Abstract
Amyloid-β-protein (Aβ) is generally assessed by neuropathologists in diagnostics. This BrainNet Europe (http://www.brainnet-europe.org/) (15 centres and 26 participants) study was carried out to investigate the reliability of such an assessment. In the first part of this trial, tissue microarray sections were stained with the antibody of each centre’s choice. Reflecting the reality, seven antibodies and a plethora of pretreatment strategies were used. Ninety-two percent of the stainings were of good/acceptable quality and the estimation of presence of Aβ aggregates yielded good results. However, a poor agreement was reached particularly regarding quantitative (density) and qualitative (diffuse/cored plaques) results. During a joint meeting, the clone 4G8 was determined to label best the fleecy/diffuse plaques, and thus, this clone and the formic acid pretreatment technique were selected for the second part of this study. Subsequently, all stained sections were of good/acceptable quality and again a high level of concordance of the dichotomized (presence/absence) assessment of plaques and CAA was achieved. However, even when only one antibody was used, the type of Aβ-aggregates (diffuse/cored), type of vessel and Vonsattel grade, were not reliably assigned. Furthermore, the quantification of lesions was far from reliable. In line with the first trial, the agreement while assessing density (some, moderate and many) was unimpressive. In conclusion, we can confirm the utility of immunohistochemical detection of Aβ-protein in diagnostics and research. It is noteworthy that to reach reproducible results a dichotomized assessment of Aβ-immunoreactivity rather than quantification and assignment of various types of lesions should be applied, particularly when comparing results obtained by different neuropathologists.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracellular deposition of β-amyloid (Aβ) protein is frequently seen in the brains of aged and demented subjects [2, 6]. The Aβ is a 39–43 amino acid peptide resulting from β- and γ-secretase cleavage of the amyloid precursor protein [12]. Aβ deposits are seen as fleecy, diffuse or dense/cored plaques [10, 18, 22, 28] and Aβ deposits are also often observed in the walls of brain vessels, i.e. cerebral amyloid angiopathy (CAA) [24, 27, 32]. Furthermore, two recent review articles have summarized emerging evidence that this peptide can also accumulate intracellularly [11, 21]. Thus, the assessment of Aβ in the brain samples obtained from both diseased as well as neurologically unimpaired subjects [31] has become an important facet of diagnostic practice.
Prior to the era of immunohistochemistry (IHC), relatively unspecific chemical stains such as alkaline Congo red, crystal violet method and thioflavin S were used in order to detect Aβ deposits [7, 8, 13]. Currently, Aβ aggregates are commonly detected in the brain tissue by applying IHC methods. A large variety of commercial and self-made Aβ antibodies with a range of sensitivities and specificities are currently in use. Consequently, differing results may be obtained depending not only on the antibody used but also from the pretreatment strategy and detection system applied. Variability in resulting IHC stains has recently been assessed with regard to other proteins such as α-synuclein [4, 9]. It is surprising that as far as we are aware, only one study has evaluated the reproducibility of Aβ-IHC in an inter-laboratory setting. This ‘pilot’ BrainNet Europe (BNE) inter-laboratory study, including 17 neuropathologists, revealed several pitfalls when applying Aβ-IHC [3]. As many as 29% of the stainings produced were of poor quality, and moreover, even when only the good/acceptable stainings were compared, the evaluations of the load of Aβ still significantly varied [3].
The BNE consortium has carried out several tissue microarray (TMA) technique-based [16, 20, 30] inter-laboratory comparison surveys that have allowed participant laboratories to assess their proficiencies with various IHC stainings [3, 4, 17]. This present BNE inter-laboratory study was designed to evaluate the reliability of the assessment of Aβ-immunoreactive (IR) aggregates in brain samples when viewed by experienced neuropathologists. This study consisted of an assessment of the routine techniques currently followed by each centre, i.e. the first trial and subsequently an assessment of the results when only one antibody was used, i.e. the second trial. This report summarizes the results obtained when 26 evaluators from 15 centres assessed the Aβ-IR aggregates in TMA core samples (2-mm Ø) using IHC methodology.
Materials and methods
Construction of TMA blocks and sectioning
The flowchart delineates the logistics of this study (Fig. 1). Construction of TMA blocks was carried out as described earlier [3, 17]. The demographic of the subjects from whom the tissue was obtained and the details regarding brain samples are given in Supplementary table 1. Briefly, the age at death of the subjects (10 females and 13 males) ranged from 58 to 88 years. The post-mortem delay varied from 3 h to 4 days, the fixation time from 1 day to 5 years, the maximum temperature of the embedding medium ranged from 56 to 63°C and the storage duration for the blocks ranged from 1 day to 10 years.
Assessment of comparability of TMA sections
Prior to distribution of TMA sections to the participants, the uniformity/comparability of the sections, i.e. cores, was assessed by the co-ordinating centre. Briefly, every tenth TMA section (n = 10 in TMA1, n = 11 in TMA2) was pretreated with 80% formic acid for 1 h and stained using a monoclonal antibody to Aβ (clone 4G8, Signet Laboratories, Dedham, MA, USA) at a dilution of 1:2,000. Every fifth core in each TMA section was assessed with respect to the density and number of Aβ-IR plaques, and number of vessels exhibiting CAA.
BNE participant efforts
The BNE participant efforts in trials 1 and 2 are summarized in Fig. 1. Briefly, in the first trial, the slides were to be stained by using the participant’s own choice of antibody directed to Aβ without strict methodological recommendations. Results obtained were discussed at a joint meeting and the difficulties observed during the assessments were summarized. At this meeting, the antibody to be used in the second part of the trial was agreed upon. The assessment instructions including figures, references for the assessments of vascular pathology [27, 28, 32] and data sheets for recording of the assessments, were the same in both trials and are summarized in Fig. 2.
a Summary of the assessment instructions, and b an example of the recording sheet. Abbreviations: Aβ+ β-amyloid-immunoreactivity, cAβ+ cored β-amyloid-positive plaques, dAβ+ diffuse β-amyloid-positive plaques (including lake-like, subpial band-like and fleecy β-amyloid-immunoreactivities), CAA cerebral amyloid angiopathy
Assessment of Aβ-IR aggregates
As described in Fig. 2, a variety of Aβ-IR structures was to be assessed in both trials (Fig. 2). Briefly, the evaluators were expected to provide a dichotomized assessment, that is, determination of the absence or presence of the background staining and Aβ-IR in general (i.e. all types of plaques, CAA, labeled cells, etc.). Furthermore, Aβ-IR diffuse plaques, cored plaques, neurons, glial cells, CAA, arteries, veins and capillaries were to be assessed in a dichotomized manner. In addition, a count (0 → > 20) and also an estimate of the density (0 = none; 1 = some ∼ 10; 2 = moderate ∼ 40 and 3 = many ∼ 100), see Panel b in Fig. 2a) of plaques were to be included. With respect to Aβ-IR CAA, the evaluators were also asked to count vessels exhibiting CAA (0 → >20) and Vonsattel grading of CAA (0 → 3, see Fig. 2).
Data analysis at the co-ordinating centre
The sections stained by the participating BNE centres were evaluated with respect to loss and damage to cores and with respect to quality of staining on a scale incorporating both staining intensity and background staining (good, acceptable and poor). Briefly, in good stainings, the staining clearly labelled the lesion evenly in most of the core samples in a TMA section, whereas in acceptable stainings, lesions were detectable but the intensity of staining between the cores varied with regard to the lesions and/or background. The staining was assessed as poor when the lesions were not at all detectable in some of the core samples.
In both trials, results obtained from different participants were compared either at the core sample level (core-to-core comparison) or at the TMA section level (Fig. 3) when poor stainings were excluded.
A schematic presentation of the data analysis. At the core sample level, i.e. core-to-core comparison the same core (example A 1) was compared in consecutive sections stained by participants. At the TMA section level, all cores in consecutive sections stained by participants were compared. TMA tissue microarray, CAA cerebral amyloid angiopathy, Aβ-IR β-amyloid-immunoreactivity
On the basis of the comments received from the joint meeting that was held after the first trial, a re-assessment of the density of plaques was carried out at the co-ordinating centre.
Statistical analysis and photomicrography
SPSS program for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analyses. The average statistical differences in the comparability of the shipped sections were estimated by a non-parametric Kruskal–Wallis (K–W) test. The average statistical differences between the assessments of IR structures at the TMA section level (and also between re-assessments of the density of plaques) were estimated by the non-parametric K–W test (Fig. 3). A non-parametric Wilcoxon test and a value of absolute agreement (%) (i.e., the proportion of core samples assessed equivalently in the primary and re-assessments), both, were used to estimate statistical differences between the primary and re-assessments of the density of plaques. At the core sample level, the proportion of the most frequent score (for the counts and density of Aβ-IR plaques, counts of vessels exhibiting CAA and for the Vonsattel grades) was calculated (Fig. 3).
Digital images were taken using an Olympus BX40 microscope equipped with an Olympus DP50 microscope digital camera system (Olympus Optical Co., Ltd., Tokyo, Japan).
Results
Comparability of consecutive sections
The density and number of Aβ-IR plaques and the number of vessels exhibiting CAA were assessed for the representative 10 TMA sections in both TMA1 and TMA2, and the results did not differ significantly (TMA1: K–W test, P = 0.437 for all parameters; TMA2: K–W test, P = 0.995, P = 0.981, P = 0.999, respectively), i.e. in the consecutive sections, the corresponding cores (Fig. 3) displayed similar number of lesions.
Result in the first trial, i.e. current IHC practices
There were 47 cores in the TMA1 sections (Fig. 1, Supplementary table 1) and altogether, the co-ordinating centre received 24 stainings and assessments from 15 BNE centres.
Quality of staining. The participants had used seven different antibodies with a variety of IHC methods (Fig. 4, Supplementary table 2). In general, the intensity of IR structures, both plaques and CAA, varied notably between the different stainings. The intensity of IR varied also between the core samples within a TMA section in some of the stainings. When clone 6F3D was used, the vessels exhibiting CAA were often more intensively detected than the plaques; in particular, the diffuse plaques were only faintly stained or undetectable. It is noteworthy that some of the antibodies visualized intracellular labelling more efficiently than others. It was noted also that while using one and the same antibody, the staining quality seemed to be influenced by the IHC practice used, in particular, the pretreatment strategy. For example, while using clone 6F3D, the staining clearly required tissue section pretreatment with formic acid, and thus pressure cooker alone (staining/assessment code #10) was not sufficient for epitope unmasking. The staining was assessed as good (staining clearly labelled the lesions in most of the core samples in a TMA section) in 50% (12/24), acceptable (some variability of labelling of lesions was seen) in 42% (10/24), and poor (some core samples remained negative) in two stainings (Fig. 5, Supplementary table 2). In majority of stainings as well as in the majority of core samples, there was no disturbing background staining. However, regardless of which antibody was used, in two of the core samples (cores 47 and 48) intensive background staining was detected quite frequently (Fig. 6). These cores were taken from a block that had been fixed for 1 day in AFA (5% acetic acid glacial, 0.8% formalin, 75% alcohol, 19.2% H2O, Eosin) and subsequently the block was placed in formic acid prior to paraffin embedding (Supplementary table 1).
Physiological cleavage of β-amyloid peptide and a schematic presentation of the epitopes of antibodies that were used in this study. Clone 6E10 is raised against, i.e. immunogen Aβ1–17 (Signet) and recognizes amino acid residues, i.e. epitope Aβ4–9 (Signet), Aβ5–11 [1] or Aβ4–13 [19, 29]; clone 6F3D immunogen Aβ8–17 (DakoCytomation) and epitope Aβ9–14 (DakoCytomation), Aβ10–15 [1] or Aβ9–14 [23]; clone 4G8 (Signet) immunogen Aβ17–24 and epitope Aβ18–22 (Signet), Aβ17–21 [23] or Aβ18–20 [1]; clone 1E8 immunogen Aβ17–23 [5]. The specificity of polyclonal antibodies as given by the producer
Note variable background staining in the same core sample (brain sample 22) when two participants used clone 4G8 for the visualization of β-amyloid-immunoreactivity: a staining #14, and b staining #16. In these two stainings, the pre-treatment strategy, dilution and detection system varied (original magnification, ×40)
When not otherwise stated, results below include only assessments of slides of good/acceptable quality.
Aβ-IR plaques: determination of the presence or absence. Most of the antibodies used labelled diffuse plaques in 45 of the 47 core samples (only CAA was seen in cores 30 and 31). In majority of these 45 core samples, all stainings revealed diffuse plaques (33/45 cores, 75%). In the remaining 12 core samples (cores 11–12, 21–23, 26, and 43–48), diffuse plaques were frequently missing in six of the stainings [clone 6E10: #19; clone 6F/3D: #6, 7; clone 4G8: #13, 14 and polyclonal antibody (pAb) 44–136: #23]. In contrast, cored plaques were seen in only 16% of the 45 core samples (7/45), independent of the antibody used. It is noteworthy that when applying only 1- to 3-min pretreatment with formic acid (#1, 5, 11, 16, 17, and 20), some of the cores did not display any cored plaques.
Aβ-IR plaques; counts and density (independent of plaque type). Detailed results are given in Table 1. At the TMA section level, the counts (0 to >20) of plaques differed significantly (K–W test, P = 0.001) between the BNE participants when applying different stainings, with the mean values (±SE) ranging from 19.9 ± 0.6 to 14.9 ± 1.1. It is noteworthy that, when only stainings of good quality were included the difference was not significant (K–W test, P = 0.181). The assessments of the density (0; 1, some ∼ 10; 2, moderate ∼ 40; 3, many ∼ 100) of plaques differed significantly between the BNE participants when applying different stainings, both when stainings of good/acceptable or only good quality were included (K–W test, P = 0.000 and P = 0.001, respectively).
Aβ-IR CAA: dichotomized assessment. CAA was seen, at least in some of the stainings, in 45 of the 47 core samples and in two of the cores; only CAA without plaques was seen (cores 30 and 31). CAA was seen in 36% of the core samples (17/47) in all stainings. Two cores were repeatedly positive regarding CAA and two cores were repeatedly negative. In 60% of core samples, the evaluators disagreed in the assessment of the CAA.
Aβ-IR CAA: counts and Vonsattel grade. At the TMA section level, the results of the counts (0 to >20) of vessels exhibiting CAA did not differ significantly (K–W test, P = 0.600) between the BNE participants when applying different stainings, with the mean values (±SE) ranging from 8.7 ± 1.2 to 5.0 ± 1.0 (Table 1). In addition, the assessments of the Vonsattel grade of CAA did not differ significantly (K–W test, P = 0.261) between the BNE participants when applying different stainings, with the mean values (±SE) ranging from 1.3 ± 0.1 to 0.7 ± 0.1 (Table 1).
Aβ-IR arteries, veins and capillaries. CAA was never detected in the arteries in 28% (13/47), in the veins in 21% (10/47), and in the capillaries in 6% (3/47) of the core samples. Most evaluators (75–100%) had observed CAA in the arteries, veins or capillaries in 35% (12/34), 22% (8/37) and in 9% (4/44) of the core samples, respectively.
Cellular Aβ-IR. Aβ-IR cells were detected in each core of the TMA1 sections, at least with some of the antibodies used. The number of cores with IR cells depended, however, on both the antibody and the pretreatment strategy used. When using clone 4G8, all evaluators had always seen labelled cells in 34% of core samples (16/47) and also in the majority of the remaining 31 cores and more than 75% of the evaluators had seen labelled cells. In contrast to the situation with clone 4G8, while using clones 6F3D and 6E10, the assessment of the presence of IR cells varied significantly.
Selection of antibody and pretreatment strategy for the second trial
In the first trial, while using clone 4G8, the staining results were good and/or acceptable in 83% of the stainings. Furthermore, it was noted that the fleecy Aβ aggregates were readily labelled with this antibody. Thus, clone 4G8 and a pretreatment strategy utilizing formic acid were consequently chosen for the second trial. Details of the staining methods applied by the participants in the second trial are listed in Supplementary table 3.
During the joint meeting after the first trial, it became evident that several of the evaluators had experienced difficulties in assessing the density of plaques (0, 1 = some ∼ 10, 2 = moderate ∼ 40, 3 = many ∼ 100). Thus, in the second trial, a reassessment of the density of plaques was carried out by the co-ordinating centre.
Results in the second trial, i.e. with harmonized IHC methodology
There were 35 core samples in the TMA2 sections (Fig. 1, Supplementary table 1) and altogether, the co-ordinating centre received 21 assessments from 13 BNE centres. Nineteen sections of these 21 were available for evaluation and reassessment by the co-ordinating centre.
Quality of staining. The quality of staining was assessed as being good in 18 of the 19 stainings obtained for re-assessments (Supplementary table 3). One staining (#21) was uneven and faint and was thus, assessed as being only acceptable quality. In general, the intensity of IR structures, both plaques and CAA, was quite even and strong within a single TMA section in the stainings with good quality. It is noteworthy that there was some variability in the pretreatment strategies even though all laboratories did apply formic acid pretreatment (Supplementary table 3). A faint background staining (i.e. including both grey and white matter) was detected in most of core samples in five of the 21 stainings (#4, 6, 7, 11 and 13). However, the contrast between the background staining and labelling of lesions was good. It is worth mentioning that intracellular labelling was detected in all stainings.
Aβ-IR plaques; dichotomized assessment. In two of the 35 core samples in TMA2 (cores 21, 22), only severe CAA without IR plaques was noted. Diffuse plaques were observed within most of the remaining 33 cores (30/33) by all evaluators (Table 2). Cored plaques, in turn, were detected by all evaluators in only 33% of the cores (11/33), and by 75–99% of the evaluators in 48% (16/33) of the cores.
Aβ-IR plaques: counts (independent of plaque type). At the TMA section level, the counts (0 to >20) of plaques did not differ significantly (K–W test, P = 0.999) between the BNE participants, with the mean values (±SE) ranging from 19.6 ± 0.8 to 18.1 ± 1.2 (Supplementary table 4). In 74% of the core samples (26/35), all evaluators had given a similar count of plaques (Table 2).
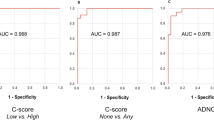
Aβ-IR plaques: density (independent of plaque type). At the TMA section level, the semiquantitative assessments of the density (from none to many) of plaques differed significantly (K–W test, P = 0.000) between the BNE participants, with the mean values (±SE) ranging from 2.1 ± 0.1 to 1.6 ± 0.1 (Fig. 7, Supplementary table 4). Absolute agreement in assessing the density of plaques between primary and re-assessment in the 19 obtained TMA2 sections ranged between 43 and 83% (Supplementary table 4). At the core sample level, by comparing assessments of the density of plaques in only 6% of cores (2/35) did all evaluators reach similar results, i.e. no plaques were seen. In contrast, when any plaques were seen (0, 1 = some ∼ 10, 2 = moderate ∼ 40, 3 = many ∼ 100), the agreement ranged between 52 and 95% (Table 2).
Aβ-IR CAA; dichotomized assessment. All evaluators had observed CAA in 34% of the core samples (12/35), whereas in four cores (11%), CAA was never detected. In 26% (5/19) of the remaining 19 core samples, 75–99% of the evaluators had seen CAA.
Aβ-IR CAA: counts and Vonsattel grade. At the TMA section level, the counts (0 to >20) of vessels exhibiting CAA did not differ significantly (K–W test, P = 0.792) between the BNE participants with the mean values (±SE) ranging from 8.2 ± 1.4 to 4.9 ± 1.1 (Supplementary table 4). At the core level, by comparing the assessments of counts of vessels exhibiting CAA, in only 14% of the cores (5/35), all assessors reached similar results. In the remaining core samples, the agreement ranged between 43 and 95% (Table 2). Moreover, in nine core samples, the evaluators had given up to three and occasionally even four possible scores, i.e. none, some, moderate, and numerous vessels exhibiting CAA. At the TMA section level, the assessments of the Vonsattel grade of CAA did not differ significantly (K–W test, P = 0.544) between the BNE participants with the mean values (±SE) ranging from 1.3 ± 0.2 to 0.7 ± 0.1 (Supplementary table 4). However, at the core level, in only 11% of the cores (4/35), had the evaluators given the same grade of Vonsattel, and in the remaining cores, the agreement ranged between 33 and 95% (Table 2). It is noteworthy that in as many as 17 of the 35 core samples, the evaluators had awarded up to three possible score values for the Vonsattel grade.
Aβ-IR arteries: veins and capillaries. CAA was never detected in the arteries in 20% (7/35), in the veins in 26% (9/35), and in the capillaries in 20% (7/35) of the core samples. More than 75% of the evaluators had observed CAA in the arteries, veins or capillaries in 39% (11/28), 23% (6/26) and in 14% (4/28) of the core samples, respectively.
Cellular Aβ-IR. All evaluators had detected Aβ-IR cells in 26% of the core samples (9/35) and moreover, in most of the remaining 26 cores, 75–99% of the evaluators had seen IR cells. The evaluators disagreed largely regarding the presence of IR cells in only two core samples with some background staining (cores 21 and 22). It is noteworthy that these two cores exhibited only CAA.
Discussion
Aβ is commonly assessed by neuropathologists in diagnostics and thus a high level of reproducibility of such an assessments is desirable. In a recent publication, BNE reported that while assessing α-synuclein pathology, only the assessment of presence or absence (dichotomized assessment) of pathology is reliable [4]. Likewise, here, when we assessed Aβ aggregates, a good agreement when using dichotomized assessment was observed when 24 neuropathologists applied their own choice of antibody (the first trial) and when 21 neuropathologists applied only one recommended antibody (the second trial).
In contrast, a poor agreement was obtained on variables, which require a quantitative and qualitative decision by the observer despite detailed instructions and even when using the same antibody. This goes beyond the present knowledge about the reliability of the assessment of the extent/load of Aβ aggregates.
The lack of agreement on the quantitative assessment of Aβ-deposits in the first trial was mainly attributed to the quality of staining rather than the choice of antibody. Thus, when only stainings of good quality were included, no significant difference was found in the counts of lesions (0 → 20) even when using three commercial antibodies. Comparably, in the second trial, when 21 participants applied only one antibody, the count of lesions did not differ significantly. It is noteworthy that the scores of lesions in individual cores in a TMA section tended to cluster at numerous lesions rather than being evenly distributed across the potential range, and thus, the lack of significant difference while counting should be interpreted with caution. In contrast, the score of counts of vessels exhibiting CAA was more evenly distributed, and thus, at least in a limited area (3.14 mm2) the counting of vessels exhibiting CAA is more reliable.
No agreement was reached in the first or the second parts of this study while assessing the density of plaques (0, 1 = some ∼ 10, 2 = moderate ∼ 40, 3 = many ∼ 100). This result might be attributed to the uneven distribution of plaques and/or presence of confluent plaques in a 2-mm core sample measuring 3.14 mm2. However, when re-assessing all core samples, it was noted that primary assessors quite often had given various assessments referring to some, moderate or many plaques, indicating that differentiation between densities as was illustrated by a cartoon in Fig. 2 was not feasible. This is unfortunate as the assessment of density of lesions is commonly applied both in diagnostics as well as in research. Thus, researchers and neuropathologists should be aware of these methodological pitfalls when comparing results obtained in different, although very trustable, laboratories. In conclusion, a direct comparison of densities of Aβ aggregates reported by different centres is not recommendable.
It is noteworthy that in this study, the results regarding counts and density were obtained when evaluating 2-mm core samples, and thus, these results are not directly applicable to routine practice where the assessment of plaques is carried out on sections including a large area of grey matter. It is intuitive that the variability should be higher when a larger specimen is observed due to the inter-rated divergence of the area considered, as the distribution of plaques is patchy. Thus, based on our results, it is questionable whether independent neuropathologists can reach comparable quantitative results without the help of morphometry.
Surprisingly, there was a poor agreement in the assignment of the type of plaques. The identification of the type of plaques, diffuse versus cored/dense seemed to be influenced not only by the antibody used but also by the observer. The influence of antibody is not surprising since each antibody is produced against different antigens (epitopes) (Fig. 3) [14, 15, 25, 26, 28]. There was, however, a high level of inter-rater variability even when one antibody was used; stainings were assessed as being good in quality even though detailed instructions including photographs were available. This is unfortunate as the type of plaques diffuse versus cored/dense is considered reflecting issues related to the development of these lesions and thus ageing and/or progression of a disease [28]. An important issue regarding concordance in assignment of lesions is probably, however, a joint training session as was recently shown by us while assigning α-synuclein IR lesions [4]. Thus, the assignment of plaque type should not be used as a diagnostic tool at least in an inter-laboratory setting.
In both parts of this trial, the assessment of the presence of CAA yielded comparable results. The distinctive features of arteries, veins and capillaries were not reliably identified in IHC-stained sections, resulting in somewhat poor agreement, particularly when assessing capillary CAA. Likewise, the assessment of the Vonsattel grade was unreliable. Thus, it is recommended that additional histological stainings should be applied when the distinction of the vessel type is required, whereas to achieve a high agreement while assigning Vonsattel grade, a joint training session is probably additionally required.
All assessors detected intracellular Aβ-IR with the clone 4G8 (second part of the trial), whereas with the clone 6F3D (first part of the trial) the results were more diverse. The variable intracellular labelling seems to be due to the different Aβ antibodies, i.e. different amino acid residues are detected. Thus, one should always keep in mind the variable performance of different commercial Aβ antibodies, particularly when comparing published reports with differing results (present vs. not present) regarding intracellular labelling.
The quality of staining varied to some extent within a TMA section. This variability is probably attributed to the pre-sectioning conditions such as post-mortem delay and fixation. Contrary to animal studies, when working with human material these issues are not easily controllable and this should be acknowledged. The TMA block was constructed from the material obtained from various centres and thus there were many pre-sectioning variables. It is noteworthy, however, that even after 5 years’ fixation, Aβ-IR deposits were detected with all antibodies used. Whether pre-sectioning conditions modify the recognition of various amino acid residues needs to be further investigated.
In conclusion, the IHC technique when visualizing Aβ may be capricious; however, all the pitfalls are manageable and avoidable when appreciated. The selection of an antibody should be based on the labelling pattern of the antibody, i.e. predominantly plaques, CAA or cytoplasm and the pretreatment technique should be optimized. It is noteworthy that compared to the Aβ in the neuropil or CAA, the intracellular Aβ labelling is significantly influenced by both the antibody and the pretreatment used. On the basis of our results, a good agreement can be achieved regarding the assessment of the presence of Aβ-IR. It should be kept in mind that assignment of variables, which require a qualitative decision by the observer such as diffuse versus cored/dense plaques, type of vessel and/or Vonsattel grade are not consistent. Furthermore, the quantitative assessment of lesions is far from reliable. Counts of lesions can be expected to be agreeably assessed within a limited area (3.14 mm2), independent of antibody used. It is intuitive, however, that when a large specimen is observed, this agreement might be lost due to the inter-rated divergence of the area considered. The agreement when assessing density, a commonly used approach, even in a limited area and in stained sections of good quality was unreliable. Thus, to reach reproducible results, a dichotomized assessment of Aβ-IR should be applied. Whereas when diagnostic neuropathologist tends to assess extent of pathology, regional involvement rather than quantification of Aβ is recommended.
References
Akiyama H, Mori H, Saido T, Kondo H, Ikeda K, McGeer PL (1999) Occurrence of the diffuse amyloid beta-protein (Abeta) deposits with numerous Abeta-containing glial cells in the cerebral cortex of patients with Alzheimer’s disease. Glia 15:324–331
Alafuzoff I, Helisalmi S, Mannermaa A, Riekkinen P Sr, Soininen H (1999) Beta-amyloid load is not influenced by the severity of cardiovascular disease in aged and demented patients. Stroke 30:613–618
Alafuzoff I, Pikkarainen M, Al-Sarraj S, Arzberger T, Bell J, Bodi I, Bogdanovic N, Budka H, Bugiani O, Ferrer I, Gelpi E, Giaccone G, Graeber MB, Hauw JJ, Kamphorst W, King A, Kopp N, Korkolopoulou P, Kovacs GG, Meyronet D, Parchi P, Patsouris E, Preusser M, Ravid R, Roggendorf W, Seilhean D, Streichenberger N, Thal DR, Kretzschmar H (2006) Interlaboratory comparison of assessments of Alzheimer disease-related lesions: a study of the BrainNet Europe Consortium. J Neuropathol Exp Neurol 65:740–757
Alafuzoff I, Parkkinen L, Al-Sarraj S, Arzberger T, Bell J, Bodi I, Bogdanovic I, Budka H, Ferrer I, Gelpi E, Gentleman S, Giaccone G, Kamphorst W, King A, Korkolopoulou P, Kovacs GG, Larionov S, Meyronet D, Monoranu C, Morris J, Parchi P, Patsouris E, Roggendorf W, Seilhean D, Streichenberger N, Thal DR, Kretzschmar H (2008) Assessment of immunohistochemically detectable α-synuclein pathology. J Neuropathol Exp Neurol 67:125–143
Allsop D, Christie G, Gray C, Holmes S, Markwell R, Owen D, Smith L, Wadsworth H, Ward RV, Hartmann T, Lichtenthaler SF, Evin G, Fuller S, Masters CL, Beyreuther K, Roberts GW (1997) Studies on inhibition of β-amyloid formation in APP751-transfected IMR-32 cells and SPA4CT-transfected SHSY5Y cells. In: Iqbal K, Winblad B, Nishimura T, Takeda M, Wisniewski HM (eds) Alzheimer’s disease: biology, diagnostics and therapeutics. Wiley, New York, pp 717–727
Arriagada PV, Marzloff K, Hyman BT (1992) Distribution of Alzheimer-type pathologic changes in nondemented elderly individuals matches the pattern in Alzheimer’s disease. Neurology 42:1681–1688
Bennhold H (1922) Eine specifische Amyloidfärbung mit Kongorot. Münch Med Wochenschr 44:1537–1538
Burns J, Pennock CA, Stoward PJ (1967) The specificity of the staining of amyloid deposits with Thioflavine T. J Pathol Bacteriol 94:337–344
Croisier E, MRes DE, Deprez M, Goldring K, Dexter DT, Pearce RK, Graeber MB, Roncaroli F (2006) Comparative study of commercially available anti-alpha-synuclein antibodies. Neuropathol Appl Neurobiol 32:351–356
Glenner GG, Wong CW (1984) Alzheimer’s disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun 16:885–890
Gouras GK, Almeida CG, Takahashi RH (2005) Intraneuronal Abeta accumulation and origin of plaques in Alzheimer’s disease. Neurobiol Aging 26:1235–1244
Hardy J, Selkoe DJ (2002) The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 19:353–356
Hucker GJ (1921) A new modification and application of the Gram stain. J Bacteriol 6:395–397
Iwatsubo T, Odaka A, Suzuki N, Mizusawa H, Nukina N, Ihara Y (1994) Visualization of Abeta 42(43) and Abeta 40 in senile plaques with end-specific Abeta monoclonals: evidence that an initially deposited species is Abeta 42(43). Neuron 13:45–53
Iwatsubo T, Saido TC, Mann DM, Lee VM, Trojanowski JQ (1996) Full-length amyloid-beta (1–42(43)) and amino-terminally modified and truncated amyloid-beta 42(43) deposit in diffuse plaques. Am J Pathol 149:1823–1830
Kallioniemi OP, Wagner U, Kononen J, Sauter G (2001) Tissue microarray technology for high-throughput molecular profiling of cancer. Hum Mol Genet 10:657–662
Kauppinen T, Martikainen P, Alafuzoff I (2006) Human postmortem brain tissue and 2-mm tissue microarrays. Appl Immunohistochem Mol Morphol 14:353–359
Kayed R, Head E, Thompson JL, McIntire TM, Milton SC, Cotman CW, Glabe CG (2003) Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis. Science 18:486–489
Kim KS, Wen GY, Bancher C, Chen CMJ, Sapienza VJ, Hong H, Wisniewski HM (1990) Detection and quantitation of amyloid B-peptide with 2 monoclonal antibodies. Neurosci Res Commun 7:113–122
Kononen J, Bubendorf L, Kallioniemi A, Bärlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP (1998) Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med 4:844–847
LaFerla FM, Green KN, Oddo S (2007) Intracellular amyloid-beta in Alzheimer’s disease. Nat Rev Neurosci 8:499–509
Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K (1985) Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natl Acad Sci USA 82:4245–4249
Matsunaga Y, Saito N, Fujii A, Yokotani J, Takakura T, Nishimura T, Esaki H, Yamada T (2002) A pH-dependent conformational transition of Abeta peptide and physicochemical properties of the conformers in the glial cell. Biochem J 1:547–556
Olichney JM, Hansen LA, Hofstetter CR, Lee JH, Katzman R, Thal LJ (2000) Association between severe cerebral amyloid angiopathy and cerebrovascular lesions in Alzheimer disease is not a spurious one attributable to apolipoprotein E4. Arch Neurol 57:869–874
Saido TC, Iwatsubo T, Mann DM, Shimada H, Ihara Y, Kawashima S (1995) Dominant and differential deposition of distinct beta-amyloid peptide species: Abeta N3(pE), in senile plaques. Neuron 14:457–466
Saido TC, Yamao-Harigaya W, Iwatsubo T, Kawashima S (1996) Amino- and carboxyl-terminal heterogeneity of beta-amyloid peptides deposited in human brain. Neurosci Lett 13:173–176
Thal DR, Ghebremedhin E, Orantes M, Wiestler OD (2003) Vascular pathology in Alzheimer disease: correlation of cerebral amyloid angiopathy and arteriosclerosis/lipohyalinosis with cognitive decline. J Neuropathol Exp Neurol 62:1287–1301
Thal DR, Capetillo-Zarate E, Del Tredici K, Braak H (2006) The development of amyloid beta protein deposits in the aged brain. Sci Aging Knowl Environ (6):re1
Wang R, Sweeney D, Gandy SE, Sisodia SS (1996) The profile of soluble amyloid beta protein in cultured cell media: detection and quantification of amyloid beta protein and variants by immunoprecipitation–mass spectrometry. J Biol Chem 13:31894–31902
Wang H, Wang H, Zhang W, Fuller GN (2002) Tissue microarrays: applications in neuropathology research, diagnosis, and education. Brain Pathol 12:95–107
Wegiel J, Kuchna I, Nowicki K, Frackowiak J, Mazur-Kolecka B, Imaki H, Wegiel J, Mehta PD, Silverman WP, Reisberg B, Deleon M, Wisniewski T, Pirttilla T, Frey H, Lehtimäki T, Kivimäki T, Visser FE, Kamphorst W, Potempska A, Bolton D, Currie JR, Miller DL (2007) Intraneuronal Abeta immunoreactivity is not a predictor of brain amyloidosis-beta or neurofibrillary degeneration. Acta Neuropathol 113:389–402
Vonsattel JP, Myers RH, Hedley-Whyte ET, Ropper AH, Bird ED, Richardson EP Jr (1991) Cerebral amyloid angiopathy without and with cerebral hemorrhages: a comparative histological study. Ann Neurol 30:637–649
Acknowledgments
We thank Tarja Kauppinen and all other laboratory technicians of the BNE members for their skilful technical assistance, Ewen MacDonald for critical reading of the manuscript, and Vesa Kiviniemi for his assistance in statistics. We acknowledge the following BNE centres (in alphabetical order of the cities) for contributing the material with generic data used in this study: Netherlands Brain Bank (Amsterdam), National and Capodistrian University of Athens (Athens), Hospital de Bellvitge/Universitat de Barcelona (Barcelona), Alma Mater Studiorum—Università de Bologna (Bologna), National Institute of Psychiatry and Neurology (Budapest, OPNI), The University of Edinburgh (Edinburgh), The Saarland University Hospital (Homburg), University of Kuopio (Kuopio), Imperial College of Science, Technology and Medicine (London), London Institute of Psychiatry (London), Hospices Civils de Lyon (Lyon), Istituto Nazionale Neurologico Carlo Besta (Milan), Ludwig-Maximilians-University of Munich (Munich), Medical University Vienna (Vienna) and University of Wuerzburg (Wuerzburg). This study was supported by European Union grant FP6: BNEII No LSHM-CT-2004-503039. This article reflects only authors’ views and the Community is not liable for any use that may be made of the information contained therein. The study has been authorized by the Ethics Committee of Kuopio University Hospital.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alafuzoff, I., Pikkarainen, M., Arzberger, T. et al. Inter-laboratory comparison of neuropathological assessments of β-amyloid protein: a study of the BrainNet Europe consortium. Acta Neuropathol 115, 533–546 (2008). https://doi.org/10.1007/s00401-008-0358-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-008-0358-2