Abstract
The distribution pattern of NOGO-A protein, an important axon growth inhibitory molecule and member of the reticulon family, has been investigated in the adult human brain, spinal cord, retina and dorsal root ganglia. Intense NOGO-A immunoreactivity was detected in oligodendroglial cell bodies and their myelin sheaths in nerve fibre tracts of the central nervous system. Furthermore, numerous populations of neurons in the brain and spinal cord expressed NOGO-A to a variable extent in their cell bodies and neurites, suggesting additional, as-yet-unknown, functions of this protein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the mammalian peripheral nervous system (PNS), lesioned nerve fibres have the capacity for extensive regeneration followed by functional recovery. However, damaged nerve fibres in the central nervous system (CNS) normally demonstrate an abortive sprouting response without any significant regeneration. Numerous investigations have indicated a range of post-traumatic events that contribute to the lack of axonal regeneration in the lesioned CNS, including glial scar formation, a lack of trophic support and the presence of growth-inhibitory molecules [15]. The latter comprise extracellular matrix proteins such as semaphorin 3A [11], chondroitin sulphate proteoglycans (CSPG) [1] and myelin-associated proteins such as NOGO-A, myelin associated glycoprotein (MAG) and oligodendrocyte myelin glycoprotein (OMgp) [7, 16, 17, 18].
NOGO-A belongs to the reticulon gene family, an eucaryotic family with a broad expression pattern but, as yet, unknown function [9]. The protein has been identified as an important negative regulator of regeneration and plasticity within the adult mammalian CNS [2, 3, 6, 12, 13, 16, 17].
In rats and mice, NOGO-A mRNA and protein are found mainly in oligodendrocytes but also in various populations of neurons throughout the nervous system [4, 19]. Neuronal expression is pronounced during development and lower in the adult nervous system. In the human nervous system, the distribution of NOGO-A has only been determined in the spinal cord at the level of mRNA [5]. To provide a more comprehensive description of the distribution of NOGO-A, we have investigated the expression of NOGO-A protein in the human nervous system.
Material and methods
Post-mortem brain and spinal cord samples were obtained from five patients who had not suffered from any neurological disorder (for details see Table 1). The study was approved by the Aachen University Ethics Committee. The tissue was fixed in 4% buffered formaldehyde, dehydrated and embedded in paraffin wax.
Western blotting
Human frontal cortex homogenate (50 ng) was loaded on a 8% (w/v) SDS-polyacrylamide gel. Following electrophoresis, the separated proteins were transferred to a PVDF membrane in a semi-dry blotter for 2 h at 1 mA/cm2. Membranes were blocked overnight at 4°C in PBS-T containing 5% de-fatted milk powder. The monoclonal antibody 3A6 was generated against a peptide sequence of human NOGO-A; the monoclonal antibody 11C7 was generated against a rat peptide sequence [10]. Both antibodies were used as purified IgG at a concentration of 1 nM/l overnight at 4°C. Furthermore, on lane 2 and 4 excess NOGO-A antigenic peptide was added to the primary antibody solution prior to incubation with the proteins on the PVDF membrane. Subsequently, the horseradish peroxidase (HRP)-conjugated anti-mouse secondary antibody (diluted 1:15,000, Pierce) was incubated for 1 h at room temperature. The blot was incubated with enhanced chemiluminescence (ECL) substrate (Pierce) and exposed to a Kodak film.
Peroxidase immunohistochemistry
Sections of 5-μm thickness were collected onto poly-l-lysine-coated slides and allowed to dry. They were de-waxed in xylene and rehydrated. Endogenous peroxidase activity was blocked by incubation in 0.1 M phosphate-buffered saline (PBS) containing 0.7% H2O2 for 30 min. Microwave treatment in 10 mM citrate buffer (pH 6), three times for 3 min, was followed by blockade of non-specific binding by incubation in 3% normal goat serum in 0.5% Triton X-100 diluted in 0.1 M PBS for 30 min and subsequent incubation with the primary antibody, overnight at room temperature. Following extensive rinsing steps in 0.1 M PBS, sections were incubated in biotinylated horse anti-mouse antibody (diluted 1:500, Vector Laboratories) for 1 h at room temperature. As described earlier, incubation with the biotinylated secondary antibody was followed by the Vector ABC system and a subsequent incubation in diaminobenzidine for visualization of the reaction product [14]. For negative controls the primary antibody was omitted.
For a qualitative description of the relative intensity of immunoreactivity revealed in the various populations of labelled neurons and in oligodendrocytes, an arbitrary rating scale for the mean staining intensity of the labelled profiles was chosen, ranging from 0 to 5 (0, no staining; 1, very weak staining, hardly above background level; 2, weak staining; 3, moderate intensity; 4, strong staining; 5, most intense staining).
Immunofluorescence
Sections were de-waxed in xylene and rehydrated. Microwave treatment in 10 mM citrate buffer (pH 6), three times for 3 min, was followed by blockade of non-specific binding by incubation in 3% normal goat serum in 0.5% Triton X-100 in 0.1 M PBS for 30 min and subsequent incubation overnight at room temperature with the anti-NOGO-A antibody and one of the following polyclonal primary antibodies: anti-glial fibrillary acidic protein (GFAP; diluted 1:2,500, code Z-0334, Dako), anti-neurofilament (NF; 200 kDa, diluted 1:2,500, N-4142, Sigma), anti-myelin basic protein (MBP; diluted 1:1,000, Ab980, Chemicon), anti-synaptophysin (diluted 1:1,000, A0010, Dako) and subsequently with Alexa 594 (red-fluorescence)-conjugated goat anti-mouse and Alexa 488 (green fluorescence)-conjugated goat anti-rabbit secondary antibodies (diluted 1:500, Molecular Probes). For negative controls, the primary antibodies were omitted.
For NOGO-A and CNPase double staining, we used the tyramide signal amplification kit (TSA Cyanine 3 system, NEL704A, Perkin-Elmer Life Sciences). Briefly, the sections were incubated with the anti-NOGO-A antibody at a concentration of 1 μg/ml overnight. Incubation with a biotinylated horse anti-mouse antibody (1:500, BA2000, Vector) for 1 h, rinsing in 0.05% Tween20 and blocking with the provided reagent for 30 min was followed by incubation with TSA Cyanine 3 (1:50) for 7 min. Next, the slides were incubated with the anti-CNPase primary antibody (1:200, SMI91, Sternberger Monoclonals) overnight and a Cy 2-conjugated goat anti-mouse secondary antibody (1:100, Jackson Laboratories) for 3 h at room temperature and finally cover-slipped with 50% glycerine.
Sections were then examined by standard epifluorescence with a Zeiss Axioplan microscope or by confocal microscopy with a Zeiss inverted microscope fitted with a Bio-Rad MRC1024 laser scanning imaging system. An argon-krypton laser beam was used with excitation at 488 nm for Cy2 visualisation and at 586 nm for Cy3 visualisation. Single confocal plane images (786×512 pixels) were collected with the laser in slow scanning mode with Kalman filtering.
Results
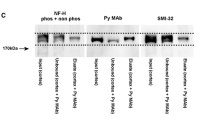
The 3A6 and the 11C7 antibody, both generated against a NOGO-A peptide sequence, specifically bind human NOGO-A with high affinity (Fig. 1). An overview of the distribution of NOGO-A protein can be seen in Table 2. A more detailed description is presented below. Since both 3A6 and 11C7 antibodies showed a comparable expression pattern, the data presented are those generated by the 11C7 antibody.
Western blot of human brain homogenate with 3A6 and 11C7. Western blot with human frontal cortex homogenate demonstrates specific high-affinity binding of the 3A6 (lane 1) and the 11C7 (lane 3) antibodies to human NOGO-A protein. Co-incubation with NOGO-A specific antigenic peptide completely abolishes the signal (lane 2 and 4). The + and − symbols reflect the preincubation of the NOGO-A antibodies with antigenic peptide or control buffer, respectively
Cerebral cortex
In the cerebral cortex, the intensity of NOGO-A staining was generally moderate (rating scale 2–3). Approximately 50–60% of large diameter pyramidal neurons located in layer III and V displayed NOGO-A staining (Fig. 2A). In layers I/II, IV and VI fewer neurons (approximately 10%) demonstrated NOGO-A immunoreactivity. In the ventricular system, NOGO-A immunoreactivity was neither detected in ependymal cells nor in the choroid plexus. Furthermore, meningothelial cells and blood vessels were also NOGO-A immunonegative (rating scale 0).
NOGO-A expression in neurons. A In the cerebral cortex, NOGO-A immunohistochemistry displays pyramidal cells mainly in layers III and V. B The retina shows immunopositive cells in the ganglion cell (arrow)- (a) and the inner- (b) and outer- (c) nuclear layers; retinal ganglion cells display strongest immunoreactivity. In the cerebellum (C), only some Purkinje cells contain detectable amounts of NOGO-A. In the molecular (left) and granule cell (right) layers, cells are rarely stained (arrow) which might represent Golgi neurons or basket cells. D In the inferior olive, all neurons display strong immunoreactivity for NOGO-A in the their cell body. E In pyramidal cells of the CA1–4 region of the hippocampus, NOGO-A labelling is granular and spread over the cell body. F In the spinal cord, many motor neurons show NOGO-A labelling, often with several granules spread throughout the cytosol. G All neurons of the dorsal root ganglia display intense, often homogenous immunoreactivity in the cell bodies, the nucleus is devoid of staining. Original magnification A see scale bar; B–E see scale bar in B and D; F, G x640
Hippocampus
In the hippocampus, NOGO-A immunoreactivity was restricted to all pyramidal cell bodies of the CA1–4 regions (Fig. 2E). The staining intensity was rather weak (rating scale1–2) and appeared granular, which is in contrast to the diffuse, moderate intensity of staining observed in the cell body of most other populations of neurons. The nuclei of immunoreactive neurons were devoid of staining. In the white matter, oligodendrocytes and their myelin sheaths were strongly stained with the NOGO-A antibody (rating scale 4–5).
Cerebellum
In the cerebellum, granule neurons were NOGO-A negative (rating scale 0). Less than 1% of Purkinje cells were moderately stained (rating scale 2–3, not shown) and in the molecular and granule cell layers, less than 1% of neuronal cell bodies (possibly Golgi neurons or basket cells) were immunopositive (rating scale 2–3, arrow, Fig. 2C). No immunoreactivity was found in the deep cerebellar nuclei. In the white matter oligodendrocytes and their myelin sheaths were NGO-A immunoreactive.
Basal ganglia and brain stem
In the brain stem, multiple neuronal populations displayed relatively moderate to strong NOGO-A immunoreactivity (rating scale 3–4). In labelled cell populations, which included the inferior olive (e.g. Fig. 2D) and most long projection neurons (such as the red nucleus) 80–90% of neurons were immunopositive. In the substantia nigra, no specific immunoreactivity could be detected. However, it cannot be discounted that melanin granules within the neuronal cell bodies may have masked weak staining. In the putamen, pallidum and the thalamus, approximately 60–70% of neurons, with an emphasis on neurons with larger cell bodies, were moderately NOGO-A positive (rating scale 2–3). Again, in the white matter, oligodendrocyte cell bodies and their myelin sheaths were NOGO-A immunopositive.
Retina
The retina was strongly immunoreactive for NOGO-A. Retinal ganglion cells were intensely stained (rating scale 4–5) and more moderate levels (rating scale 3–4) of staining were detected in the inner and outer molecular layers (Fig. 2B).
Spinal cord and dorsal root ganglia
The meninges and blood vessels were NOGO-A negative. In the spinal cord grey matter, about 80% of motoneurons and Clarke’s nucleus neurons, mostly with large cell bodies, were moderately to strongly NOGO-A positive (rating scale 3–4, e.g. Fig. 2F). Furthermore, about 10–20% of interneurons, mostly from laminae IV to VI were immunopositive. Double immunofluorescence with an antibody against synaptophysin showed no overlap of NOGO-A with the synaptic marker (Fig. 3H–J). The sensory neurons of the dorsal root ganglia and their neurites revealed a strong, diffuse immunoreactivity within the cell body (rating scale 4–5), whereas Schwann cells did not show any specific staining (Fig. 2G).
NOGO-A expression in oligodendrocytes. A In the brain and spinal cord, oligodendrocytic cell bodies (arrows) are strongly labelled for NOGO-A. In B, double staining with NOGO-A (red) and neurofilament (green) shows no overlap. Instead, axons are surrounded by the NOGO-A-positive myelin sheaths. C Double staining with GFAP (green) reveals no NOGO-A staining in astrocytic cell bodies or processes; sometimes the distribution on the inner and outer myelin membrane can be differentiated (arrow). D Confocal microscopy of double staining with MBP (red) shows no overlap in compact myelin which demonstrates that NOGO-A (green) is not associated with compact myelin. On some myelin rings, the distribution of NOGO-A on the inner and outer myelin membrane can be differentiated (arrows). E–G Double immunofluorescence for NOGO-A (red) and CNPase (green) in spinal cord white matter demonstrates the presence of NOGO-A in oligodendrocytes. H–J Confocal microscopy of double immunofluorescence for NOGO-A (red) and synaptophysin (green) in spinal cord ventral horn. Arrows indicate lipofuscin autofluorescence within motoneurons. There is no overlap of both proteins in synaptic structures. Original magnification: A ×320; B, C ×400; D ×1,200; E–J ×640
In brain and spinal cord white matter, the NOGO-A antibody stained myelin sheaths as well as oligodendrocytic cell bodies (rating scale 4–5, e.g. in spinal cord, Fig. 3A). In myelin, NOGO-A did not co-localize with MBP and is therefore not present in compact myelin. However, the inner and outer myelin membrane contained detectable levels of NOGO-A (Fig. 3D). Double immunohistochemistry with an antibody against CNPase confirmed the oligodendroglial nature of these NOGO-A-positive cells (Fig. 3E–G). Furthermore, double staining with the astrocyte-specific marker, GFAP, revealed no co-localization (Fig. 3C).
Discussion
The present investigation has demonstrated the spatial distribution of NOGO-A protein in the adult human nervous system. In agreement with data from rat and mouse [4, 19], NOGO-A was detected in oligodendroglial cell bodies as well as in the inner and outer membranes of CNS myelin. This is consistent with its documented function as a myelin-associated neurite growth inhibitor. Furthermore, as in rodents, NOGO-A protein was detected in the cell bodies and neurites of a number of different populations of neurons, suggesting additional as-yet-unknown functions of the protein.
In the human brain and spinal cord, multiple neuronal populations were labelled. Comparing different cerebral regions, the brain stem contained by far the most NOGO-A-positive neurons. Using the arbitrary five-point scale for the relative intensity of NOGO-A staining described above (0, no staining to 5, intense staining), nearly all brain stem nuclei, including the red nucleus, the inferior olive and many cranial nerve nuclei were relatively strongly stained (scale 3–4). The neuronal distribution of NOGO-A in the human spinal cord and dorsal root ganglia corresponds to that previously described on the level of mRNA and to the results in mice and rats [4, 19]. In the brain, however, differences were found in the basal ganglia and the cerebellum. In mice, the substantia nigra was stained for NOGO-A, whereas we could not find detectable levels in our material. In the cerebellum, the expression of NOGO-A was generally lower in the human CNS than has been reported in either rat or mouse [4, 19]. Furthermore, granule cells in mice and the deep cerebellar nuclei in rats were immunopositive. Neither of these cell populations were labelled in the present investigation. Nonetheless, in general, the neuronal distribution of NOGO-A in the human CNS corresponds well with that already published using experimental animals.
NOGO-A belongs to the reticulon family [9]. In accordance with other members of this protein family, cell culture experiments on experimentally derived oligodendrocytic cell bodies demonstrated the localisation of NOGO-A in the endoplasmic reticulum (ER) and the Golgi complex [10]. In the present post-mortem human material, the conditions of fixation and tissue preparation are sub-optimal when compared to those employed in experimental investigations, making a definitive interpretation of the subcellular localisation within this material extremely difficult. The present data demonstrate both diffuse and granular immunoreactivity within the cell cytoplasm (the nucleus being devoid of staining). The reason(s) for the differences in the quality, and intensity of staining, as well as for different sub-populations of neurons being stained remain uncertain. However, it is tempting to highlight the trend that large diameter projection neurons with long axons (i.e. those populations of neurons that require high protein synthesis and transport rates) were those that displayed the most intense NOGO-A immunoreactivity.
Apart from the cytoplasmic distribution in neurons, Liu and colleagues [8] found NOGO-A at the post-synaptic zone of rat motoneurons. In our material, double immunofluorescence with synaptophysin showed no overlap of NOGO-A with synaptic structures in the human brain or spinal cord.
The other main cell population labelled in the brain and spinal cord were oligodendroglia. This is in line with the function of NOGO-A as a myelin-associated inhibitor of neuronal outgrowth and plasticity. Several studies using transgenic and knockout animals have demonstrated an inhibitory function of NOGO-A on axonal regeneration, both in vitro and in vivo [2, 3, 6, 12, 13, 16], although others have produced more equivocal data [20]. The present data reveal the presence of NOGO-A on the inner and outer myelin membrane, which is identical to the distribution already described in the rat and mouse CNS [4, 19]. The presence of cytoplasmic NOGO-A immunoreactivity within the oligodendrocytic cell bodies, similar to that identified in neuronal cell bodies, may also suggest a localisation in the ER; however, as pointed out earlier, this remains highly speculative in the present post-mortem material. In contrast to oligodendrocytes, which are the myelinating cells of the CNS, Schwann cells in the PNS do not express NOGO-A.
In summary, our data on the expression of NOGO-A in the human nervous system are in line with those previously described on the level of mRNA and to the distribution in experimental animals. Beside the growth inhibitory function, the widespread presence of the protein in neuronal cells suggests hitherto unknown functions, perhaps associated with the complex network of the ER.
References
Bradbury EJ, Moon LD, Popat RJ, King VR, Bennett GS, Patel PN, Fawcett JW, McMahon SB (2002) Chondroitinase ABC promotes functional recovery after spinal cord injury. Nature 416:636–640
Chen MS, Huber AB, Haar ME van der, Frank M, Schnell L, Spillmann AA, Christ F, Schwab ME (2000) Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature 403:434–439
GrandPre T, Nakamura F, Vartanian T, Strittmatter SM (2000) Identification of the Nogo inhibitor of axon regeneration as a reticulon protein. Nature 403:439–444
Huber AB, Weinmann O, Brosamle C, Oertle T, Schwab ME (2002) Patterns of nogo mRNA and protein expression in the developing and adult rat and after CNS lesions. J Neurosci 22:3553–3567
Josephson A, Widenfalk J, Widmer HW, Olson L, Spenger C (2001) NOGO mRNA expression in adult and fetal human and rat nervous tissue and in weight drop injury. Exp Neurol 169:319–328
Kim JE, Li S, GrandPre T, Qiu D, Strittmatter SM (2003) Axon regeneration in young adult mice lacking Nogo-A/B. Neuron 38:187–199
Liu BP, Fournier A, GrandPre T, Strittmatter SM (2002) Myelin-associated glycoprotein as a functional ligand for the Nogo-66 receptor. Science 297:1190–1193
Liu YY, Jin WL, Liu HL, Ju G (2003) Electron microscopic localization of Nogo-A at the postsynaptic active zone of the rat. Neurosci Lett 346:153–156
Oertle T, Schwab ME (2003) Nogo and its paRTNers. Trends Cell Biol 13:187–194
Oertle T, Haar ME van der, Bandtlow CE, Robeva A, Burfeind P, Buss A, Huber AB, Simonen M, Schnell L, Brosamle C, Kaupmann K, Vallon R, Schwab ME (2003) Nogo-A inhibits neurite outgrowth and cell spreading with three discrete regions. J Neurosci 23:5393–5406
Pasterkamp RJ, Anderson PN, Verhaagen J (2001) Peripheral nerve injury fails to induce growth of lesioned ascending dorsal column axons into spinal cord scar tissue expressing the axon repellent Semaphorin3A. Eur J Neurosci 13:457–471
Pot C, Simonen M, Weinmann O, Schnell L, Christ F, Stoeckle S, Berger P, Rulicke T, Suter U, Schwab ME (2002) Nogo-A expressed in Schwann cells impairs axonal regeneration after peripheral nerve injury. J Cell Biol 159:29–35
Prinjha R, Moore SE, Vinson M, Blake S, Morrow R, Christie G, Michalovich D, Simmons DL, Walsh FS (2000) Inhibitor of neurite outgrowth in humans. Nature 403: 383–384
Schmitt AB, Brook GA, Buss A, Nacimiento W, Noth J, Kreutzberg GW (1998) Dynamics of microglial activation in the spinal cord after cerebral infarction are revealed by expression of MHC class II antigen. Neuropathol Appl Neurobiol 24:167–176
Schwab ME, Bartholdi D (1996) Degeneration and regeneration of axons in the lesioned spinal cord. Physiol Rev 76:319–370
Simonen M, Pedersen V, Weinmann O, Schnell L, Buss A, Ledermann B, Christ F, Sansig G, Putten H van der, Schwab ME (2003) Systemic deletion of the myelin-associated outgrowth inhibitor Nogo-A improves regenerative and plastic responses after spinal cord injury. Neuron 38:201–211
Spillmann AA, Bandtlow CE, Lottspeich F, Keller F, Schwab ME (1998) Identification and characterization of a bovine neurite growth inhibitor (bNI-220). J Biol Chem 273:19283–19293
Wang KC, Koprivica V, Kim JA, Sivasankaran R, Guo Y, Neve RL, He Z (2002) Oligodendrocyte-myelin glycoprotein is a Nogo receptor ligand that inhibits neurite outgrowth. Nature 417:941–944
Wang X, Chun SJ, Treloar H, Vartanian T, Greer CA, Strittmatter SM (2002) Localization of Nogo-A and Nogo-66 receptor proteins at sites of axon-myelin and synaptic contact. J Neurosci 22:5505–5515
Zheng B, Ho C, Li S, Keirstead H, Steward O, Tessier-Lavigne M (2003) Lack of enhanced spinal regeneration in Nogo-deficient mice. Neuron 38:213–224
Acknowledgements
The authors would like to thank K. Pech and A. Knischewski for excellent technical assistance. These investigations were supported by a grant from the BMBF (Bundesministerium für Bildung und Forschung, 01K09804/4).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buss, A., Sellhaus, B., Wolmsley, A. et al. Expression pattern of NOGO-A protein in the human nervous system. Acta Neuropathol 110, 113–119 (2005). https://doi.org/10.1007/s00401-004-0942-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-004-0942-z