Abstract
Axonal degeneration contributes to the transient and permanent neurological deficits seen in multiple sclerosis, an inflammatory disease of the central nervous system. To study the immunological mechanisms causing axonal degeneration, we induced experimental autoimmune encephalomyelitis (EAE) in wildtype Lewis rats and Lewis rats with a slowly progressive myelin degeneration due to proteolipid protein (PLP) overexpression. EAE was triggered either by the transfer of encephalitogenic T-cells alone or by the co-transfer of T-cells with demyelinating antibodies. Inducible nitric oxide synthase (iNOS) expression in perivascular macrophages was associated with a transient functional disturbance of axons, reflected by the focal and reversible accumulation of amyloid precursor protein. Clinical disease correlated with the numbers of APP positive axon spheroids. Demyelination was associated with a further increase of iNOS expression in macrophages and with a higher degree of axonal injury. Our studies suggest that nitric oxide and its metabolites contribute to axonal pathology and possibly also to subsequent neurological dysfunction in EAE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system (CNS) which leads to large areas of demyelination [21, 29]. Although axonal degeneration is recognized as an important cause of neurological deficit [41], the exact pathogenetic mechanisms underlying axonal injury remain unknown. Early on, axonal injury has often been interpreted as a secondary consequence of primary demyelination [9]. As there is only little evidence for direct immune attack on axons [16, 27], recent studies focused on the role of free inflammatory mediators and radicals in the disease process. These studies were initiated by the findings that inducible nitric oxide synthase (iNOS), the enzyme responsible for nitric oxide (NO) production at inflammatory sites, is up-regulated by macrophages/microglia in MS [11, 26, 30] and its animal model, experimental autoimmune encephalomyelitis (EAE) [17]. NO is able to cause reversible or irreversible axonal conduction block and thus interferes with axonal function [18, 34, 37]. In addition, NO leads to the production of peroxynitrite (ONOO-), one of the most powerful and harmful oxidants, which is suspected to induce axonal damage with characteristics of acute axonopathy [36, 40]. Peroxynitrite is readily diffusible, highly reactive, and damages proteins by rapid nitrosylation of tyrosine residues [3]. Elevated levels of 3-nitrotyrosine, a “footprint” of peroxynitrite attack, have been found in MS [26] and EAE lesions [10].
We analyzed the role of iNOS in axonal pathology in different EAE models. In the first experiments, we induced EAE in Lewis rats by the transfer of MBP-specific T-cells. Clinical disease in this model is reflected by iNOS expression in macrophages and transient axonal dysfunction in the absence of demyelination. In a second set of experiments, we injected MBP-specific T-cells in proteolipid protein (PLP)-overexpressing transgenic Lewis rats (tg). These animals are characterized by low grade myelin degeneration and microglia activation [2, 7] throughout life and allowed to address the contribution of a myelin degenerative CNS environment to axonal injury. In this model, the genetic instability of myelin increased iNOS expression and axonal dysfunction in EAE. In the last set of experiments, the rats received MBP-specific T-cells and additional demyelinating α-MOG antibodies. iNOS expression, axonal damage, and clinical disease were massively augmented in the presence of antibody-mediated demyelination.
Materials and methods
Animals
All hemizygous PLP-overexpressing transgenic Lewis rats and their wildtype littermates used in this study have already been described elsewhere [1]. In addition, we used young adult Lewis rats, which were purchased from Charles River Laboratories (Sulzfeld, Germany). The animals were kept under standardized conditions. All procedures and experiments were carried out in accordance to protocols approved by the local animal welfare committee.
T-cells and antibodies
Encephalitogenic MBP-specific T-cells used in this study were established from Lewis rats according to established protocols [4]. Depending on the T-cell line used, between 1×105 and 5×106 MBP-specific T-cells were injected. The production of the α-MOG serum has already been described [1].
Induction of EAE
-
1.
For the induction of purely T-cell-mediated EAE, freshly activated MBP-specific T-cells were injected into young adult Lewis rats.
-
2.
For the induction of T-cell initiated, antibody-mediated EAE, the animals were injected with freshly activated MBP-specific T-cells on day 0, followed by the injection of 1.5 ml α-MOG serum or control serum on day 3 (prior to the onset of clinical disease).
Clinical evaluation of EAE
The rats were weighed daily and scored for neurological signs as follows: 0.5, partial loss of tail tonus; 1, complete loss of tail tonus; 2, hind limb paresis; 3, hind limb paralysis; 4, tetra-paresis/paralysis.
Antibodies
The following well-characterized antibodies were used: Monoclonal (mouse) antibodies: W3/13 (1:50; T-cells, Harlan Sera-Lab, Leicestershire, UK), ED1 (1:4,000; activated macropages/microglia, Serotec, Kidlington, Oxford, UK), α-EMAP II (1:1,000; activated macrophages/microglia, Abcam, Cambridge, UK), α-AIF (1:500; Allograft Inhibitory Factor; activated macrophages/microglia, BMA, Augst, Switzerland), α-glial fibrillary acid protein GFAP (1:300; astrocytes; Neomarkers, Fremont, CA, USA), α-2′3′-cyclic nucleotide 3′ phosphodiesterase CNP (1:2,000; oligodendrocytes, myelin; Sternberger Monoclonals Incorporated, Lutherville, MD, USA), α-amyloid precursor protein APP (1:1,000; marker for acute axonal injury; Chemicon, Temecula, CA, USA), α-non-phosphorylated neurofilament protein SMI32 (1:1,000; clone SMI32; Sternberger Monoclonals Incorporated, Lutherville, MD, USA), α-MHC II (1:250; microglia/macrophages; DAKO, Glostrup, Denmark); Polyclonal (rabbit) antibodies: α-iNOS (1:500; inducible nitric oxide synthase; Chemicon, Temecula, CA, USA), α-nitrotyrosine NT (1:500; Upstate Biotechnology, Lake Placid, NY, USA), α-GFAP (1:3,000; astrocytes, DAKO, Glostrup, Denmark), α-myelin basic protein MBP (1:2,500; myelin, DAKO, Glostrup, Denmark), α-neurofilament 68 kD (1:1,000; neurons, axons; Chemicon, Temecula, CA, USA).
Histology and immunohistochemistry
For histological analysis, the rats were killed with CO2 and transcardially perfused with 4% paraformaldehyde (PFA) in phosphate buffered saline (PBS). The brains and spinal cords were dissected, postfixed in 4% PFA/PBS for 24 h and paraffin embedded. Two to four micrometer thick adjacent serial sections were cut on a microtome and stained with hematoxylin/eosin, luxol fast blue, and Bielschowsky’s silver impregnation to assess inflammation, demyelination, and axonal pathology, respectively.
Immunohistochemistry was carried out as follows: the sections were deparaffinized in xylene for 1 h and transferred to 96% ethanol. Endogenous peroxidase was blocked by incubation in 0.03% hydrogen peroxide for 30 min. The sections were rehydrated through a descending ethanol series (96, 70, 50%) and rinsed in distilled water. The slides were heated in 10 mM citrate buffer, rinsed in 0.1 M PBS for 60 min, and then exposed to 10% fetal calf serum (FCS) in PBS for 20 min at room temperature to reduce non-specific background. Then, the slides were washed with PBS 3–4 times and incubated with primary antibodies (described above) at 4°C overnight. The sections were then washed in PBS and exposed to biotinylated secondary antibodies (1:200; donkey–anti-rabbit; donkey–anti-mouse; Amersham Pharmacia Biotech, Uppsala, Sweden) in FCS/PBS for 2 h at room temperature followed by avidin–peroxidase complex (1:100; Sigma, St Louis, MO, USA) for 1 h. Peroxidase reactivity was visualized with 3,3′-diaminobenzidine-tetra-hydrochloride (DAB; Sigma, St Louis, MO, USA) containing 0.3% hydrogen peroxide. Negative controls were performed by omitting the primary antibody or by using irrelevant isotype-matched control antibodies. All the sections were counterstained with Meyer’s hematoxylin, dehydrated, and coverslipped.
Double labeling
For the simultaneous detection of APP and iNOS, the paraffin embedded sections were pre-treated as described above, followed by incubation with a mixture of mouse α-APP (1:1,000) and rabbit α-iNOS (1:500) at 4°C overnight. After washing 3–4 times with PBS, two different detection systems were applied including (1) α-mouse alkaline phosphatase-conjugated IgG (1:150; Jackson Immuno Research Laboratories, West Grove, PA, USA) and (2) biotinylated donkey α-rabbit IgG (1:200; Amersham Pharmacia Biotech), each for 2 h followed by incubation with avidin–peroxidase complex (1:100; Sigma). The slides were incubated in fast blue salt solution at 37°C for 1–3 h to detect the alkaline phosphatase complex, and then washed several times with PBS. Avidine–peroxidase complex was visualized as described above for light microscopy.
For the fast blue salt developing solution, 25 mg fast blue salt (Sigma, St Louis, MO, USA) was dissolved in 615 μl 2 M hypochloric acid (Sigma, St Louis, MO, USA) and 615 μl NaNO2 (Merck, Darmstadt, Germany) and added to a solution containing 100 ml 0.1 M tris-hypochloric acid puffer pH 8.5 [12.1 g tris-aminomethane (Merck, Darmstadt, Germany) in 980 ml distilled water and 20 ml 2 M hypochloric acid (Merck, Darmstadt, Germany)], with 12.5 mg Naphtol-AS-MX-phosphate (Sigma, St Louis, MO, USA), 615 μl dimethyl-formamide (Sigma, St Louis, MO, USA) and 185 μl levamisole (Sigma, St Louis, MO, USA).
Double fluorescence labeling
For additional analyses, double fluorescence labeling was performed. In principle, pre-treatment of the slides and the application of primary and appropriate secondary antibodies was performed as described above with minor modifications. Briefly, after incubation with primary antibodies from different species (mouse, rabbit) at 4°C overnight, the slides were washed with PBS several times and exposed to compatible secondary antibodies consisting of either biotinylated-sheep-α-mouse or biotinylated-sheep-α-rabbit (both 1:200; Amersham Pharmacia Biotech) and either donkey-α-mouse Cy3 or goat-α-rabbit Cy3 (both 1:100; Jackson Immuno Research Laboratories, West Grove, PA, USA) for 1 h at room temperature. Double labeling was finished by application of Cy2 conjugated streptavidin (1:75; Jackson Immuno Research Laboratories, West Grove, PA, USA). Finally, the slides were mounted with PBS/glycerol (1:9) with 3% DABCO (Sigma, St Louis, MO, USA). In contrast to the immunocytochemistry protocol for light microscopy, FCS/PBS was replaced in all the steps by “antibody diluent” solution (DAKO, Glostrup, Denmark).
Laser scanning confocal microscopy
Fluorescence analysis was performed with a Zeiss LSM-410 motorized confocal laser scan microscope (Carl Zeiss, Jena, Germany) equipped with an argon-ion laser source [488 nm excitation] and two HeNe lasers [543 and 633 nm excitation]. Operating conditions (contrast, brightness settings) and an appropriate combination of excitation- and barrier filters (bandpass filters 515–525 and 595–615 nm) were used to eliminate “bleed-through” from either channel. Fluorescence signals were collected either simultaneously or sequentially in the green (Cy2) or red channel (Cy3). In some cases, z-series from three to ten planes with an axial resolution of 0.25 μm were collected for reconstruction and analyzed with LSM Image Browser © software from Zeiss. Co-localization of antigens, for example ED1 (red) and iNOS (green), appears in yellow.
Quantitative assessment
The numbers of inflammatory cells (iNOS, W3/13, ED1), APP positive axons/spheroids, and demyelinated lesion areas were analyzed in at least six representative complete adjacent spinal cord sections of each animal by blinded investigators (PW, FAE).
Statistical analysis
For the statistical analysis, non-parametric group tests and regression analysis were applied. All the tests were classified as significant if the P-value was <0.05. All values are expressed as means ± standard error of the mean.
Results
Clinical disease in acute T-cell-mediated EAE is reflected by iNOS expression in macrophages and transient axonal dysfunction in the absence of demyelination
Following the transfer of MBP-specific T-cells, EAE developed in all the Lewis rats. The disease followed a monophasic acute course with complete remission and recovery: weight loss and first neurological signs such as loss of tail tonus appeared 4 days after transfer of MBP-specific T-cells. The maximum clinical score—nearly all animals (10/11) showed paretic hind limbs—was reached on day 5 (average of all animals 1.96±0.45; Fig. 1). On day 8 after cell transfer, a complete remission of clinical symptoms was observed in all the animals.
Clinical disease in acute T-cell-mediated experimental autoimmune encephalomyelitis is reflected by inducible nitric oxide synthase (iNOS) expression in macrophages and transient axonal dysfunction in the absence of demyelination. iNOS+ macrophages (white bar) were present at the peak of inflammation on day 6 (asterisk, P<0.01). APP+ acutely injured axons (black bars) were found in highest numbers on day 6 (asterisk, P<0.01), and their numbers decreased. In the following disease course, complete remission was reflected by the complete absence of iNOS+ macrophages and rapid decline of axonal APP expression (black bars) within all lesions. A strong significant relationship was found between iNOS+ macrophages and APP+ spheroids (correlation coefficient=0.95; r 2=90.24%; P<0.00001)
The clinical course was reflected in histological observations: on day 3 infiltration of W3/13+ T-cells and ED1+ activated macrophages was exclusively confined to the meninges, with a predilection for the lumbar spinal cord. No signs for axonal injury or demyelination were found. On day 6, additional widespread inflammatory infiltration was noticed around the parenchymal veins and venules and in the parenchyma (Fig. 2a). The perivascular infiltrates consisted predominantly of W3/13+ T lymphocytes (66.7±14.4 mm−2) and ED1+ macrophages (252.9±17.4 mm−2). Whereas various microglia and macrophage activation antigens such as ED1, EMAP-II, and AIF were found up-regulated throughout the whole spinal cord parenchyma (Fig. 2a; data for EMAP-II and AIF are not shown), iNOS expression remained restricted to a small fraction of macrophages in the perivascular regions only (Fig. 2b; arrowheads).
iNOS+ (inducible nitric oxide synthase) macrophages are only a small subset of macrophages in experimentally induced central nervous system inflammation. a On day 6, extensive meningeal and perivascular infiltration of immune cells were seen in the spinal cord (a: ED1). Note that activated ED1+ macrophages were seen throughout the entire spinal cord (a: ED1), but iNOS + macrophages were restricted to some perivascular regions only (b: iNOS, arrowheads). Bars a, b—500 μm
In detail, iNOS expression was exclusively found in macrophages (31.0±1.9 mm−2), and was completely absent in the endothelial cells, lymphocytes, astrocytes, oligodendrocytes, or neurons (Fig 3a–c). In parallel, immunoreactivity for nitrotyrosine (Fig. 3d) was found around perivascular inflamed vessels, indicating in vivo generation of peroxynitrite, a powerful oxidant formed by the rapid combination of free oxygen and nitrogen intermediates [35, 43]. Furthermore, in all the spinal cord sections examined, perivascular expression of APP was detected in axons and/or axonal spheroids (32.4±2.1 mm−2; Fig. 4), indicating acute axonal injury [20]. The myelin sheaths remained intact (Fig. 3g–h). Most importantly, we found a strict correlation of iNOS reactive macrophages with acute axonal injury (Fig. 1, regression analysis: correlation coefficient 0.97, r 2=94.8%, P<0.00001). Confocal analysis, too, revealed a close proximity of iNOS positive macrophages to injured axons (Fig. 3b, arrow). Axonal and/or spheroidal APP expression was completely absent in perivascular cuffs consisting of W3/13+ T-cells and ED1+/iNOS- macrophages only. On day 9–15, the numbers of all inflammatory cells declined (perivascular T-cells—day 9, 10.9±1.6 mm−2 to day 15, 3.0±3.1 mm−2; perivascular macrophages—day 9, 175.1±9.6 mm−2 to day 15, 11.5±1.7 mm−2). iNOS expression could no longer be detected and the numbers of APP positive axonal spheroids decreased progressively (Fig. 1). At this point of time, we did not observe any signs for axonal transection (axonal end bulbs), axonal loss (Bielschowsky silver-impregnation), or demyelination (data not shown).
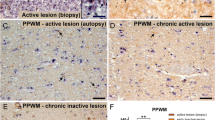
Identification of inducible nitric oxide synthase (iNOS) mediated axonal damage in experimental autoimmune encephalomyelitis (EAE). a–d Confocal lasermicroscopy scans: in all the experiments iNOS expression was strictly confined to ED1 + macrophages (a: iNOS, green; ED1, red; colocalization appears in yellow) in close proximity (b: arrows) to acutely injured APP + axons (b: iNOS, green; APP, red; asterisk lumen of inflamed vessel). Immunoreactivity for iNOS was completely absent in other cell types. Here, we show the lack of any reactivity for iNOS (green) in astrocytes (c: arrows) close to an inflamed vessel (asterisk vessel lumen) consisting of numerous iNOS + macrophages (c: iNOS, green; GFAP, red). Note that the immunoreactivity for nitrotyrosine was found in areas of axonal injury (d: APP, green; NT, red; asterisk lumen of inflamed vessel). e–l MBP-specific T-cell-mediated EAE in proteolipid protein-overexpressing transgenic Lewis rats in the absence (e–h), or presence of α-MOG antibodies (i–l). e–g Stainings of consecutive tissue sections with ED1 (e) and APP blue and iNOS brown (f: double labeling; no counterstain with hematoxylin) and CNP (g) reveal that acute axonal injury is strictly associated with ED1 +/iNOS + macrophages. Myelin sheaths remained intact (g: CNP; h: confocal analysis—APP, green; MBP, red). In the presence of α-MOG antibodies, sparse subpial and perivascular demyelination (arrows; i: luxol fast blue) and C9 complement deposition (j: red) was seen. In consecutive sections, ED1 + macrophages (k) and iNOS + macrophages (brown) associated with APP+ spheroids (blue) were seen (l: double labeling; no counterstain with hematoxylin). Bars—a, b 30 μm; c 25 μm; d 50 μm; e–g 100 μm; h 10 μm; i–l 150 μm
Correlation between the numbers of iNOS+ (inducible nitric oxide synthase) macrophages and acutely injured APP+ axons/spheroids within the lesions of different experimental autoimmune encephalomyelitis models on day 6. Strong correlation between iNOS+ macrophages and acutely injured APP+ axons (correlation coefficient=0.75; r 2=55.6%; P<0.0002). Black circles wt/normal serum (NS); white circles wt/α-MOG; black triangles proteolipid protein-overexpressing transgenic Lewis rats (tg)/NS; white triangles tg/α-MOG
To summarize, this experiment revealed a temporal and spatial correlation of acute axonal injury with iNOS expressing macrophages/microglia in the absence of demyelination. The axonal pathology was transient.
Genetic instability of myelin increases iNOS expression and axonal dysfunction in EAE
In the next experiments, we used PLP-overexpressing transgenic Lewis rats as recipients for MBP-specific T-cells. These animals allow study of the consequences of inflammation for axonal pathology in a degenerative CNS environment, characterized by myelin/oligodendrocyte dystrophy. This is defined by PLP accumulation within oligodendrocytes, resulting in an endoplasmatic reticulum stress reaction, some scattered apoptotic cell death, minor demyelination, and chronic microglia activation [7].
Comparable to our former experiments, PLP-overexpressing transgenic Lewis rats (tg) showed first clinical symptoms on day 4 after T-cell transfer. CNS disease and EAE course showed a minor increase in transgenic animals that received T-cells and normal serum (NS) compared to their wildtype counterparts (clinical score for tg/NS 2.4±1.3; wt/NS 1.8±0.5), which, however, did not reach statistical significance.
On day 6, histological analyses revealed widespread meningeal, perivascular, and parenchymal infiltration of W3/13+ T-cells and ED1+ macrophages throughout the spinal cord, with a predilection of lumbar spinal cord and gray/white matter junctions. The overall numbers of lymphocytic infiltrates of both the groups were comparable [1], while the numbers of ED1+/iNOS+ macrophages increased in the degenerative CNS (Fig. 4). iNOS expression was strictly confined to cells of the macrophages/microglia cell lineage (Fig. 3a). These cells were predominately located around inflamed vessels, and were clearly associated with immunoreactivity for nitrotyrosine and profound acute axonal injury (Fig. 3b, d–f). Most dystrophic axons were surrounded by myelin sheaths (Fig. 3g–h). In sum, this experiment showed an enhanced susceptibility of the degenerative CNS to axonal damage provoked by iNOS+ macrophages.
iNOS expression, axonal dysfunction, and clinical deficit are augmented in EAE in the presence of antibody-mediated demyelination
To study the effect of demyelination on axonal injury and iNOS expression in EAE, we additionally administered demyelinating antibodies in the wildtype and degenerative CNS.
The onset of the disease was comparable to our former experiments on day 4. MBP specific T-cell transfer with additional administration of α-MOG antibodies led to a slight aggravation of clinical symptoms (wt/α-MOG 2.3±0.5), but provoked a very aggressive disease course in tg/α-MOG animals (clinical score 3.75±0.25; P<0.01).
The degree of demyelination was low (Fig. 3i; [1]), but abundant meningeal, perivascular, and parenchymal infiltration of W3/13+ T lymphocytes and ED1+ macrophages were found in all the spinal cord sections examined. While the numbers of W3/13+ T-cells were comparable in both groups of animals, numbers of ED1+/iNOS+ macrophages were significantly increased in tg/α-MOG animals (Fig. 4). As seen in our former experiments, immunoreactivity for iNOS was exclusively found in macrophages and/or microglia cells. Perivascular ED1+/iNOS+ macrophages were clearly associated with APP+ axons/spheroids (Figs. 3k–l, 4).
Taken together, the presence of demyelinating α-MOG antibodies led to enhanced numbers of iNOS+ cells in the wildtype, and even more so in the degenerative CNS parenchyma (Fig. 4).
Correlation between axonal pathology and clinical disease
In the next step, we combined all the experimental groups receiving T-cells together with NS or demyelinating α-MOG antibodies, and plotted the numbers of APP+ axons/spheroids (Fig. 5) or the numbers of iNOS+ macrophages (Fig. 6) against the EAE score. Clear correlations between clinical disease and axonal injury (Fig. 5), and between clinical disease and the numbers of iNOS+ macrophages (Fig. 6) were found.
Clinical disease was reflected by the presence of APP+ acutely injured axons within the lesions in different experimental autoimmune encephalomyelitis models on day 6 (correlation coefficient=0.64; r 2=40.7%; P<0.002). Black circles wt/normal serum (NS); white circles wt/α-MOG; black triangles tg/NS; white triangles tg/α-MOG
Clinical disease was reflected by the presence and numbers of iNOS+ (inducible nitric oxide synthase) macrophages within the lesions of different experimental autoimmune encephalomyelitis models on day 6 (correlation coefficient=0.76; r 2=58.2%; P<0.00001). Line regression curve; dashed lines 95% confidence intervals; dotted lines prediction intervals; black circles wildtype Lewis rats (wt) that received MBP-specific T-cells only; white circles wt/normal serum (NS); black triangles ωτ/α-MOG; white triangles tg/NS; black squares tg/α-MOG
Discussion
Recent reports identified axonal degeneration as an important substrate of neurological deficit in MS [41]. Axonal degeneration is commonly regarded as a secondary consequence of demyelination. However, our study shows that axonal injury may occur in brain inflammation in absence of demyelination. The key observations of our study are as follows:
-
1.
In purely T-cell-mediated EAE, the peak of clinical disease was synchronous with iNOS expression in macrophages and nitrotyrosine deposition in the absence of demyelination. This was associated with axonal dysfunction, reflected by transient disturbance of axonal transport.
-
2.
When demyelination was additionally present in EAE, clinical disease was augmented and associated with a significant increase in iNOS expression in macrophages and with an increase in axonal injury.
-
3.
Acute axonal damage and macrophages positive for iNOS were found in essentially the same areas within the spinal cord lesions. In the remaining spinal cord areas, where no acute axonal damage was found, macrophages and/or microglia did not express iNOS.
In chronic models of EAE in both the rat and mouse, extensive myelin loss is evident, in particular in the animals’ spinal cord [21–23]. Consequently, the neurological symptoms and the clinical disease seen in these EAE models are generally explained by demyelination, followed eventually by degeneration and loss of axons. Recovery in chronic EAE models correlates with remyelination [6, 28] and restoration of axonal function [19].
In acute EAE, functional neurological deficit and clinical disease cannot be explained easily by demyelination. In these animals, extremely severe clinical deficit may be present in the absence of visible demyelination in the CNS. Although it has been argued that demyelination in the peripheral nerve roots may account for clinical deficit in acute EAE [8, 31, 32], this is not the case in animals sensitized with MOG [25]. In addition, extensive demyelination can be seen in the root entry and exit zones in the absence of clinical disease, following intrathecal injection of anti-MOG antibodies [42].
Our study offers an additive explanation for clinical disease in acute EAE, the direct induction of acute (and reversible) axonal injury by macrophage toxins, such as NO radicals. Recent studies suggest that various soluble factors such as free radicals or NO [5, 39, 40] produced by inflammatory cells may cause reversible axonal dysfunction or even permanent axonal degeneration.
In our acute monophasic rat EAE model, we found a strict temporal and spatial correlation of acute axonal injury to ED1+/iNOS+ macrophages and to immunoreactivity for nitrotyrosine, a footprint for in vivo peroxynitrite formation. Interestingly, the widespread expression of other macrophage activation antigens such as ED1, EMAP-II and AIF was not associated with axonal injury. This suggests that iNOS-induced NO production may play a central role in the induction of axonal injury. There are several possibilities to explain the role of NO for axonal dysfunction/degeneration: NO was shown to inhibit mitochondrial respiration and may thus cause axonal energy failure [44]. It may also lead to an increase of intra-axonal sodium levels, which may be followed by an increased calcium influx into the axons. This may directly interfere with axonal transport or may activate proteases, which dissolve the axonal cytoskeleton and hence block axonal transport [38, 39].
Following the induction of EAE in PLP-overexpressing transgenic Lewis rats, we found increased numbers of (iNOS+) macrophages and increased axonal pathology in the CNS of these animals. One explanation for this could be that the altered gene dosage of PLP in the transgenic animals might have increased the susceptibility of the axons for later degeneration in the absence of inflammation or demyelination, as seen in patients and in mice lacking PLP [14, 15]. However, such an explanation does not fit our observations in the PLP-overexpressing transgenic rats: first, PLP overexpression in these rats leads to myelin degeneration and microglia activation [2, 7], but not to spontaneous axonal degeneration. And secondly, inflammation in the CNS of these animals causes an enhanced axonal degeneration, which is strongly associated with increased numbers of iNOS+ macrophages. These cells are either recruited from the activated microglia cells present in the transgenic CNS [1] or from the peripheral macrophage pool in response to chemoattractants produced by the activated glial cells [13]. Hence, in transgenic animals, the pre-activation of microglia and/or better recruitment of macrophages leads to higher numbers of cells expressing iNOS, higher levels of NO, and more axonal damage. Following the co-transfer of α-MOG antibodies and T-cells, axonal degeneration was further enhanced. In this setting, the binding of the antibodies to the myelin sheaths and the activation of complement at this site might further activate macrophages by complement or Fc-receptor-mediated mechanisms [24, 33], possibly resulting in higher numbers of iNOS+ macrophages in the perivascular cuffs. It was recently described that even low grade demyelination, with only subtle release of myelin breakdown products, leads to a self-amplification loop of macrophage phagocytosis and activation [12]. This could lead to enhanced iNOS expression, to higher tissue concentrations of NO and peroxynitrite, and hence to augmented acute axonal injury. Moreover, lack of myelin sheaths might render axons more susceptible to free-radical-mediated damage [34].
In conclusion, our data established a possible key role for iNOS in various models of experimentally transferred CNS inflammation. This view is supported by the strict temporal and spatial correlation of iNOS+ macrophages and APP+ acutely injured axons. The highly significant association between iNOS and nitrotyrosine expression with clinical disease in experimentally transferred CNS inflammation suggests that a functional disturbance of axonal conduction, as seen following the exposure of axons with NO in vitro [34], may also be relevant in vivo. Unfortunately, there are no treatment strategies available that efficiently target the expression of iNOS in the CNS.
Our data further suggest that in an inflammatory condition like that in MS, demyelination is not a prerequisite for axonal injury. Such a mechanism may be important in the pathogenesis of diffuse damage of the normal appearing white matter in MS patients.
Abbreviations
- MOG:
-
Myelin oligodendrocyte glycoprotein
- α-MOG:
-
Anti-MOG antibodies
- APP:
-
Amyloid precursor protein
- CNP:
-
2′3′-cyclic nucleotide 3′ phosphodiesterase
- EAE:
-
Experimental autoimmune encephalomyelitis
- GFAP:
-
Glial fibrillary acidic protein
- MBP:
-
Myelin basic protein
- NS:
-
Normal serum
- NT:
-
Nitrotyrosine
- PFA:
-
Paraformaldehyde
- PLP:
-
Proteolipid protein
- Tg:
-
Transgenics
References
Aboul-Enein F, Bauer J, Klein M, Schubart A, Flugel A, Ritter T, Kawakami N, Siedler F, Linington C, Wekerle H, Lassmann H, Bradl M (2004) Selective and antigen-dependent effects of myelin degeneration on central nervous system inflammation. J Neuropathol Exp Neurol 63:1284–1296
Bauer J, Bradl M, Klein M, Leisser M, Deckwerth TL, Wekerle H, Lassmann H (2002) Endoplasmic reticulum stress in PLP-overexpressing transgenic rats: gray matter oligodendrocytes are more vulnerable than white matter oligodendrocytes. J Neuropathol Exp Neurol 61:12–22
Beckman JS (2002) Protein tyrosine nitration and peroxynitrite. FASEB J 16:1144
Ben Nun A, Wekerle H, Cohen IR (1981) The rapid isolation of clonable antigen-specific T lymphocyte lines capable of mediating autoimmune encephalomyelitis. Eur J Immunol 11:195–199
Bitsch A, Schuchardt J, Bunkowski S, Kuhlmann T, Bruck W (2000) Acute axonal injury in multiple sclerosis. Correlation with demyelination and inflammation. Brain 123:1174–1183
Blight AR (1993) Remyelination, revascularization, and recovery of function in experimental spinal cord injury. Adv Neurol 59:91–104
Bradl M, Bauer J, Inomata T, Zielasek J, Nave KA, Toyka K, Lassmann H, Wekerle H (1999) Transgenic Lewis rats overexpressing the proteolipid protein gene: myelin degeneration and its effect on T cell-mediated experimental autoimmune encephalomyelitis. Acta Neuropathol 97:595–606
Chalk JB, McCombe PA, Pender MP (1994) Conduction abnormalities are restricted to the central nervous system in experimental autoimmune encephalomyelitis induced by inoculation with proteolipid protein but not with myelin basic protein. Brain 117:975–986
Charcot JM (1868) Histologie de la sclerose en plaque. Gaz Hosp (Paris) 41:554–556
Cross AH, Manning PT, Stern MK, Misko TP (1997) Evidence for the production of peroxynitrite in inflammatory CNS demyelination. J Neuroimmunol 80:121–130
De Groot CJ, Ruuls SR, Theeuwes JW, Dijkstra CD, Van der Valk P (1997) Immunocytochemical characterization of the expression of inducible and constitutive isoforms of nitric oxide synthase in demyelinating multiple sclerosis lesions. J Neuropathol Exp Neurol 56:10–20
Diestel A, Aktas O, Hackel D, Hake I, Meier S, Raine CS, Nitsch R, Zipp F, Ullrich O (2003) Activation of microglial poly(ADP-ribose)-polymerase-1 by cholesterol breakdown products during neuroinflammation: a link between demyelination and neuronal damage. J Exp Med 198:1729–1740
Fuentes ME, Durham SK, Swerdel MR, Lewin AC, Barton DS, Megill JR, Bravo R, Lira SA (1995) Controlled recruitment of monocytes and macrophages to specific organs through transgenic expression of monocyte chemoattractant protein-1. J Immunol 155:5769–5776
Garbern JY, Yool DA, Moore GJ, Wilds IB, Faulk MW, Klugmann M, Nave KA, Sistermans EA, van der Knaap MS, Bird TD, Shy ME, Kamholz JA, Griffiths IR (2002) Patients lacking the major CNS myelin protein, proteolipid protein 1, develop length-dependent axonal degeneration in the absence of demyelination and inflammation. Brain 125:551–561
Griffiths I, Klugmann M, Anderson T, Yool D, Thomson C, Schwab MH, Schneider A, Zimmermann F, McCulloch M, Nadon N, Nave KA (1998) Axonal swellings and degeneration in mice lacking the major proteolipid of myelin. Science 280:1610–1613
Hoftberger R, Aboul-Enein F, Brueck W, Lucchinetti C, Rodriguez M, Schmidbauer M, Jellinger K, Lassmann H (2004) Expression of major histocompatibility complex class I molecules on the different cell types in multiple sclerosis lesions. Brain Pathol 14:43–50
Hooper DC, Bagasra O, Marini JC, Zborek A, Ohnishi ST, Kean R, Champion JM, Sarker AB, Bobroski L, Farber JL, Akaike T, Maeda H, Koprowski H (1997) Prevention of experimental allergic encephalomyelitis by targeting nitric oxide and peroxynitrite: implications for the treatment of multiple sclerosis. PNAS 94:2528–2533
Kapoor R, Davies M, Smith KJ (1999) Temporary axonal conduction block and axonal loss in inflammatory neurological disease: a potential role for nitric oxide? Ann NY Acad Sci 893:304–308
Kerschensteiner M, Bareyre FM, Buddeberg BS, Merkler D, Stadelmann C, Bruck W, Misgeld T, Schwab ME (2004) Remodeling of axonal connections contributes to recovery in an animal model of multiple sclerosis. J Exp Med 200:1027–1038
Kornek B, Storch MK, Weissert R, Wallstroem E, Stefferl A, Olsson T, Linington C, Schmidbauer M, Lassmann H (2000) Multiple sclerosis and chronic autoimmune encephalomyelitis: a comparative quantitative study of axonal injury in active, inactive, and remyelinated lesions. Am J Pathol 157:267–276
Lassmann H (1998) Pathology of multiple sclerosis. In: Compston A, Ebers G, Lassmann H, McDonald I, Matthews B, Wekerle H (eds) McAlpine’s multiple sclerosis. Churchill Livingstone, London, pp 323–377
Lassmann H, Wekerle H (1998) Experimental models of multiple sclerosis. In: Compston A, Ebers G, Lassmann H, McDonald I, Matthews B, Wekerle H (eds) McAlpine’s multiple sclerosis. Churchill Livingstone, London, pp 409–433
Lassmann H, Brunner C, Bradl M, Linington C (1988) Experimental allergic encephalomyelitis: the balance between encephalitogenic T lymphocytes and demyelinating antibodies determines size and structure of demyelinated lesions. Acta Neuropathol 75:566–576
Linington C, Lassmann H, Morgan BP, Compston DA (1989) Immunohistochemical localisation of terminal complement component C9 in experimental allergic encephalomyelitis. Acta Neuropathol 79:78–85
Linington C, Berger T, Perry L, Weerth S, Hinze-Selch D, Zhang Y, Lu HC, Lassmann H, Wekerle H (1993) T cells specific for the myelin oligodendrocyte glycoprotein mediate an unusual autoimmune inflammatory response in the central nervous system. Eur J Immunol 23:1364–1372
Liu JSH, Zhao ML, Brosnan CF, Lee SC (2001) Expression of inducible nitric oxide synthase and nitrotyrosine in multiple sclerosis lesions. Am J Pathol 158:2057–2066
Medana I, Martinic MA, Wekerle H, Neumann H (2001) Transection of major histocompatibility complex class I-induced neurites by cytotoxic T lymphocytes. Am J Pathol 159:809–815
Murray PD, McGavern DB, Sathornsumetee S, Rodriguez M (2001) Spontaneous remyelination following extensive demyelination is associated with improved neurological function in a viral model of multiple sclerosis. Brain 124:1403–1416
Noseworthy JH, Lucchinetti C, Rodriguez M, Weinshenker BG (2000) Multiple sclerosis. N Engl J Med 343:938–952
Oleszak EL, Zaczynska E, Bhattacharjee M, Butunoi C, Legido A, Katsetos CD (1998) Inducible nitric oxide synthase and nitrotyrosine are found in monocytes/macrophages and/or astrocytes in acute, but not in chronic multiple sclerosis. Clin Diagn Lab Immunol 5:438–445
Pender MP, Sears TA (1985) Vulnerability of the dorsal root ganglion in experimental allergic encephalomyelitis. Clin Exp Neurol 21:211–223
Pender MP, Sears TA (1986) Involvement of the dorsal root ganglion in acute experimental allergic encephalomyelitis in the Lewis rat. A histological and electrophysiological study. J Neurol Sci 72:231–242
Piddlesden SJ, Lassmann H, Zimprich F, Morgan BP, Linington C (1993) The demyelinating potential of antibodies to myelin oligodendrocyte glycoprotein is related to their ability to fix complement. Am J Pathol 143:555–564
Redford EJ, Kapoor R, Smith KJ (1997) Nitric oxide donors reversibly block axonal conduction: demyelinated axons are especially susceptible. Brain 120:2149–2157
Reiter CD, Teng RJ, Beckman JS (2000) Superoxide reacts with nitric oxide to nitrate tyrosine at physiological pH via peroxynitrite. J Biol Chem 275:32460–32466
Smith KJ, Kapoor R, Felts PA (1999) Demyelination: the role of reactive oxygen and nitrogen species. Brain Pathol 9:69–92
Smith KJ, Kapoor R, Hall SM, Davies M (2001) Electrically active axons degenerate when exposed to nitric oxide. Ann Neurol 49:470–476
Strong MJ, Sopper MM, Crow JP, Strong WL, Beckman JS (1998) Nitration of the low molecular weight neurofilament is equivalent in sporadic amyotrophic lateral sclerosis and control cervical spinal cord. Biochem Biophys Res Commun 248:157–164
Stys PK (1998) Anoxic and ischemic injury of myelinated axons in CNS white matter: from mechanistic concepts to therapeutics. J Cereb Blood Flow Metab 18:2–25
Touil T, Deloire-Grassin MS, Vital C, Petry KG, Brochet B (2001) In vivo damage of CNS myelin and axons induced by peroxynitrite. Neuroreport 12:3637–3644
Trapp BD, Ransohoff R, Rudick R (1999) Axonal pathology in multiple sclerosis: relationship to neurologic disability. Curr Opin Neurol 12:295–302
Vass K, Heininger K, Schafer B, Linington C, Lassmann H (1992) Interferon-gamma potentiates antibody-mediated demyelination in vivo. Ann Neurol 32:198–206
Viera L, Ye YZ, Estevez AG, Beckman JS (1999) Immunohistochemical methods to detect nitrotyrosine. Methods Enzymol 301:373–381
Waxman SG (2003) Nitric oxide and the axonal death cascade. Ann Neurol 53:150–153
Acknowledgments
This work was supported by the FWF (project P16047-B02) and the European commission (QLG3-CT-2002-00612). The authors wish to thank Ulrike Köck, Angela Kury, and Marianne Leiszer for the excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aboul-Enein, F., Weiser, P., Höftberger, R. et al. Transient Axonal Injury in the Absence of Demyelination: A Correlate of Clinical Disease in Acute Experimental Autoimmune Encephalomyelitis. Acta Neuropathol 111, 539–547 (2006). https://doi.org/10.1007/s00401-006-0047-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-006-0047-y