Abstract
HAART-induced immune restoration is beneficial for patients with AIDS-related progressive multifocal leukoencephalopathy (PML). However, in rare instances, an immune-reconstitution inflammatory syndrome (IRIS) may cause paradoxical clinical deterioration. We report the neuropathological study of an AIDS patient who presented with progressive cognitive deterioration; CD4+ count was 117 and the HIV viral load >104; imaging showed non-enhancing lesions consistent with PML. Following initiation of HAART, CD4+ was 300 and HIV viral load <103, but his neurological symptoms continued to deteriorate. Imaging revealed an increase in the size and number of lesions and enhancement of all the lesions. A stereotactic biopsy showed severe inflammatory and demyelinating lesions with marked infiltration by macrophages and T lymphocytes in the absence of a detectable infectious agent. Despite high doses of steroids, the patient died 3 months after admission. Autopsy showed two types of lesions: (1) active inflammatory PML changes with abundant JC virus, and intraparenchymal and perivascular infiltration by T lymphocytes, and (2) acute perivenous leukoencephalitis devoid of JC virus. Most lymphocytes were CD8+ lymphocytes; CD4+ lymphocytes were virtually absent. Two pathological reactions were associated with the paradoxical clinical deterioration related to dysregulation of the immune response characteristic of IRIS in PML: (1) an accentuation of JCV infection, and (2) a nonspecific acute perivenous leukoencephalitis. We suggest that both these types of lesions are due to an imbalance of CD8+/CD4+ T cells, with massive infiltration of the cerebral parenchyma by CD8+ cytotoxic T lymphocytes in the absence of sufficient CD4+ response. Better understanding of the mechanisms of the IRIS may enable prevention or cure of this severe, sometimes fatal complication of HAART.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Introduction of combination anti-retroviral treatment, also called highly active anti-retroviral therapy (HAART), has dramatically reduced morbidity and mortality in HIV infected patients [22], as well as improving their quality of life. These benefits are mainly due to decreased human immunodeficiency virus (HIV) viral load (VL) and restored immune function with increased CD4+ lymphocytes [1, 38]. The spectrum of acquired immune deficiency syndrome (AIDS)-related diseases has changed [3, 5]. With regard to the central nervous system (CNS), epidemiological studies show that most opportunistic infections for which effective treatment is available have decreased [39] and survival of patients with primary CNS non-Hodgkin’s lymphoma [20] and progressive multifocal leukoencephalopathy (PML) [7, 45] has improved.
Neuropathological studies confirm this favorable development [24, 30, 34, 46]. Some studies show the emergence of new forms of the classical complications of AIDS. “Burnt out” forms of toxoplasmosis, varicella zoster virus encephalitis (VZVE), PML or HIV encephalitis (HIVE) are described, in which inflammation or an infective agent cannot be detected [18, 47]. Destructive scar lesions with secondary Wallerian degeneration or neuronal apoptosis may explain the persistence or progression of neurological deficits and cognitive disorders despite efficient treatment [12] in some patients receiving HAART or, for PML, despite prolonged survival [15].
Fulminant inflammatory leukoencephalopathies associated with immune reconstitution have been reported recently in patients with HIVE who received HAART [29, 32]. These diseases may be due to the recently described “immune reconstitution inflammatory syndrome” (IRIS) defined as a “paradoxical deterioration in clinical status attributable to the recovery of the immune system during HAART” [42]. IRIS involving the CNS has been described in association with mycobacterial infection [10, 14], cytomegalovirus retinitis [23], and cryptococcal meningitis [26, 48]. In some patients with PML, magnetic resonance imaging (MRI) shows contrast enhancement following HAART [8], which also suggests an unusually intense inflammatory reaction, confirmed by cerebral biopsy [28, 33]. In most cases, this correlated with prolonged survival and was interpreted as a marker of both improved immune status and outcome [2, 8, 21, 28]; however, in rare instances [33, 40], it coincided with clinical and radiological deterioration.
We report an autopsy case of fulminant inflammatory leukoencephalopathy associated with immune restoration in a patient with AIDS-related PML who received HAART.
Case report
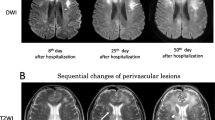
A 52-year-old Caribbean male had been HIV-1 positive for 16 years. He remained asymptomatic for 12 years and never received HAART. When aged 48, he presented with depression, psychomotor slowing and speech disorder. He was admitted to hospital 4 years later because of progression of cognitive impairment (reduction of verbal fluency, dysarthria, agnosia) and psycho-organic syndrome with delusions of persecution and threatening behavior. CD4+ T lymphocytes count was 117/µl and the HIV VL 314,072 copies/ml (>104). Initial MR) showed non-enhancing T1 hypo-intense and fluid attenuated inversion recovery pulse sequence (FLAIR) hyper-intense lesions in the left occipital and temporal lobes, left insula (Fig. 1a, b) and left middle cerebellar peduncle, consistent with PML. Cerebrospinal fluid (CSF) tests for pathogens (including PCR for JC virus) were negative. HAART (lopinavir boosted by ritonavir, lamivudine and zidovudine then didanosine) was started 4 weeks after admission. One month following initiation of HAART, HIV VL was <103 and a strong immunological response was observed (CD4+ T lymphocytes count, 284/µl). His neurological symptoms progressed rapidly with mental confusion, disorientation, aggressiveness and aphasia. A second MRI revealed an increase in the size and number of the cerebral lesions and overall, enhancement of all the lesions (Fig. 1c, d). A stereotactic biopsy of the left temporo-insular lesion showed severe inflammatory and demyelinating lesions with marked infiltration by macrophages and T lymphocytes in the absence of detectable infectious agent. These were interpreted as suggestive of IRIS. Despite high doses of steroids, his status remained unchanged and he died from septic shock, 3 months after admission.
MRI findings. a, b Initial MRI at admission. a FLAIR showing an hyper-intense lesion in the white matter of the left temporal lobe. b There is no enhancement of the lesion on T1-weighted image after gadolinium injection. c, d MRI 1 month after initiation of HAART. c FLAIR showing extension of the left temporal lesion to the occipital white mater, and presence of new lesions in the white matter of the right temporal lobe and cingulum of both sides. d Contrast enhancement at the periphery of the lesions is seen on T1-weighted image after gadolinium injection (MRI magnetic resonance imaging, FLAIR fluid attenuated inversion recovery pulse sequence)
Neuropathology
Methods
Postmortem examination was performed 24 h following death and was limited to the brain. Gross neuropathological examination was performed after 1-month 10% buffered formalin fixation, on coronal sections of the cerebral hemispheres and sections of the cerebellum and brain stem perpendicular to its axis.
For light microscopy, large slices involving the left cerebral hemisphere at three levels (head of caudate nucleus and anterior commissure, thalamus and gray commissure, occipital horn of the lateral ventricle), the right cerebral hemisphere at the level of the splenium of the corpus callosum, and the brain stem/cerebellum at the level of the dentate nuclei, were embedded in paraffin, and 15-μm-thick sections were cut and stained by hematoxylin and eosin and cresyl violet combined with Luxol-fast blue. Smaller blocks were also taken from a number of regions of the cerebral and cerebellar hemispheres including the deep gray nuclei, midbrain and brain stem, and embedded in paraffin. The same stains were used for the cerebral biopsy and postmortem samples, and included routine techniques and immunohistochemical methods using the following antibodies: anti-glial fibrillary acidic protein (GFAP; Dako, 1:1,000), anti-β-amyloid precursor protein (APP; Boehringer, 1:50), anti-HLADR (Dako, 1:50), anti-CD68 (Dako, 1:400), anti-CD3 (Novocastra,1:400), anti-CD20 (Dako, 1:200), anti-CD8 (Dako, 1:50), anti-CD4 (Novocastra, undiluted). The following organisms were looked for: herpes simplex type 1 and 2, VZV, CMV and Toxoplasma (by immunocytochemistry), JC and EBV (by in situ hybridization), Mycobacteria and fungi (by histochemistry).
Results
Cerebral biopsy
Inflammatory changes involved the cerebral cortex and underlying white matter and consisted of diffuse astrocytic and microglial activation and infiltration by CD3+ lymphocytes. In the white matter there was also massive myelin destruction and macrophagic reaction. T lymphocytes and macrophages/microglial cells were diffusely distributed in the cerebral parenchyma but also formed thick perivascular cuffs. Most T lymphocytes were CD8+. Only occasional CD20+ B lymphocytes were found. Macrophages and microglial cells strongly expressed HLA-DR. No infectious agent was identified, in particular p24 immunostaining for HIV and in situ hybridization (ISH) for JC virus and EBV were negative.
Postmortem study
Gross examination showed multiple demyelinating foci disseminated in the white matter of the cerebral hemispheres and cerebellum, mostly but not exclusively in the subcortical areas (Fig. 2a, b). These were mainly small lesions but in some regions, e.g., the left temporal lobe and insula, the lesions were more extensive, confluent and necrotic, extending to the occipital lobe; the subcortical white matter was spared (Fig. 2a). Demyelinating confluent lesions were also found in the left middle cerebral peduncle and right cerebellar cortex. There was no edema, no mass effect, no deviation of the midline structures, and no change in ventricular size or position.
Neuropathological findings. a Coronal section of the left cerebral hemisphere at the level of the lateral geniculate nucleus showing the scar of the biopsy (arrow), multiple demyelinating foci disseminated in the frontal and parietal white matter, mostly in the subcortical areas, and large confluent demyelinating lesions sparing the U fibers in the temporal white matter. Klüver-Barrera stain. b, c Horizontal section of the right cerebellar hemisphere showing multiple demyelinating foci in the white matter of the folia. c At higher magnification, the lesions include acute perivascular myelin destruction and perivenous inflammation reminiscent of perivenous leukoencephalitis. Klüver-Barrera stain. d–f Successive section of a recent PML lesion at the cortico-subcortical junction. d CD3 immunostaining showing marked T cell infiltration at the periphery of the lesion and around blood vessels. e CD68 immunostaining showing intense macrophage reaction predominant at the periphery of the lesion. f In situ hybridization for JCV showing numerous positive oligodendrocytes in the center of the lesion. g–i Successive sections of a perivascular inflammatory infiltrate at the periphery of a PML lesion. g Hematoxylin and eosin staining showing a large perivascular cuff. h CD8 immunostaining shows that most inflammatory cells are CD8+ T lymphocytes. i CD4 immunostaining shows that CD4+ T lymphocytes are absent (PML progressive multifocal leukoencephalopathy). b ×4; c ×50; d–f ×50; g–i ×200
Microscopic examination showed different types of lesion. Recent changes characteristic of PML were present particularly in the small demyelinating foci at the cortico-subcortical junction; they showed marked macrophagic/microglial activation (Fig. 2e), variable lympho-plasmacytic inflammation (Fig. 2d) and abundant enlarged oligodendrocytes containing JC virus-positive inclusion bodies (Fig. 2f). Chronic PML changes were present in the left insula, temporal and occipital lobes; they showed massive myelin destruction with focal necrotic cavitation, little or no inflammation and macrophage reaction, and rare JC virus-positive oligodendroglial inclusion bodies. GFAP immunostaining showed moderate astrocytic activation, but bizarre astrocytes were not found. The most striking feature was an intense infiltration by inflammatory cells. These were either diffuse in the cerebral parenchyma, or forming large perivascular cuffs (Fig. 2g). Inflammatory cells included CD68+ macrophage/microglial cells and CD3+ T lymphocytes. CD20+ B cells were rare. Most T lymphocytes were CD8+ lymphocytes (Fig. 2h); CD4+ lymphocytes were virtually absent (Fig. 2i). The inflammatory changes were found in association with PML changes, predominantly around them. JC virus was not found in the cerebellar lamellae and some cortico-subcortical frontal and parietal lesions. The lesions only showed recent myelin loss with many lipid-laden macrophages and marked perivenous inflammation (Fig. 2b, c). There were no multinucleated giant cells, and immunostaining for HIV was negative. No infectious agent other than JC virus could be identified by special stains, immunocytochemistry or ISH.
Discussion
PML is a devastating disease, usually rapidly fatal in advanced HIV infection. Although a number of antiviral agents with putative effect against JC virus have been reported, there is no proven curative therapy for PML. Recently, several reports have shown that HAART treatment significantly improved survival in AIDS patients with PML [7, 15, 45]. HAART is currently considered standard therapy for AIDS-related PML. Even so, PML may develop in AIDS patients while on HAART [44]. Also, despite good virological and immunological response to HAART, neurological and radiological signs in patients with prolonged survival may not improve and may even worsen [15, 44]. In some cases, this aggravated course can be due to extensive necrotic “burnt out” lesions [18, 47], particularly in cases co-infected with HIV [43]; these cases should become less frequent with earlier diagnosis and institution of HAART. In other instances, like our case, paradoxical deterioration of both clinical and radiological features results from an inflammatory syndrome secondary to HAART-induced restoration of the immune system.
An immune-reconstitution disease defined as “an acute symptomatic or paradoxical deterioration of a (presumably) pre-existing infection that is temporally related to recovery of the immune system” has been described in different types of immunodeficiency [6]. Unusual clinical inflammatory syndromes associated with underlying opportunistic infections after initiation of HAART, are being reported increasingly in AIDS patients [11, 14]. The name “immune-reconstitution inflammatory syndrome”(IRIS) was proposed [42] for this disease, which clinically had four diagnostic criteria: (1) patient with AIDS; (2) HAART induced a decrease in HIV-1 VL and an increase in CD4+ T lymphocytes; (3) symptoms consistent with an infectious/inflammatory condition appeared while on antiretroviral therapy; and (4) symptoms could not be explained by a newly acquired infection, the expected course of a previously recognized infection, or side effects of therapy. IRIS has been described for a wide variety of infections, mycobacterial, herpes zoster, Pneumocystis carinii pneumonia, hepatitis C and B, CMV retinitis, cryptococcal meningitis (for review see [42]).
The undesirable effects of immune reconstitution may present either as an inflammatory reaction unmasking a smoldering active infection, or a paradoxical immunopathological reaction to latent antigen or inactive infectious agent. As an example in the CNS, symptomatic cryptococcal meningitis [48], intracranial cryptococcoma [4], and aseptic meningitis [48] can occur following HAART initiation in patients with Cryptococcus neoformans infection. HAART can unmask latent CMV retinitis [23], or cause vitritis in patients successfully treated for CMV retinitis [25]. Comparable reactions have been observed in patients with HIVE. A severe leukoencephalopathy with intense perivascular infiltration by HIV-gp41-immunoreactive monocytes/macrophages was described in seven patients in whom HAART failed [29]. On the other hand, a diffuse perivascular and intraparenchymal infiltration by CD8+ T lymphocytes was reported as the main pathological feature in two cases [32]; one patient had moderate productive HIV infection of the brain, but in the second case, HIV-DNA could only be identified by in situ PCR.
In our patient, PML appears to have been accentuated following HAART initiation. This is the likely explanation of the intense inflammatory reaction around the lesions identified on initial MRI, and the diffuse nature of the more recent inflammatory lesions containing abundant JC virus in both cerebral hemispheres. These lesions are similar to those described in other case reports [28, 33, 40] on brain biopsies from patients with AIDS-related PML who worsened clinically and radiologically, shortly following HAART; or in whom HAART unmasked PML [21]. The intense perivascular inflammation correlates with the MRI changes of PML—contrast enhancement and/or mass effect—following HAART reported in several studies [2, 8, 37, 44]. The perilesional contrast enhancement correlated topographically with the inflammatory infiltrates found at brain biopsy, which were more severe in areas of maximum contrast enhancement [8, 28]. Follow-up MRI studies in patients with prolonged survival showed improvement of MRI changes from enhancing to non-enhancing lesions after 3–6 months [8, 21].
In our complete postmortem neuropathological study, in addition to the inflammatory PML changes, we found other white matter changes, i.e., perivascular myelin destruction, axonal sparing and perivenous inflammation in the right cerebellar cortex and fronto-parietal regions. JC virus was not identified in these areas. The lesions corresponded with acute disseminated encephalomyelitis (ADEM), a nonspecific immune complication of many infectious [41] or non-infectious conditions (anti-beta A4 vaccination) [36].
IRIS is regarded as an overactive response of a newly reconstituted immune system to infectious antigens already present in the patient when therapy started. The harmful complication of T cell restoration in PML is supported by two cases who presented with fatal IRIS in the first few weeks of HAART [40]. Brain biopsies showed prominent inflammation and evidence of JC virus by PCR. It was assumed that restoration of T cell function, which usually peaks 12 weeks after initiation of effective HAART [1, 9], allowed an influx of memory T cells that recognized JC virus antigens. Immunophenotyping of the T lymphocytes was not performed in that study, but our findings and those of Miralles [33] support a role for CD8+ cytotoxic cells. In the PML cases, and in the HIVE cases [32], most lymphocytes were CD8+, whereas CD4+ lymphocytes were virtually absent in brain.
CD8+ T lymphocytes form the majority of cytotoxic cells, and are present only in small numbers within the normal CNS [35]. In patients with AIDS-related PML, HAART-induced immune restoration usually produces a strong cellular immune response mediated by JC Virus-specific CD8+ cytotoxic T lymphocytes (CTL), which are instrumental in preventing disease progression [13, 27]. In pathological circumstances, CD8+ CTL responses may be so intense that CD8+ outnumber CD4+ T lymphocytes and may be harmful. In most case reports, the uncontrolled immune-inflammatory reaction occurred when HAART induced a rapid immune restitution in patients with profound CD4+ lymphopenia before treatment [32, 37, 40]; this was not the case in our patient. Altered CD4/CD8 ratios may explain the reactivation of a slowly progressive infection and increase of viral replication. JC virus-specific CD4+ T cell responses appear to play a critical role in the control of JCV infection, preventing PML development [16]. They are consistently lacking in the early stages of PML and are found in most PML survivors. This indicates that effective and prolonged antiretroviral therapy restores JCV-specific CD4 T cell responses. Indeed, help from CD4 T cells appears critical for sustaining macrophage and effective CD8+ CTL responses during viral infection [16, 31].
CD8+ cytotoxicity may also participate in the perivenous leukoencephalopathy associated with PML lesions in our case. This could occur by promoting myelin phagocytosis by monocytes/macrophages [19] or triggering oligodendrocyte apoptosis through ligating TNF receptor-like molecules by their corresponding ligands. An imbalance of intraparenchymal CD8+/CD4+ T-cells has already been observed in the early stages of multiple sclerosis and ADEM [17].
In conclusion, HAART-induced immune restoration is most often beneficial for patients with AIDS-related PML. Infrequently, early restoration of a pathogen-specific immune response may be “dysregulated”, and result in paradoxical clinical and radiological deterioration. Our clinico-pathological observation shows that this deterioration may be associated with two concurrent neuropathological changes: (1) accentuated JCV infection, and (2) acute perivenous leukoencephalitis. Both these lesions may be due to a dysregulation of the CD8+/CD4+ T cell balance with massive infiltration of the brain by CD8+ CTL in the absence of sufficient CD4+ cells. A better understanding of the underlying mechanisms of this new disease may help prevent or cure this severe, sometimes fatal complication of treatment.
References
Autran B, Carcelain G, Li TS, Blanc C, Mathez D, Tubiana R, Katlama C, Debre P, Leibowitch J (1997) Positive effects of combined antiretroviral therapy on CD4+ T cells homeostasis and function in advanced HIV cases. Science 277:112–116
Berger JR, Levy RM, Flomenhoft D, Dobbs M (1998) Predictive factors for prolonged survival in acquired immunodeficiency syndrome-associated progressive multifocal leukoencephalopathy. Ann Neurol 44:341–349
Bonnet F, Morlat P, Chene G, Mercie P, Neau D, Chossat I, Decoin M, Djossou F, Beylot J, Dabis F, groupe d’Epidémiologie Clinique du SIDA en Aquitaine (GECSA) (2002) Causes of death among HIV-infected patients in the era of highly active antiretroviral therapy, Bordeaux, France, 1998–1999. HIV Med 3:195–199
Breton G, Seilhean D, Chérin P, Herson S, Benveniste O (2002) Paradoxical intracranial cryptococcoma in a human immunodeficiency virus-infected man being treated with combination antiretroviral therapy. Am J Med 113:155–157
Brodt HR, Kkamps BS, Gute P, Knupp B, Staszewski S, Helm EB (1997) Changing incidence of AIDS-defining illnesses in the era of antiretroviral combination therapy. AIDS 11:1731–1738
Cheng VCC, Yuen K-Y, Chan W-M, Wong SSY, Ma ESK, Chan RMT (2000) Immunorestitution disease involving the innate and adaptive response. Clin Infect Dis 30:882–892
Clifford DB, Yiannoutsos C, Glicksman M, Simpson DM, Singer EJ, Piliero PJ, Marra CM, Francis GM, McArthur JC, Tyler KL, Tselis AC, Hyslop NE (1999) HAART improves prognosis in HIV-associated progressive multifocal leukoencephalopathy. Neurology 52:623–625
Collazos J, Mayo J, Martinez E, Blanco MS (1999) Contrast enhancing PML as an immune reconstitution event in AIDS patients. AIDS 13:1426–1428
Connick E, Lederman MM, Kotzin BL, Spritzler J, Kuritzkes DR, St Clair M, Sevin AD, Fox L, Chiozzi MH, Leonard JM, Rousseau F, D’Arc Roe J, Martinez A, Kessler H, Landay A (2000) Immune reconstitution in the first year of potent antiretroviral therapy and its relationship to virologic response. J Infect Dis 181:358–563
Crump JA, Tyrer MJ, Lloyd-Owen SJ, Han LY, Lipman MC, Johnson MA (1998) Miliary tuberculosis with paradoxical expansion of intracranial tuberculomas complicating immunodeficiency virus infection in a patient receiving highly active antiretroviral therapy. Clin Infect Dis 26:1008–1009
De Simone JA Pomerantz RJ, Babinchak TJ (2000) Inflammatory reactions in HIV-1infected persons after initiation of HAART. Ann Intern Med 133:447–454
Dore G, Correll PK, Ly Y, Kaldor JM, Cooper DA, Brew BJ (1999) Changes to AIDS dementia complex in the era of highly active antiretroviral therapy. AIDS 13:1249–1253
Du Pasquier RA, Clark KW, Smith PS, Joseph JT, Mazullo JM, De Girolami U, Letvin NL, Koralnik IJ (2001) JCV-specific cellular immune response correlates with a favorable clinical outcome in HIV-infected individuals with progressive multifocal leukoencephalopathy. J Neurovirol 7:318–322
Foudraine NA, Hovenkamp E, Notermans DW, Meenhorst PL, Klein MR, Lange JM, Miedema F, Reiss P (1999) Immunopathology as a result of highly active antiretroviral therapy in HIV-1-infected patients. AIDS 13:177–184
Gasnault J, Taoufik Y, Goujard C Kousignian P, Abbed K, Boue F, Dussaix E, Delfraissy JF (1999) Prolonged survival without neurological impairment in patients with AIDS-related progressive multifocal leukoencephalopathy on potent compbined antiretroviral therapy. J Neurovirol 5:421–429
Gasnault J, Kahraman M, Goer de Herve MG de, Durali D, Delfraissy JF, Taoufik Y (2003) Critical role of JC virus-specific CD4 T-cell responses in preventing progressive multifocal leukoencephalopathy. AIDS 17:1443–1449
Gay FW, Drye TJ, Dick GW, Esiri MM (1997) The application of multifactorial cluster analysis in the staging of plaques in early multiple sclerosis. Identification and characterisation of the primary demyelinating lesion. Brain 120:1461–1483
Gray F, Chrétien F, Vallat-Decouvelaere AV, Scaravilli F (2003) The changing pattern of HIV neuropathology in the HAART era. J Neuropathol Exp Neurol 62:429–440
Hartung HP, Grossman RI (2001) ADEM: distinct disease or part of MS spectrum? Neurology 56:1257–1260
Hoffmann C, Tabrizian S, Wolf E, Eggers C, Stoehr A, Plettenberg A, Buhk T, Stellbrink HJ, Horst HA, Jager H, Rosenkranz T (2001) Survival of AIDS patients with primary central nervous system lymphoma is dramatically improved by HAART-induced immune recovery. AIDS 15:2119–2127
Hoffmann C, Horst HA, Albrecht H, Schlote W (2003) Progressive multifocal leukoencephalopathy with unusual inflammatory response during antiretroviral treatment. J Neurol Neurosurg Psychiatry 74:1142–1144
Hogg RS, O’Shaughnessy MV, Gataric N, Yip B, Craib K, Schechter MT, Montaner JS (1997) Decline in deaths from AIDS due to new antiretrovirals. Lancet 349:1294
Jacobson MA, Zegans M, Pavan PR, O’Donnell JJ, Sattler F, Rao N, Owens S, Pollard R (1997) Cytomegalovirus retinitis after initiation of highly active antiretroviral therapy. Lancet 349:1443–1445
Jellinger KA, Setinek U, Drlicek M, Böhm G, Steurer A, Lintner F (2000) Neuropathology and general autopsy findings in AIDS during the last years. Acta Neuropathol 100:213–220
Karavellas MP, Plummer DJ, Macdonald JC, et al (1999) Incidence of immune recovery vitritis in cytomegalovirus retinitis patients following institution of successful HAART. J Infect Dis 179:697–700
King MD, Perlino CA, Cinnamon J, Jernigan JA (2002) Paradoxical recurrent meningitis following therapy of cryptococcal meningitis: an immune reconstitution syndrome after initiation of highly active antiretroviral therapy. Int J STD AIDS 13:724–726
Koralnik IJ (2004) New insight into progressive multifocal leukoencephalopathy. Curr Opin Neurol 17:365–370
Kotecha N, George MJ, Smith TW, Corvi F, Litofsky NS (1998) Enhancing progressive multifocal leukoencephalopathy: an indicator of improved immune status? Am J Med 105:541–543
Langford TD, Letendre SL, Marcotte TD, Ellis RJ, McCutchan JA, Grant I, Mallory ME, Hansen LA, Archibald S, Jernigan T, Masliah E, the HNRC group (2002) Severe, demyelinating leukoencephalopathy in AIDS patients on antiretroviral therapy. AIDS 16:1019–1029
Masliah E, DeTeresa RM, Mallory ME, Hansen LA (2000) Changes in pathological findings at autopsy in AIDS cases for the last 15 years. AIDS 14:69–74
Matloubian M, Concepcion RJ, Ahmed R (1994) CD4+ T cells are required to sustain CD8+ cytotoxic T-cell responses during chronic viral infection. J Virol 68:8056–8063
Miller RF, Isaacson PG, Hall-Craggs M, Lucas S, Gray F, Scaravilli F, An SF (2004) Cerebral CD8+ lymphocytosis in HIV-1 infected patients with immune restoration induced by HAART. Acta Neuropathol 108:17–23
Miralles P, Berenguer J, Lacruz C, Cosin J, Lopez JC, Padilla B, Munoz L, Garcia-de-Viedma D (2001) Inflammatory reactions in progressive multifocal leukoencephalopathy after highly active antiretroviral therapy. AIDS 15:1900–1902
Morgello S, Mahboob R, Yakoushina T, Khan S, Hague K (2002) Autopsy findings in human immunodeficiency virus-infected population over 2 decades: influences of gender, ethnicity, risk factors and time. Arch Pathol Lab Med 126:182–190
Neumann H, Medana IM, Bauer J, Lassmann H (2002) Cytotoxic T lymphocytes in autoimmune and degenerative CNS disease. Trends Neurosci 25: 313–319
Nicoll JAR, Wilkinson D, Holmes C, Steart P, Markham H, Weller RO (2003) Neuropathology of human Alzheimer disease after immunization with amyloid-β peptide: a case report. Nat Med 9: 448–452
Nuttall JJC, Wilmshurst JM, Ndondo AP, Yeats J, Corcoran C, Hussey GD, Eley BS (2004) Progressive multifocal leukoencephalopathy after initiation of highly active antiretroviral therapy in a child with advanced human immunodeficiency virus infection: a case of immune reconstitutioninflammatory syndrome. Pediatr Infect Dis J 23:683–685
Pakker NG, Ross MTL, Leeuwen R van, Jong MD de, Koot M, Reiss P, lange JM, Miedema F, Danner SA, Schellekens PT (1997) Patterns of T-cell repopulation, virus load replication, and restoration of T-cell function on HIV-infected persons during therapy with different antiretroviral agents. J Acquir Immune Defic Syndr Hum Retrovirol 16:318–326
Sacktor N, Lyles RH, Skolasky R, Kleeberger C, Selnes OA, Miller EN, Becker JT, Cohen B, McArthur JC (2001) HIV associated neurologic disease incidence changes: Multicenter AIDS cohort study, 1990–1998. Neurology 56:257–260
Safdar A, Rubocki RJ, Horvath JA, Narayan KK, Waldron RL (2002) Fatal immune restoration disease in human immunodeficiency virus type 1-infected patients with progressive multifocal leukoencephalopathy: impact of antiretroviral therapy-associated immune reconstitution. Clin Infect Dis 35:1250–1257
Scaravilli F, Esiri M, Sharer L, Gray F (2004) Infections of the central nervous system. In: Gray F, DeGirolami U, Poirier J (eds) Escourolle and Poirier Manual of Basic Neuropathology, 4th edn, Chapter 5. Butterworth Heinemann, Philadelphia, pp 113–144
Schmidbauer M, Budka H, Shah KV (1990) Progressive multifocal leukoencephalopathy (PML) in AIDS and in the pre-AIDS era. A neuropathological comparison using immunocytochemistry and in situ DNA hybridisation for virus detection. Acta Neuropathol 80:375–380
Shelburne SA, Hamill RJ, Rodriguez-Barradas MC, Greenberg SB, Atmar RL, Musher DW, Gathe JC Jr, Visnegarwala F, Trautner BW(2002) Immune reconstitution inflammatory syndrome. Emergence of a unique syndrome during HAART. Medicine 81:213–227
Tantisiriwat W, Tebas P, Clifford DB, Powderly WG, Fichtenbaum CJ (1998) Progressive multifocal leukoencephalopathy in patients with AIDS receiving highly active antiretroviral therapy. Clin Infect Dis 28:1152–1154
Tassié JM, Gasnault J, Bentata M, Deloumeaux J, Boué F, Billaud E, Costagliola D, the French Hospital Database on HIV (1999) Survival improvement of AIDS-related progressive multifocal leukoencephalopathy in the era of protease inhibitors. AIDS 13:1881–1887
Vago L, Bonetto S, Nebuloni M, Duca P, Carsana L, Zerbi P, D’Arminio-Monforte A (2002) Pathological findings in the CNS of AIDS patients on assumed ART regimens: retrospective study of 1597 autopsies. AIDS 16:1925–1928
Vallat-Decouvelaere AV, Chrétien F, Lorin de la Grandmaison G, Carlier R, Force G, Gray F (2003) La pathologie du système nerveux central liée au VIH à l’ère des multithérapies. Ann Pathol 23:408–423
Woods ML, MacGinley R, Eisen DP, Allworth AM (1998) HIV combination therapy: partial immune restitution unmasking latent cryptococcal infection. AIDS 12:1491–1494
Acknowledgements
Supported by grants to Dr. Gray from Agence Nationale de Recherches sur le SIDA (ANRS) and Ensemble Contre le SIDA (ECS). The authors wish to thank Dr. Catherine Keohane for kindly reviewing the English, Dr. Patrice LeFloch-Progent in the Service Central d’Anatomie et Cytologie Pathologiques at Hôpital Cochin (Pr. M.C. Vacher-Lavenu) who performed the autopsy, and Marie-Annick Bretel, Patrice Castagnet, Katia Dossou, Isabelle Levesque and Claudine Poron, for histological preparations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vendrely, A., Bienvenu, B., Gasnault, J. et al. Fulminant inflammatory leukoencephalopathy associated with HAART-induced immune restoration in AIDS-related progressive multifocal leukoencephalopathy. Acta Neuropathol 109, 449–455 (2005). https://doi.org/10.1007/s00401-005-0983-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-005-0983-y