathological data will become available in the near future. The information obtained will be important in helping to understand the pathogenesis not only of AD but also of other neurodegenerative disorders associated with protein aggregation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The limitations of post mortem neuropathology in understanding Alzheimer’s disease (AD)
The neuropathology of AD is characterised macroscopically by widespread cerebral atrophy and microscopically by: accumulation of amyloid-β (Aβ) protein in the form of plaques in the grey matter and in the walls of blood vessels as cerebral amyloid angiopathy (CAA); accumulation of tau protein within neurons—in the cell bodies as neurofibrillary tangles, in neuronal processes as dystrophic neurite clusters associated with plaques, and as neuropil threads distributed through the grey matter; synaptic and neuronal loss; reactive microglia and astrocytes [59]. These features have been defined based on post mortem human neuropathology and their pathological recognition is still viewed as the gold standard for the diagnosis for AD. However, post mortem neuropathological studies have limitations in terms of the understanding of the disease pathogenesis; only a single time point in the development of the disease is assessable and that time point, in many cases, is at the end of the disease process many years or even decades after the disease initiation. A consequence of this limited histological view of AD is the difficulty in gaining a clear conception of how the different features of the disease are inter-related, both in terms of the timing of their appearance during AD pathogenesis and also in terms of cause and effect. If it was possible to manipulate one feature of the disease then, by analysing the effects this had on other features of the disease, it might be possible to obtain useful insights into the interconnectivity of the different aspects of the neuropathology of AD.
The amyloid cascade hypothesis
For many years, a major driving force behind much of the research in understanding AD pathogenesis has been the amyloid or Aβ cascade hypothesis [38]. In order to prevent this concept from becoming an overwhelming dogma, it is useful to scrutinise the evidence on which this hypothesis is based. The major supporting evidence is as follows:
-
APP gene point mutations cause AD in some rare familial cases [27, 49, 73, 108, 109, 129].
-
Rare familial forms of AD caused by point mutations in APP, PS1 and PS2 genes have in common increased Aβ42, a form which is particularly prone to aggregation [37, 71, 72, 95, 96, 115, 128].
-
People affected by Down’s syndrome, due usually to triplication of chromosome 21 on which the APP gene is located, consistently develop AD pathology at an early age [40].
-
The APOE ε4 allele, the major genetic risk factor for the common form of AD (i.e. sporadic AD) [110], is associated with Aβ accumulation [44].
-
Transgenic mice expressing human AD-causing gene point mutations develop some features of AD pathology, including Aβ plaques, with ageing [13, 29, 42, 45, 111].
The unifying thread for these points involves Aβ in the form of fibrillar or oligomeric aggregates as the starting point of the disease process, leading ultimately to the generation of the full spectrum of AD pathology [39, 100]. It is worth noting that most of this evidence is derived from rare genetically caused forms of AD rather than the much more common sporadic form of the disease. Although similar in neuropathological characteristics, it requires a leap of faith to extrapolate the same mechanism of disease pathogenesis from genetically caused AD to sporadic AD. Indeed, credible alternative hypotheses exist, e.g., putting APOE at the centre of the disease-initiating process. APOE acts as a lipid transport protein in the central nervous system [3, 14, 18], delivering to neurons lipids which are essential for the development and maintenance of membranes and synapses [87], and thus for synaptic plasticity [64], an important physiological process in the establishment of memory [51, 52, 57, 75, 80, 82, 117]. Nevertheless, the Aβ cascade hypothesis provides a clearly testable hypothesis that AD results from production of Aβ peptide by cleavage of APP protein by β and γ secretases [54] with subsequent Aβ aggregation and that this causes, directly or indirectly, all of the pathological and functional abnormalities of AD.
Aβ immunotherapy in animal models
Immunotherapeutic manipulation of Aβ, in effect testing the Aβ cascade hypothesis, emerged with the seminal work of Schenk and colleagues [97] on PDAPP transgenic mice, which bear a human familial AD-causing APP gene point mutation and develop Aβ plaques, resembling those seen in AD, as they age [29]. Active immunisation of PDAPP mice with Aβ42 peptide early in their lives, before the appearance of plaques, was found to abolish the formation of plaques with ageing. It was also observed that immunisation of older mice, in which plaques were already present, resulted in a reduction in plaque load, with some evidence that plaques had been actively removed [97]. This study has spawned a major field within AD research involving exploration of a number of different active and passive Aβ immunisation protocols [1, 5–7, 50, 56, 60, 67, 69, 90, 105], their effects on pathology and function in animal models [58, 68, 126] and, subsequently, second generation clinical trials which are currently in progress [55, 127]. Early studies in mice showed that not only there was prevention or reversal of some of the Aβ-associated pathology in these models (e.g. synaptic loss) but also there were benefits in terms of preventing or reversing the decline in function [16, 47, 68, 81, 104, 125, 126].
The first Aβ immunotherapy clinical trial
Concepts from these early studies of immunotherapy in experimental models were first translated into human studies by Elan Pharmaceuticals who initiated a clinical trial in year 2000. The study involved active immunisation with full length Aβ42 and the adjuvant QS21 (AN1792) of patients with mild to moderate AD [Mini-mental State Examination (MMSE) 15-25] [28]. A total of 80 patients were enrolled in 4 clinical trial centres across the south of the UK (Southampton, Cardiff, Bath and Swindon). In each centre, 16 patients received Aβ42 plus adjuvant and 4 patients received the adjuvant alone as a placebo control. This was designed primarily as a safety and immunogenicity study, rather than a study of efficacy [8]. The findings were that no major adverse events occurred and Aβ antibodies were detectable in blood samples in more than half of the patients receiving the active vaccine [8].
Active Aβ42 immunotherapy removes Aβ deposits from the human brain
In 2002, one of the patients receiving the active vaccine in the first Elan Pharmaceuticals trial died for reasons unrelated to the trial and we had the opportunity to see for the first time the effect of Aβ immunisation in AD. The findings were remarkable in that there were extensive areas of cerebral cortex devoid of Aβ plaques [78]. However, plaques remained in other cortical areas and there was residual tau pathology, permitting a neuropathological diagnosis of AD in which there had been some removal of Aβ plaques [78]. These intriguing observations prompted us to perform a long-term clinical and neuropathological follow-up study of the patients who had enrolled in the trial. Meanwhile, a second clinical trial of AN1792 had begun, recruiting a total of 372 patients with mild to moderate AD in centres in Europe and the United States. This trial was halted when it was recognised that a small proportion of the patients (6%) were experiencing side effects interpreted as inflammatory in nature [83].
Our initial census of the clinicopathological follow-up study provided information from post mortem neuropathology on nine patients, all of whom had received the active Aβ42 vaccine, and seven of whom had responded by generating detectable titres of antibodies to Aβ [43]. Survival times after the first immunisation dose ranged from 4 to 64 months. In one case, the neuropathological diagnosis was progressive supranuclear palsy, not AD, and it was excluded from subsequent analysis. This case highlights the point that, despite major recent advances, clinical diagnosis of the pathological substrate underlying dementia is not perfect. This is a point that is currently being urgently addressed, by searching for biomarkers and new imaging methodologies, because having 10% or so of the patients in a therapeutic trial that do not have the disease process targeted by the therapy impairs the statistical power of the study [130]. The neuropathology from the immunised AD cases (iAD) was compared with unimmunised AD archival histology controls (cAD, n = 12), matched for age at death, history of progressive dementia and which satisfied consensus criteria for AD.
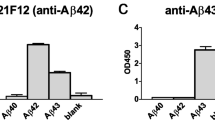
The histological pattern of Aβ immunostaining in the cerebral cortex in the iAD cases was remarkably variable: some cases (Fig. 1a) had a plaque density indistinguishable from AD controls, some had almost complete absence of plaques (Fig. 1b), whereas others had an intermediate appearance often with alternating patches of presence and absence of plaques in the cortex (Fig. 1c) [43]. This variability in distribution of Aβ throughout the cerebral cortex is illustrated in whole sections of frontal lobe to give an impression of variable occurrence of plaque removal (Fig. 1e–g). All iAD cases illustrated had Aβ antibody titres detectable in the blood. In Fig. 1e, Aβ remains present extensively throughout the neocortex with only a few small patches devoid of Aβ. In Fig. 1f, there is an intermediate pattern with patches and bands of residual Aβ within the cortex. In contrast, in Fig. 1g, there is virtually complete absence of Aβ from the hemisphere. Quantification of Aβ42 immunostaining throughout frontal, temporal and parietal neocortex revealed a substantially lower Aβ42 load in the iAD cases compared with the AD controls (Fig. 1h; iAD: 2.70 vs. cAD: 4.55; P = 0.026).
Low power views of Aβ immunohistochemistry in the cerebral neocortex of patients with Alzheimer’s disease after Aβ immunisation to illustrate the variability and often patchy nature of plaque removal: a–c three iAD cases with a high immune response compared to d an unimmunised AD case. a iAD case with extensive Aβ plaques remaining throughout the cortex. b iAD case with virtually complete absence of Aβ. c iAD case with an intermediate pattern characterised by patches and bands of residual Aβ within the cortex. d Unimmunised AD case with Aβ throughout the neocortex. e–g Scanned images of Aβ immunostained sections of whole frontal lobe from three iAD cases, each with a high immune response, showing marked variability in the amount of Aβ (yellow) remaining in the cortex. h Quantification of Aβ42 load in the cerebral neocortex shows it is significantly lower after Aβ immunisation (n = 9) compared with unimmunised AD cases (n = 12). Scale bar 0.5 mm. iAD immunised AD, cAD unimmunised AD
It is important to note that demonstrating a lower Aβ load in iAD cases than in AD controls is not the same as demonstrating that Aβ has been removed by the immunotherapy. Ideally, histological samples of cortex would be available from before treatment and after treatment from each patient. Recently, in vivo PET imaging of amyloid using Pittsburgh B compound has confirmed that Aβ immunotherapy does indeed result in a reduction in amyloid signal when comparing post-treatment scans with pre-treatment scans. However, before this, we were able to define a constellation of features based on Aβ immunohistochemistry which we interpreted as reflecting positive evidence of Aβ plaque clearance [76]. This interpretation was given confidence as each of these histological features is also demonstrated in PDAPP mice actively immunised with Aβ42 peptide [30, 97]. The positive features of Aβ clearance following Aβ immunotherapy are as follows:
-
A “moth-eaten” appearance of some remaining diffuse plaques, interpreted as reflecting partial or ongoing removal of diffuse amyloid (Fig. 2a).
Fig. 2 Illustrations of the key histological features reflecting Aβ removal after Aβ immunisation. a Moth-eaten appearance of remaining diffuse plaques and a granular pattern of Aβ immunostaining within microglia. b Residual plaque cores in plaque-free areas. c Abundant Aβ42 in the cortical and leptomeningeal vasculature in an area devoid of plaques. d Association of Aβ with capillaries in plaque-free areas. Double-label confocal microscopy for Aβ (green) and HLA-DR (red) showing e only very occasional granules of Aβ in an unimmunised AD case compared with f abundant Aβ within microglia in an immunised AD case. Scale bar a, b, d 50 μm, c 150 μm, e, f 20 μm. Arrow moth-eaten plaques, arrow head core plaques, asterisk Aβ within microglia, white arrow colocalisation Aβ and HLA-DR (yellow)
-
Residual plaque cores in plaque-free areas, interpreted as reflecting removal of diffuse amyloid from dense core plaques (Fig. 2b).
-
Marked Aβ within the walls of cortical and leptomeningeal arteries (CAA). Much of this is Aβ42, which is usually scarce in sporadic CAA, and is interpreted as being derived from plaques that have been “dissolved” by the immunotherapy [11] (Fig. 2c).
-
Association of Aβ with capillaries in plaque-free areas, both within the walls of the capillaries and forming nodules attached to the outer surface of the capillaries (Fig. 2d).
-
A granular pattern of Aβ immunoreactivity within microglia (Fig. 2a). This pattern reflects Aβ within microglial lysosomes, is confirmed by double-label confocal microscopy, and is therefore interpreted as Aβ which has been phagocytosed; Aβ was observed very infrequently within microglia in unimmunised AD cases [76] (Fig. 2e, f).
A striking feature of the findings was the considerable variability of Aβ plaque removal after immunotherapy which may be explained, at least in part, by the variability in the immune response to Aβ immunisation. Active immunisation in AD relies on the ageing immune system to generate antibodies and only 53% of the patients in the study generated Aβ antibodies [8], with considerable variation in peak titres amongst the responders. A significant association was observed between the mean Aβ antibody response assessed during the 18-month trial period and the degree of Aβ plaque removal subsequently identified at post mortem [43]. Nevertheless, the levels of antibody titres in the blood seem unlikely to fully explain the patchy nature of plaque removal in some of the cases and the reasons for this variability remain unclear. A possible explanation may relate to access of immunoglobulins from the blood into the brain parenchyma, a process which seems to be poorly understood, and which may depend on the physiological/pathophysiological status of local blood vessels.
Neuropathological studies have been performed on some patients who were immunised with the same vaccine (AN1792) in the subsequent trial. In that study dosing was halted, because of recognition of side effects [83], after patients had received only 1, 2 or 3 vaccine doses, rather than the 8 doses received by the patients in the initial trial. Nevertheless, essentially identical pathological alterations have been described in these patients [12, 26, 62, 78].
Active Aβ42 immunotherapy influences tau pathology
One important unanswered question about the pathogenesis of AD, which potentially can be addressed in these studies, is the inter-relationship between Aβ and tau. There has long been controversy surrounding whether plaques (Aβ aggregation) and/or tangles (tau aggregation) appear earlier in the disease process; their inter-relationship in terms of cause and effect, and which, if either, is more important in influencing cognitive function. In studying the neuropathology of the first immunised AD case, it became clear that plaque removal did indeed have some influence on tau pathology [78]. In this case, there were areas of cortex where plaques remained and appeared unaffected by the immunotherapy process and other areas completely devoid of plaques, where plaques were presumed to have been removed. Subjective assessment of tau immunostaining in corresponding areas showed that where plaques remained, tau was present as expected in plaque-associated dystrophic neurite clusters, tangles and neuropil threads. In contrast, where plaques had been removed, tangles and neuropil threads remained but there was complete absence of dystrophic neurite clusters. The inference is that when Aβ plaques are cleared by immunotherapy, the plaque-associated tau-containing dystrophic neurites are also cleared. This interpretation was supported by observations from a mouse study using the elegant technology of in vivo multiphoton microscopy which allows revisualisation of individual plaques over a period of days. This study showed that removal of a plaque following application of Aβ antibody was associated with removal of the dystrophic neurites associated with that plaque [15]. However, it is important to point out that although there are dystrophic neurites associated with the plaques in this mouse model there is no aggregation of tau within the neurites.
Those preliminary observations were confirmed in two subsequent cases [76] and prompted us to revisit this question in a quantitative fashion when more cases became available. Quantification of Aβ42 and phospho-tau (AT8) immunohistochemistry was performed in 3 neocortical regions (superior and middle temporal gyrus, inferior parietal lobule and medial frontal gyrus) and the hippocampal formation (CA1, subiculum and entorhinal cortex) in 10 iAD cases and 28 AD controls matched for age, disease duration and APOE genotype [9]. The results demonstrated that in the iAD cases, compared with cAD cases, in association with a lower Aβ42 load there was a significantly lower phospho-tau load in the neocortex and all three hippocampal fields. The interpretation is that Aβ immunotherapy has an effect not only in reducing histologically detectable Aβ but also has an effect on intraneuronal phospho-tau accumulation. The effect appears to be restricted to phospho-tau accumulation in neuronal processes, both in the form of dystrophic neurite clusters and neuropil threads. In contrast, there was no difference in the density of phospho-tau positive neuronal cell bodies, or in Braak stage, between the iAD and cAD cases (Fig. 3). The patients in the trial were immunised at the stage of mild to moderate AD (MMSE 15-25), corresponding to a Braak stage in the range III–V [74]; as 9/10 were stage VI when they died, this implies that accumulation of phospho-tau in neuronal cell bodies and tangle formation may have continued despite Aβ immunotherapy.
Illustration of the effect of Aβ immunisation on plaques and tangles using modified Bielschowsky staining. In unimmunised AD (left), tangles and plaques are visible, with dystrophic neurites associated with some of the plaques (arrow). In immunised AD (right), the plaques and associated dystrophic neurites are gone, but the tangles remain. cAD unimmunised AD case, iAD immunised AD case. Scale bar 50 μm
A recent detailed study of the hippocampi of five patients immunised with AN1792 in the second trial identified a reduction in abnormal curvature of neuronal processes and some differences in tau-neuronal cell body, notably a reduction in late stage hyperphosphorylated tau [101]. However, as observed in the study described above, the density of neurofibrillary tangles was not affected by the immunotherapy. Overall, this evidence of a relative reduction of phospho-tau in neurons seems likely to reflect a beneficial effect on neuronal metabolism of the removal of Aβ prompted by Aβ immunisation.
In conclusion, there seems to be clear evidence that tau pathology can be ameliorated to some extent by Aβ immunisation [9, 76, 78, 101] with the effects most marked on phospho-tau aggregation in the neuronal processes rather than neuronal cell body. However, even when plaque clearance is very extensive, there is still substantial aggregated tau protein. This raises the possibility that a combined approach targeting both aggregated Aβ and tau may be of beneficial. A few studies have been performed in experimental models which suggest that tau antibodies can modify tau pathology [4, 103], but as far as we are aware a combination of Aβ and tau immunotherapy has not been investigated.
Is there a beneficial effect of Aβ immunotherapy on synapses?
Previous studies of AD have shown a close correspondence between synaptic loss and cognitive decline [21, 53, 61, 100, 112, 113]. Despite much investigation, the pathophysiological link between Aβ aggregation and synaptic dysfunction and loss remains poorly understood. From the earliest studies, which demonstrated that synaptic loss in AD occurs not only within cortical amyloid plaques but is also distributed throughout the cortical neuropil [63], it seemed clear that the presence of the plaques themselves is not directly responsible for the synaptic loss. More recent studies have focused on the synaptotoxic role of Aβ oligomers which interfere with long-term potentiation [102, 118].
In our study, quantification of synaptophysin immunohistochemistry, both relative optical density measurements and protein load, showed no difference between iAD cases and cAD cases (Fig. 4). Indeed, the cortical and hippocampal neuropil were severely degenerated in many of the iAD cases, with marked status spongiosus typical of advanced AD, including those iAD cases in which plaque removal was virtually complete. In other words, removal of plaques in the iAD cases seemed to confirm no protective benefit to synapses. This observation is based on a small number of cases and merits further and more detailed study.
Lack of an effect of plaque removal induced by Aβ immunotherapy on synapses. An iAD case showing a a neocortical area with plaques remaining and b the corresponding area stained for synaptophysin (presynaptic protein, SY38) compared with c an area in which plaques have been removed and d the corresponding area stained for synaptophysin. There is no visible difference in the synaptic staining as a consequence of the plaque removal. e This observation is confirmed by the absence of a significant difference in the quantification of synaptophysin load or relative optical density (using the pons as a reference) of synaptophysin immunohistochemistry in seven immunised AD cases (iAD) and nine unimmunised AD cases (cAD). Scale bar 50 μm
The overall histological changes in AD pathology induced by Aβ immunotherapy are illustrated in Fig. 5.
Cartoon to summarise the effects of Aβ immunotherapy on Alzheimer’s disease histopathology. Stage 0 In unimmunised AD, all of the characteristic features of the disease are present as illustrated. Following immunotherapy, stage 1 antibodies enter the brain and bind to plaques resulting in phagocytosis of Aβ by microglia and solubilisation of Aβ which is translocated to the vasculature resulting in an increase in the severity of cerebral amyloid angiopathy. “Moth-eaten” plaques are seen at this stage. Stage 2 Plaques have been removed but some dense plaque cores remain; there is marked accumulation of Aβ in the cerebral vasculature, including in cortical capillaries, arteries and arterioles and also leptomeningeal arteries. Microhaemorrhages may occur, probably at this stage. Plaque-associated dystrophic neurites are removed and there is some reduction in the density of neuropil threads, but tangles remain. Stage 3 This is an end stage at which Aβ may have been completely removed from the parenchyma and the vasculature. Tangles and neuropil threads remain, although the neuropil thread density may be reduced. In some cases there are old microvascular lesions, reflecting previous microhaemorrhages
Is there clinical benefit associated with removing Aβ deposits from the brain?
Long-term clinical follow up of the 80 patients who had been immunised in the study showed no evidence of beneficial effects either in terms of survival or time to the development of severe dementia (defined as MMSE ≤ 10) [43]. As this was a clinicopathological study, we were able to match the cognitive function scores with the post mortem neuropathology for some patients. Interestingly, excluding one patient who had died very shortly after immunisation, the cognitive function of all the immunised AD patients had continued to decline and reached a terminal end stage dementia (MMSE = 0) prior to death. This included two patients in whom there was virtually complete clearance of Aβ plaques from the brain [11].
Although based on detailed examination of a small number of patients from a clinical trial which was not powered to study efficacy; the findings seemed to have some inescapable conclusions regarding the role of plaques in the neurodegenerative pathology of AD and in the progressive cognitive decline. Specifically, the findings imply that removal of plaques is not sufficient to halt the progression of neurodegeneration and associated cognitive decline in AD. There are several potential explanations for this observation. Firstly, Aβ plaques may be necessary to initiate, but not necessary to maintain the neurodegenerative mechanism; in this case, the progression of the disease could rely purely on other features of the pathology, either singly or in combination. Possible candidates for progressive neurodegeneration in the absence of plaques are: self-perpetuating tau aggregation [20]; activation of microglia [31, 85] or astrocytes [124]; synaptic degeneration and cerebrovascular pathology, including CAA [120]. Secondly, the studies reported so far are of histologically detectable Aβ plaques and leave open a potential role for non-plaque forms of Aβ (e.g. soluble, oligomeric or intraneuronal Aβ). Indeed, preliminary studies have indicated that levels of oligomeric Aβ are more variable in iAD than in cAD [116] and concentrations of soluble Aβ are remarkably high after immunotherapy [84]. Thirdly, a further logical possibility to explain the continued progression of cognitive decline in AD patients who have been immunised and in whom the plaques have been removed is that, after all, Aβ aggregation is not involved in the causal sequence of events in AD.
Clearly, more remains to be learned in terms of the effects on clinical function of Aβ immunotherapy. Some studies showed evidence of modest benefit in some of the assessment parameters in patients treated with active Aβ42 immunisation (AN1792) [8, 32, 41]. Particularly illuminating will be the cognitive follow up of larger numbers of patients with pre- and post-immunotherapy brain imaging for amyloid plaques, e.g., by use of PIB PET scans, in the larger cohorts of patients in ongoing clinical trials.
Pathological “side effects” associated with removing Aβ
There are several reasons for thinking that there may be risks associated with Aβ immunisation. Indeed, immunisation is performed against a self-protein and as such may initiate an autoimmune disease. In addition, Aβ is a peptide which is normally present in the brain and may have a physiological role, with which immunisation could interfere. Finally, in disaggregating Aβ plaques, the levels of soluble Aβ may be increased which could overload the aged and already compromised cerebral systems by which Aβ is normally removed.
Effects on microglia
Aβ immunotherapy stimulates microglia and targets their activity towards plaques. The evidence for this comes from marked clustering of activated microglia, identified with CD68 and HLA-DR (MHC class II) immunostaining, around plaques and the presence of Aβ within microglial lysosomes [76, 78]. Data from animal and human studies indicate that microglial phagocytosis of Aβ is one of the mechanisms by which Aβ immunotherapy results in plaque removal [10]. The proposed mechanism is that antibodies enter the brain parenchyma from the blood stream, bind to and opsonise Aβ in plaques, thereby prompting phagocytosis by microglia [7, 76]. Whereas plaque removal may be a helpful end result, stimulating microglia in order to remove plaques may also provoke unwanted side effects. Indeed in AD, there is a longstanding literature invoking “neuroinflammation” (i.e. microglial activation) as underlying the continuing neuronal damage [2, 35, 36, 48, 66, 70, 123]. One of the proposals for the role of microglia in AD pathogenesis is that the presence of Aβ deposits in themselves is not harmful, but that the microglial activation provoked in response to Aβ is associated with the release of neurotoxic cytokines. Further stimulation of microglia by Aβ immunotherapy could provoke additional collateral damage as the process of plaque removal is in progress, but conceivably ultimately could result in lowered microglial activation once the plaques have been removed. Our understanding of the overall balance between the beneficial and harmful effects of activated microglia is evolving and seems likely to depend on the precise nature of their activation status [85, 91]. There are clearly unanswered questions here in relation to the precise level and phenotype of microglial activation following Aβ immunotherapy, but it is notable that there is no evidence of an overall accelerated decline in function in AD patients subject to the immunotherapy, which might be predicted if stimulating microglia in this way was particularly neurotoxic.
Effects on CAA
Previous studies have proposed that although the CNS does not have a lymphatic system for the drainage of extracellular fluid, there is an analogous pathway involving the basement membranes of the walls of the vessels forming the cerebral arterial trees [17, 19, 79, 119, 121, 122]. Evidence for the existence of a perivascular drainage pathway includes the observation that soluble substances, such as Indian ink injected into the rodent brain track towards blood vessels, delineating the arterial walls in a pattern similar to that of CAA in humans. A recent study using fluorescent dextran as a soluble tracer, which is of similar molecular weight to monomeric Aβ, colocalises rapidly with the laminin in the vascular basement membranes [17].
Recognition of (a) the concept of the perivascular drainage pathway and (b) that in AD, Aβ42 is located predominantly in cortical plaques whereas CAA is composed predominantly of Aβ40, gives rise to the possibility of tracking the path of plaque Aβ to the vasculature after its mobilisation by Aβ immunotherapy. We found that despite the substantially lower Aβ42 load located in plaques in iAD, overall, the amount of Aβ42 located in the blood vessel walls was many times higher in iAD than in cAD [11]. With the iAD cases available for analysis distributed over a period of many years following immunisation and at different phases of plaque removal, it is possible to envisage a sequence of events in which (a) in cAD, Aβ42 is located mainly in plaques with very little in the vasculature, (b) shortly after immunisation, plaques begin to disaggregate and Aβ42 appears in the blood vessel walls, (c) abundant Aβ42 is present in the walls of blood vessels in cortical regions devoid of plaques and (d) at a late stage in cases with extensive removal of parenchymal Aβ, Aβ42 is ultimately removed from the vasculature [11]. The overall interpretation is that plaque Aβ is solubilised by the therapeutic process, enters the perivascular drainage pathway indicated by increased Aβ42 immunostaining of blood vessel walls and eventually may be cleared from the vasculature. This interpretation is supported by elegant well-controlled experimental studies with multiple pre-determined time points of assessment [88, 126].
The increase in CAA after immunotherapy could be regarded as a beneficial event, indicating that Aβ is draining out of the brain or, alternatively, increased CAA could be viewed as potentially harmful for an aged vasculature. Previous studies of naturally occurring CAA have shown that severe CAA can be associated with large lobar cerebral haemorrhages, presenting with stroke, and cortical microhaemorrhages, associated with rapidly progressing dementia [77]. As far as we are aware, there are no reports of large lobar CAA-related intracerebral haemorrhages after Aβ immunotherapy. However, quantification of microhaemorrhages using Perl’s Prussian stain for iron has shown a substantially higher density of cortical microhaemorrhages and microvascular lesions in some iAD patients compared with cAD [11], as observed in experimental models [86]. It, therefore, appears that Aβ immunotherapy can induce cortical microhaemorrhages, and possibly other forms of microvascular lesions in the AD brain. The clinical implications of this effect, if any, are as yet unclear. Nevertheless, there is an intense interest in this question in the current clinical trials of Aβ immunotherapy in which the occurrence of microhaemorrhages can be documented in vivo by T2 gradient echo MRI scans [34].
Naturally occurring severe CAA has been previously associated with changes in the underlying superficial cerebral white matter. This is thought to occur as a consequence of the anatomical arrangement in which leptomeningeal arteries branch to supply the underlying cerebral cortex and then the superficial white matter. If the leptomeningeal and cortical segments of the arterial tree are affected by severe CAA, then the periarterial spaces in the superficial white matter become dilated [92]. We have identified enlarged perivascular spaces in the superficial cerebral white matter in some of the iAD cases with severe CAA. This observation may have some clinical utility because the size of the periarterial spaces (up to 2–3 mm in diameter) would be visible in vivo on MRI scans. Recognition of this feature as an indirect marker for the presence of severe CAA may be of use in diagnostic imaging as direct methods for imaging CAA in vivo are currently lacking.
Effects on soluble and oligomeric Aβ
One of the proposed mechanisms by which Aβ immunotherapy removes plaques is by Aβ antibody binding to Aβ plaques, resulting in plaque disaggregation with solubilisation of fibrillar Aβ. Direct evidence of this comes from biochemical studies of two cases indicating several fold higher levels of soluble Aβ in the cerebral cortex after immunisation [84]. This supports our interpretation of the cause of the increased severity of the CAA, as described above. Recent studies have suggested that soluble Aβ levels correlate better with cognitive function than plaque load or other parameters of AD pathology [65, 114], consequently, solubilising Aβ plaques by immunotherapy and thereby raising levels of soluble Aβ could potentially be functionally harmful. Nevertheless, as already mentioned, there is no evidence overall that cognitive function is worsened in the immunised AD population. There is intense interest in the role of oligomeric Aβ in AD as the key cause of neurotoxicity [65]. Preliminary studies in iAD cases using Aβ oligomer-specific antibodies have shown an increased variability in the concentration of Aβ oligomers in iAD compared to cAD controls [116]. Interestingly, in a recent post mortem study of patients immunised with AN1792, it was found that plaques remaining after immunotherapy had increased numbers of dystrophic neurites per plaque [101]. This observation was interpreted as consistent with the immunisation process increasing local soluble/oligomeric Aβ with worsening neuritic dystrophy localised to remaining plaques. The effects of immunotherapy on soluble/oligomeric Aβ and the consequences that any such changes may have on function in AD still require further clarification.
Clinical evidence of side effects with the active Aβ42 vaccine
Progress with the active Aβ42 vaccine (AN1792, Elan Pharmaceuticals) came to a halt when it was recognised that a small proportion of patients (6%) developed a subacute neurological deterioration accompanied by the presence of lymphocytes in the cerebrospinal fluid and variable focal white matter abnormalities on imaging [83]. This side effect was interpreted as a form of meningoencephalitis, likely an autoimmune reaction, probably occurring as a result of reformulation of the detergent carrier in the vaccine in order to increase solubility of the Aβ42 in the preparation [89, 98]. Post mortem neuropathology has been reported on two patients who had this complication, the patient we described initially [78] who had been dosed with the reformulated agent in an extension phase to the initial study, and a further Spanish patient from the subsequent trial [26]. Taken together, the main neuropathological features appeared to be, focal abnormalities in the cerebral white matter comprising white matter rarefaction and macrophages, associated with infiltration of T lymphocytes mainly clustered around leptomeningeal blood vessels severely affected by CAA. Although these features seem to be relatively specific for these two patients who presented clinical evidence of this side effect, it should be noted that both patients died many months after the acute clinical event and so the neuropathological features may have changed in that time.
Second generation Aβ immunotherapy approaches and apparent re-emergence of side effects
The clinically evident side effect described above [83] prompted the growing Aβ immunotherapy field to devise a number of immunotherapy protocols with a major aim of avoiding a T lymphocyte response, as this was thought to be responsible. These protocols include the following approaches:
-
1.
Active immunisation with a truncated peptide containing only the N- or C-terminal region of Aβ [104, 107].
-
2.
Passive immunisation which has the advantage of reliability, control of the antibody concentration in the bloodstream and management of the kinetics of Aβ removal [127].
-
3.
Use of pooled immunoglobulins from a large numbers of donors (IVIg) which have anti-inflammatory properties and the capacity to dissolve fibrillar Aβ in vitro [46].
-
4.
Enhancing the “peripheral sink effect” to stop antibodies getting into the brain: This can be achieved by binding Aβ antibodies to large molecules to ensure that they remain in the blood or by inducing production of IgM only, instead of IgG. This methodology generates an alteration in the equilibrium of Aβ across the blood–brain barrier resulting in plaque removal [22–24, 104].
-
5.
Specifically targeting Aβ oligomers rather than fibrillar amyloid using Aβ oligomer-specific antibodies [33].
-
6.
Immunisation early in the disease process: at the stage of mild cognitive impairment or before.
There are currently in the region of 15 second generation Aβ immunotherapy approaches in clinical trials [55], altogether involving many thousands of subjects, and interesting and informative findings are expected to emerge over the next few years. Published data are already available from the first of these studies. The study involved 234 patients (124 treated and 110 placebos) who received passive immunisation with a monoclonal Aβ antibody directed against the N-terminal region of Aβ (Bapineuzumab). Six intravenous infusions were administered 13 weeks apart with the final assessments at week 78. Overall, there was no significant difference in cognitive function between the treated and placebo patients; however, there was a significant benefit in study completers (i.e. patients who completed the protocol to their final assessment) amongst APOE ε4 non-carriers, but not in the APOE ε4 carriers [94]. On the basis of these findings, Bapineuzumab has progressed to a phase III trial (Janssen Alzheimer Immunotherapy Research & Development). However, a side effect was encountered in a small proportion of patients (12/124) who had associated symptoms including headache, confusion, vomiting and gait disturbance. The findings on imaging included FLAIR MRI signal in the white matter, leptomeninges or sulci associated with gyral swelling. This effect was observed with the higher dosage of Bapineuzumab and in APOE ε4 carriers and was resolved after cessation of dosing [94]. The overall findings are somewhat reminiscent of the side effect encountered with AN1792 which is disappointing as passive immunotherapy was supposed to avoid provoking the T cell inflammatory reaction thought to be responsible for the “meningoencephalitis”. This highlights the point that the cause of the side effects encountered with Aβ immunotherapy remains to be fully understood.
Proposed pathophysiological mechanism for the clinical side effects
We propose a pathophysiological mechanism which attempts to draw together the key pieces of information (Fig. 6). The concept is as follows: after Aβ immunisation, Aβ antibodies enter the brain parenchyma and bind to plaques, resulting in solubilisation and mobilisation of Aβ which is translocated to the vasculature. The precise mechanism of Aβ transport, whether in the form of soluble/oligomeric Aβ, or as IgG/Aβ immune complexes or in association with ApoE is not clear at this stage, nevertheless, this results in an increase in the severity of CAA. It is also conceivable that immune complexes deposited in the blood vessel walls activate the complement pathway and provoke an inflammatory response. As a consequence, there is a disturbance of the vascular function resulting in focal abnormalities within their territory of supply, including the underlying white matter. The changes observed in the white matter are due to an altered fluid balance, “vasogenic oedema”, for which the mechanism may be due to impaired perivascular drainage of fluid from the white matter. The relatively common occurrence of these events in APOE ε4 carriers may be due to this group being more likely to have pre-existing CAA as a part of the AD pathology, or/and the association of APOE ε4 with other forms of vascular pathophysiology (i.e. atherosclerosis and arteriosclerosis). In addition, Aβ antibodies may bind to pre-existing CAA and this could conceivably contribute to the vascular effects. The overall implications of this mechanism are that (a) Aβ immunisation induces an iatrogenic process which might be relevant to any Aβ immunotherapy whichever protocol is used; and (b) it may reflect rapid mobilisation of Aβ from plaques, occurs particularly in patients in whom the cerebral vasculature cannot cope with the volume of Aβ traffic due to either pre-existing cerebrovascular disease and/or inflammation related to rapid mobilisation of plaques, and is likely to be associated with increased microglial activation.
It is intriguing to note that a remarkably similar process seems to occur rarely as a natural disease process. Eng and colleagues [25] identified a group of patients with lymphocytic infiltration associated with CAA in whom there were reversible white matter hyperintensities on MRI scans. In addition, Scolding and colleagues [99] observed a similar disease process in which there were perivascular and leptomeningeal CD3+ T cells associated with severe CAA, scarcity of Aβ plaques, presence of Aβ in microglia, accompanied by white matter rarefaction and gliosis, as described above in response to Aβ immunisation. It is tempting to suggest, therefore, that these are patients with AD who have sensitised themselves to the presence of Aβ in their central nervous system and responded in a fashion similar to that subset of immunised AD patients who develop the side effect.
Implications for other neurodegenerative disorders with protein aggregation
Abnormal aggregation of specific proteins is a common feature of many neurodegenerative disorders. Although recognising the protein aggregates has been useful in defining the different disease processes and remains useful in their diagnosis, it is still unclear whether the protein accumulation is a cause or effect of the disease. A powerful way to test the hypothesis that aggregated protein is key to the pathogenesis of these diseases is to manipulate the system. There are a number of examples either from observational studies or after manipulations, both in human and experimental models, in which there is dissociation between the histologically detectable protein accumulation and the neurodegenerative process. These examples would seem to raise the possibility that the histologically detectable protein accumulation is not the cause of the neurodegeneration in these disorders.
Conclusion
AD, in common with other neurodegenerative disorders, is a complex disease process with multiple facets to its neuropathology, each of which may contribute to the overall damage to the brain and consequent dysfunction. Remarkably, it is possible to modify AD pathology by targeting one of those facets, namely Aβ aggregation, by Aβ immunotherapy. However, mobilising Aβ, particularly by use of immunological methods, seems to be associated with side effects at least in a proportion of patients. In addition, as the human brain is notoriously poor at repairing itself after damage, it seems optimistic to expect that a therapy aimed at only one facet of the disease, even if it is involved in initiation of the disease process, may have substantial benefit late in the course of the disease. It is noteworthy that even patients presenting with mild cognitive impairment already at that stage have a substantial burden of Aβ and tau pathology as a result of a process that began many years or even decades before. An intriguing point to consider, on returning to the seminal study of Schenk and colleagues [97], is whether immunotherapy could be used as prevention for AD rather than treatment of established disease. The initial studies showed that Aβ immunisation in young APP transgenic mice prevented the accumulation of Aβ plaques during ageing. It is intriguing to speculate whether this observation would translate to humans: could young or middle-aged humans be safely immunised against Aβ and, if so, would this prevent the formation of Aβ plaques, together with prevention of all of the other features of AD pathology including intraneuronal tau aggregation, loss of synapses and neurons and the glial reaction? It is challenging to envisage how these studies could be performed, but surely this would be the ultimate test of the Aβ cascade hypothesis.
References
Agadjanyan MG, Ghochikyan A, Petrushina I et al (2005) Prototype Alzheimer’s disease vaccine using the immunodominant B cell epitope from beta-amyloid and promiscuous T cell epitope pan HLA DR-binding peptide. J Immunol 174:1580–1586
Akiyama H, Barger S, Barnum S et al (2000) Inflammation and Alzheimer’s disease. Neurobiol Aging 21:383–421
Alaupovic P (1982) The role of apolipoproteins in lipid transport processes. Ric Clin Lab 12:3–21
Asuni AA, Boutajangout A, Quartermain D, Sigurdsson EM (2007) Immunotherapy targeting pathological tau conformers in a tangle mouse model reduces brain pathology with associated functional improvements. J Neurosci 27:9115–9129
Asuni AA, Boutajangout A, Scholtzova H et al (2006) Vaccination of Alzheimer’s model mice with Abeta derivative in alum adjuvant reduces Abeta burden without microhemorrhages. Eur J Neurosci 24:2530–2542
Bard F, Barbour R, Cannon C et al (2003) Epitope and isotype specificities of antibodies to beta-amyloid peptide for protection against Alzheimer’s disease-like neuropathology. Proc Natl Acad Sci USA 100:2023–2028
Bard F, Cannon C, Barbour R et al (2000) Peripherally administered antibodies against amyloid beta-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nat Med 6:916–919
Bayer AJ, Bullock R, Jones RW et al (2005) Evaluation of the safety and immunogenicity of synthetic Abeta42 (AN1792) in patients with AD. Neurology 64:94–101
Boche D, Donald J, Love S et al (2010) Reduction of aggregated Tau in neuronal processes but not in the cell bodies after Abeta42 immunisation in Alzheimer’s disease. Acta Neuropathol 120:13–20
Boche D, Nicoll JA (2008) The role of the immune system in clearance of abeta from the brain. Brain Pathol 18:267–278
Boche D, Zotova E, Weller RO et al (2008) Consequence of Abeta immunization on the vasculature of human Alzheimer’s disease brain. Brain 131:3299–3310
Bombois S, Maurage CA, Gompel M et al (2007) Absence of beta-amyloid deposits after immunization in Alzheimer disease with Lewy body dementia. Arch Neurol 64:583–587
Borchelt DR, Ratovitski T, van Lare J et al (1997) Accelerated amyloid deposition in the brains of transgenic mice coexpressing mutant presenilin 1 and amyloid precursor proteins. Neuron 19:939–945
Boyles JK, Zoellner CD, Anderson LJ et al (1989) A role for apolipoprotein E, apolipoprotein A-I, and low density lipoprotein receptors in cholesterol transport during regeneration and remyelination of the rat sciatic nerve. J Clin Invest 83:1015–1031
Brendza RP, Bacskai BJ, Cirrito JR et al (2005) Anti-Abeta antibody treatment promotes the rapid recovery of amyloid-associated neuritic dystrophy in PDAPP transgenic mice. J Clin Invest 115:428–433
Buttini M, Masliah E, Barbour R et al (2005) Beta-amyloid immunotherapy prevents synaptic degeneration in a mouse model of Alzheimer’s disease. J Neurosci 25:9096–9101
Carare RO, Bernardes-Silva M, Newman TA et al (2008) Solutes, but not cells, drain from the brain parenchyma along basement membranes of capillaries and arteries: significance for cerebral amyloid angiopathy and neuroimmunology. Neuropathol Appl Neurobiol 34:131–144
Chauhan NB (2003) Membrane dynamics, cholesterol homeostasis, and Alzheimer’s disease. J Lipid Res 44:2019–2029
Clapham R, O’Sullivan E, Weller RO, Carare RO (2010) Cervical lymph nodes are found in direct relationship with the internal carotid artery: significance for the lymphatic drainage of the brain. Clin Anat 23:43–47
Clavaguera F, Bolmont T, Crowther RA et al (2009) Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol 11:909–913
Davies CA, Mann DM, Sumpter PQ, Yates PO (1987) A quantitative morphometric analysis of the neuronal and synaptic content of the frontal and temporal cortex in patients with Alzheimer’s disease. J Neurol Sci 78:151–164
DeMattos RB, Bales KR, Cummins DJ et al (2001) Peripheral anti-A beta antibody alters CNS and plasma A beta clearance and decreases brain A beta burden in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci USA 98:8850–8855
DeMattos RB, Bales KR, Cummins DJ, Paul SM, Holtzman DM (2002) Brain to plasma amyloid-beta efflux: a measure of brain amyloid burden in a mouse model of Alzheimer’s disease. Science 295:2264–2267
DeMattos RB, Bales KR, Parsadanian M et al (2002) Plaque-associated disruption of CSF and plasma amyloid-beta (Abeta) equilibrium in a mouse model of Alzheimer’s disease. J Neurochem 81:229–236
Eng JA, Frosch MP, Choi K, Rebeck GW, Greenberg SM (2004) Clinical manifestations of cerebral amyloid angiopathy-related inflammation. Ann Neurol 55:250–256
Ferrer I, Boada Rovira M, Sanchez Guerra ML, Rey MJ, Costa-Jussa F (2004) Neuropathology and pathogenesis of encephalitis following amyloid-beta immunization in Alzheimer’s disease. Brain Pathol 14:11–20
Fidani L, Rooke K, Chartier-Harlin MC et al (1992) Screening for mutations in the open reading frame and promoter of the beta-amyloid precursor protein gene in familial Alzheimer’s disease: identification of a further family with APP717 Val→Ile. Hum Mol Genet 1:165–168
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Games D, Adams D, Alessandrini R et al (1995) Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein. Nature 373:523–527
Games D, Bard F, Grajeda H et al (2000) Prevention and reduction of AD-type pathology in PDAPP mice immunized with A beta 1–42. Ann N Y Acad Sci 920:274–284
Gentleman SM, Leclercq PD, Moyes L et al (2004) Long-term intracerebral inflammatory response after traumatic brain injury. Forensic Sci Int 146:97–104
Gilman S, Koller M, Black RS et al (2005) Clinical effects of Abeta immunization (AN1792) in patients with AD in an interrupted trial. Neurology 64:1553–1562
Gong Y, Chang L, Viola KL et al (2003) Alzheimer’s disease-affected brain: presence of oligomeric A beta ligands (ADDLs) suggests a molecular basis for reversible memory loss. Proc Natl Acad Sci USA 100:10417–10422
Greenberg SM (1998) Cerebral amyloid angiopathy: prospects for clinical diagnosis and treatment. Neurology 51:690–694
Griffin WS (2006) Inflammation and neurodegenerative diseases. Am J Clin Nutr 83:470S–474S
Griffin WS, Sheng JG, Royston MC et al (1998) Glial-neuronal interactions in Alzheimer’s disease: the potential role of a ‘cytokine cycle’ in disease progression. Brain Pathol 8:65–72
Haltia M, Viitanen M, Sulkava R et al (1994) Chromosome 14-encoded Alzheimer’s disease: genetic and clinicopathological description. Ann Neurol 36:362–367
Hardy J, Allsop D (1991) Amyloid deposition as the central event in the aetiology of Alzheimer’s disease. Trends Pharmacol Sci 12:383–388
Hardy J, Selkoe DJ (2002) The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297:353–356
Heston LL, Mastri AR (1977) The genetics of Alzheimer’s disease: associations with hematologic malignancy and Down’s syndrome. Arch Gen Psychiatry 34:976–981
Hock C, Konietzko U, Streffer JR et al (2003) Antibodies against beta-amyloid slow cognitive decline in Alzheimer’s disease. Neuron 38:547–554
Holcomb L, Gordon MN, McGowan E et al (1998) Accelerated Alzheimer-type phenotype in transgenic mice carrying both mutant amyloid precursor protein and presenilin 1 transgenes. Nat Med 4:97–100
Holmes C, Boche D, Wilkinson D et al (2008) Long term effect of Abeta42 immunization in Alzheimer’s disease: follow-up of a randomised, placebo-controlled phase I trial. Lancet 372:216–223
Holtzman DM, Bales KR, Wu S et al (1999) Expression of human apolipoprotein E reduces amyloid-beta deposition in a mouse model of Alzheimer’s disease. J Clin Invest 103:R15–R21
Hsiao K, Chapman P, Nilsen S et al (1996) Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. Science 274:99–102
Istrin G, Bosis E, Solomon B (2006) Intravenous immunoglobulin enhances the clearance of fibrillar amyloid-beta peptide. J Neurosci Res 84:434–443
Janus C, Pearson J, McLaurin J et al (2000) Abeta peptide immunization reduces behavioural impairment and plaques in a model of Alzheimer’s disease. Nature 408:979–982
Kalaria RN (1999) Microglia and Alzheimer’s disease. Curr Opin Hematol 6:15–24
Karlinsky H, Vaula G, Haines JL et al (1992) Molecular and prospective phenotypic characterization of a pedigree with familial Alzheimer’s disease and a missense mutation in codon 717 of the beta-amyloid precursor protein gene. Neurology 42:1445–1453
Kim HD, Cao Y, Kong FK et al (2005) Induction of a Th2 immune response by co-administration of recombinant adenovirus vectors encoding amyloid beta-protein and GM-CSF. Vaccine 23:2977–2986
Korwek KM, Trotter JH, Ladu MJ, Sullivan PM, Weeber EJ (2009) ApoE isoform-dependent changes in hippocampal synaptic function. Mol Neurodegener 4:21
Krugers HJ, Mulder M, Korf J et al (1997) Altered synaptic plasticity in hippocampal CA1 area of apolipoprotein E deficient mice. Neuroreport 8:2505–2510
Lassmann H (1996) Patterns of synaptic and nerve cell pathology in Alzheimer’s disease. Behav Brain Res 78:9–14
Lee SJ, Liyanage U, Bickel PE et al (1998) A detergent-insoluble membrane compartment contains A beta in vivo. Nat Med 4:730–734
Lemere CA, Masliah E (2010) Can Alzheimer disease be prevented by amyloid-beta immunotherapy? Nat Rev Neurol 6:108–119
Lemere CA, Spooner ET, LaFrancois J et al (2003) Evidence for peripheral clearance of cerebral Abeta protein following chronic, active Abeta immunization in PSAPP mice. Neurobiol Dis 14:10–18
Levi O, Lutjohann D, Devir A et al (2005) Regulation of hippocampal cholesterol metabolism by apoE and environmental stimulation. J Neurochem 95:987–997
Lombardo JA, Stern EA, McLellan ME et al (2003) Amyloid-beta antibody treatment leads to rapid normalization of plaque-induced neuritic alterations. J Neurosci 23:10879–10883
Lowe J, Mirra SS, Hyman BT, Dickson DW (2008) Ageing and dementia. In: Love S, Louis DN, Ellison DW (eds) Greenfield’s neuropathology, 8th edn. Edward Arnold Ltd, London, pp 1031–1152
Manea M, Mezo G, Hudecz F, Przybylski M (2004) Polypeptide conjugates comprising a beta-amyloid plaque-specific epitope as new vaccine structures against Alzheimer’s disease. Biopolymers 76:503–511
Masliah E (1995) Mechanisms of synaptic dysfunction in Alzheimer’s disease. Histol Histopathol 10:509–519
Masliah E, Hansen L, Adame A et al (2005) Abeta vaccination effects on plaque pathology in the absence of encephalitis in Alzheimer disease. Neurology 64:129–131
Masliah E, Terry RD, Alford M, DeTeresa R, Hansen LA (1991) Cortical and subcortical patterns of synaptophysin like immunoreactivity in Alzheimer’s disease. Am J Pathol 138:235–246
Mauch DH, Nagler K, Schumacher S et al (2001) CNS synaptogenesis promoted by glia-derived cholesterol. Science 294:1354–1357
McDonald JM, Savva GM, Brayne C et al (2010) The presence of sodium dodecyl sulphate-stable Abeta dimers is strongly associated with Alzheimer-type dementia. Brain 133:1328–1341
McGeer PL, Itagaki S, Tago H, McGeer EG (1987) Reactive microglia in patients with senile dementia of the Alzheimer type are positive for the histocompatibility glycoprotein HLA-DR. Neurosci Lett 79:195–200
McLaurin J, Cecal R, Kierstead ME et al (2002) Therapeutically effective antibodies against amyloid-beta peptide target amyloid-beta residues 4–10 and inhibit cytotoxicity and fibrillogenesis. Nat Med 8:1263–1269
Morgan D, Diamond DM, Gottschall PE et al (2000) A beta peptide vaccination prevents memory loss in an animal model of Alzheimer’s disease. Nature 408:982–985
Mouri A, Noda Y, Hara H et al (2007) Oral vaccination with a viral vector containing Abeta cDNA attenuates age-related Abeta accumulation and memory deficits without causing inflammation in a mouse Alzheimer model. FASEB J 21:2135–2148
Mrak RE, Griffin WS (2005) Glia and their cytokines in progression of neurodegeneration. Neurobiol Aging 26:349–354
Mullan M, Crawford F, Axelman K et al (1992) A pathogenic mutation for probable Alzheimer’s disease in the APP gene at the N-terminus of beta-amyloid. Nat Genet 1:345–347
Mullan M, Houlden H, Windelspecht M et al (1992) A locus for familial early-onset Alzheimer’s disease on the long arm of chromosome 14, proximal to the alpha 1-antichymotrypsin gene. Nat Genet 2:340–342
Naruse S, Igarashi S, Kobayashi H et al (1991) Mis-sense mutation Val–Ile in exon 17 of amyloid precursor protein gene in Japanese familial Alzheimer’s disease. Lancet 337:978–979
Nelson PT, Braak H, Markesbery WR (2009) Neuropathology and cognitive impairment in Alzheimer disease: a complex but coherent relationship. J Neuropathol Exp Neurol 68:1–14
Nichol K, Deeny SP, Seif J, Camaclang K, Cotman CW (2009) Exercise improves cognition and hippocampal plasticity in APOE epsilon4 mice. Alzheimer’s Dement 5:287–294
Nicoll JA, Barton E, Boche D et al (2006) Abeta species removal after Abeta42 immunization. J Neuropathol Exp Neurol 65:1040–1048
Nicoll JA, McCarron MO (2001) APOE gene polymorphism as a risk factor for cerebral amyloid angiopathy-related hemorrhage. Amyloid 8(Suppl 1):51–55
Nicoll JA, Wilkinson D, Holmes C et al (2003) Neuropathology of human Alzheimer disease after immunization with amyloid-beta peptide: a case report. Nat Med 9:448–452
Nicoll JA, Yamada M, Frackowiak J, Mazur-Kolecka B, Weller RO (2004) Cerebral amyloid angiopathy plays a direct role in the pathogenesis of Alzheimer’s disease. Pro-CAA position statement. Neurobiol Aging 25:589–597 (discussion 603–604)
Nwosu I, Gairhe S, Struble RG, Nathan BP (2008) Impact of apoE deficiency during synaptic remodeling in the mouse olfactory bulb. Neurosci Lett 441:282–285
Oddo S, Vasilevko V, Caccamo A et al (2006) Reduction of soluble Abeta and tau, but not soluble Abeta alone, ameliorates cognitive decline in transgenic mice with plaques and tangles. J Biol Chem 281:39413–39423
Oh JY, Nam YJ, Jo A et al (2010) Apolipoprotein (APOE) mRNA is transported to dendrites and may have a role in synaptic structural plasticity. J Neurochem [Epub ahead of print] 2010 April 28. doi:10.1111/j.1471-4159.2010.06773
Orgogozo JM, Gilman S, Dartigues JF et al (2003) Subacute meningoencephalitis in a subset of patients with AD after Abeta42 immunization. Neurology 61:46–54
Patton RL, Kalback WM, Esh CL et al (2006) Amyloid-beta peptide remnants in AN-1792-immunized Alzheimer’s disease patients: a biochemical analysis. Am J Pathol 169:1048–1063
Perry VH, Nicoll JA, Holmes C (2010) Microglia in neurodegenerative disease. Nat Rev Neurol 6:193–201
Pfeifer M, Boncristiano S, Bondolfi L et al (2002) Cerebral hemorrhage after passive anti-Abeta immunotherapy. Science 298:1379
Poirier J (2000) Apolipoprotein E and Alzheimer’s disease. A role in amyloid catabolism. Ann N Y Acad Sci 924:81–90
Prada CM, Garcia-Alloza M, Betensky RA et al (2007) Antibody-mediated clearance of amyloid-beta peptide from cerebral amyloid angiopathy revealed by quantitative in vivo imaging. J Neurosci 27:1973–1980
Pride M, Seubert P, Grundman M et al (2008) Progress in the active immunotherapeutic approach to Alzheimer’s disease: clinical investigations into AN1792-associated meningoencephalitis. Neurodegener Dis 5:194–196
Qu B, Rosenberg RN, Li L, Boyer PJ, Johnston SA (2004) Gene vaccination to bias the immune response to amyloid-beta peptide as therapy for Alzheimer disease. Arch Neurol 61:1859–1864
Ransohoff RM, Perry VH (2009) Microglial physiology: unique stimuli, specialized responses. Annu Rev Immunol 27:119–145
Roher AE, Kuo YM, Esh C et al (2003) Cortical and leptomeningeal cerebrovascular amyloid and white matter pathology in Alzheimer’s disease. Mol Med 9:112–122
Rovelet-Lecrux A, Hannequin D, Raux G et al (2006) APP locus duplication causes autosomal dominant early-onset Alzheimer disease with cerebral amyloid angiopathy. Nat Genet 38:24–26
Salloway S, Sperling R, Gilman S et al (2009) A phase 2 multiple ascending dose trial of bapineuzumab in mild to moderate Alzheimer disease. Neurology 73:2061–2070
Sato N, Imaizumi K, Manabe T et al (2001) Increased production of beta-amyloid and vulnerability to endoplasmic reticulum stress by an aberrant spliced form of presenilin 2. J Biol Chem 276:2108–2114
Schellenberg GD, Bird TD, Wijsman EM et al (1992) Genetic linkage evidence for a familial Alzheimer’s disease locus on chromosome 14. Science 258:668–671
Schenk D, Barbour R, Dunn W et al (1999) Immunization with amyloid-beta attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature 400:173–177
Schenk D, Hagen M, Seubert P (2004) Current progress in beta-amyloid immunotherapy. Curr Opin Immunol 16:599–606
Scolding NJ, Joseph F, Kirby PA et al (2005) Abeta-related angiitis: primary angiitis of the central nervous system associated with cerebral amyloid angiopathy. Brain 128:500–515
Selkoe DJ (2002) Alzheimer’s disease is a synaptic failure. Science 298:789–791
Serrano-Pozo A, Williams MW, Ferrer I et al (2010) Beneficial effect of human anti-Aβ active immunization on neurite morphology and tau pathology. Brain 133:1312–1327
Shankar GM, Bloodgood BL, Townsend M et al (2007) Natural oligomers of the Alzheimer amyloid-beta protein induce reversible synapse loss by modulating an NMDA-type glutamate receptor-dependent signaling pathway. J Neurosci 27:2866–2875
Sigurdsson EM (2009) Tau-focused immunotherapy for Alzheimer’s disease and related tauopathies. Curr Alzheimer Res 6:446–450
Sigurdsson EM, Knudsen E, Asuni A et al (2004) An attenuated immune response is sufficient to enhance cognition in an Alzheimer’s disease mouse model immunized with amyloid-beta derivatives. J Neurosci 24:6277–6282
Sigurdsson EM, Scholtzova H, Mehta PD, Frangione B, Wisniewski T (2001) Immunization with a nontoxic/nonfibrillar amyloid-beta homologous peptide reduces Alzheimer’s disease-associated pathology in transgenic mice. Am J Pathol 159:439–447
Sleegers K, Brouwers N, Gijselinck I et al (2006) APP duplication is sufficient to cause early onset Alzheimer’s dementia with cerebral amyloid angiopathy. Brain 129:2977–2983
Solomon B, Koppel R, Frankel D, Hanan-Aharon E (1997) Disaggregation of Alzheimer beta-amyloid by site-directed mAb. Proc Natl Acad Sci USA 94:4109–4112
Sorbi S, Nacmias B, Forleo P et al (1993) APP717 and Alzheimer’s disease in Italy. Nat Genet 4:10
St George-Hyslop PH, Tanzi RE, Polinsky RJ et al (1987) The genetic defect causing familial Alzheimer’s disease maps on chromosome 21. Science 235:885–890
Strittmatter WJ, Saunders AM, Schmechel D et al (1993) Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci USA 90:1977–1981
Sturchler-Pierrat C, Abramowski D, Duke M et al (1997) Two amyloid precursor protein transgenic mouse models with Alzheimer disease-like pathology. Proc Natl Acad Sci USA 94:13287–13292
Sze CI, Troncoso JC, Kawas C et al (1997) Loss of the presynaptic vesicle protein synaptophysin in hippocampus correlates with cognitive decline in Alzheimer disease. J Neuropathol Exp Neurol 56:933–944
Terry RD, Masliah E, Salmon DP et al (1991) Physical basis of cognitive alterations in Alzheimer’s disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol 30:572–580
Tomic JL, Pensalfini A, Head E, Glabe CG (2009) Soluble fibrillar oligomer levels are elevated in Alzheimer’s disease brain and correlate with cognitive dysfunction. Neurobiol Dis 35:352–358
Van Broeckhoven C, Backhovens H, Cruts M et al (1992) Mapping of a gene predisposing to early-onset Alzheimer’s disease to chromosome 14q24.3. Nat Genet 2:335–339
van Helmond Z, Boche D, Nicoll J et al (2009) Oligomeric A beta levels following A beta(42) immunisation. Neuropathol Appl Neurobiol 35:25
Veinbergs I, Jung MW, Young SJ et al (1998) Altered long-term potentiation in the hippocampus of apolipoprotein E-deficient mice. Neurosci Lett 249:71–74
Walsh DM, Klyubin I, Fadeeva JV et al (2002) Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature 416:535–539
Weller RO (2005) Drainage pathways of CSF and interstitial fluid. In: Kalimo H (ed) Cerebrovascular diseases. ISN Neuropath Press, Basel, pp 50–55
Weller RO, Boche D, Nicoll JA (2009) Microvasculature changes and cerebral amyloid angiopathy in Alzheimer’s disease and their potential impact on therapy. Acta Neuropathol 118:87–102
Weller RO, Djuanda E, Yow HY, Carare RO (2009) Lymphatic drainage of the brain and the pathophysiology of neurological disease. Acta Neuropathol 117:1–14
Weller RO, Galea I, Carare RO, Minagar A (2009) Pathophysiology of the lymphatic drainage of the central nervous system: implications for pathogenesis and therapy of multiple sclerosis. Pathophysiology [Epub ahead of print] 2009 Nov 30. doi:10.1016/j.pathophys.2009.10.007
Weninger SC, Yankner BA (2001) Inflammation and Alzheimer disease: the good, the bad, and the ugly. Nat Med 7:527–528
Wharton SB, O’Callaghan JP, Savva GM et al (2009) Population variation in glial fibrillary acidic protein levels in brain ageing: relationship to Alzheimer-type pathology and dementia. Dement Geriatr Cogn Disord 27:465–473
Wilcock DM, Gharkholonarehe N, Van Nostrand WE et al (2009) Amyloid reduction by amyloid-beta vaccination also reduces mouse tau pathology and protects from neuron loss in two mouse models of Alzheimer’s disease. J Neurosci 29:7957–7965
Wilcock DM, Rojiani A, Rosenthal A et al (2004) Passive immunotherapy against Abeta in aged APP-transgenic mice reverses cognitive deficits and depletes parenchymal amyloid deposits in spite of increased vascular amyloid and microhemorrhage. J Neuroinflamm 1:24
Wisniewski T, Konietzko U (2008) Amyloid-beta immunisation for Alzheimer’s disease. Lancet Neurol 7:805–811
Wolfe MS, De Los Angeles J, Miller DD, Xia W, Selkoe DJ (1999) Are presenilins intramembrane-cleaving proteases? Implications for the molecular mechanism of Alzheimer’s disease. Biochemistry 38:11223–11230
Yoshioka K, Miki T, Katsuya T, Ogihara T, Sakaki Y (1991) The 717Val–Ile substitution in amyloid precursor protein is associated with familial Alzheimer’s disease regardless of ethnic groups. Biochem Biophys Res Commun 178:1141–1146
Zetterberg H, Mattsson N, Shaw LM, Blennow K (2010) Biochemical markers in Alzheimer’s disease clinical trials. Biomark Med 4:91–98
Acknowledgments
We thank the patients who were involved in this study and their carers. Vivienne Hopkins, David Wilkinson, Anthony Bayer, Roy Jones and Roger Bullock enrolled patients in the original trial and facilitated subsequent follow up of the patients. The Neuropathology Section, Department of Cellular Pathology, Southampton University Hospitals NHS Trust and the Histopathology Research Unit and Biomedical Research Unit of the School of Medicine, University of Southampton and Miss Elina Zotova facilitated tissue analysis. Staff at Elan Pharmaceuticals made available original clinical trial data. The studies were funded by the Alzheimer Research Trust (JARN, DB, CH: ART/PG2006/4) and the Medical Research Council (DB: G0501033).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boche, D., Denham, N., Holmes, C. et al. Neuropathology after active Aβ42 immunotherapy: implications for Alzheimer’s disease pathogenesis. Acta Neuropathol 120, 369–384 (2010). https://doi.org/10.1007/s00401-010-0719-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-010-0719-5