Abstract
The blood-brain barrier (BBB), mediated by endothelial tight junctions, is defective in malignant gliomas such as glioblastoma, resulting in cerebral edema and contrast enhancement upon neuroradiological examination. The mechanisms underlying BBB breakdown are essentially unknown. Since non-neoplastic astrocytes are required to induce BBB features of cerebral endothelial cells, it is conceivable that malignant astrocytes have lost this ability due to dedifferentiation. Alternatively, glioma cells might actively degrade previously intact BBB tight junctions. To examine the latter hypothesis, we have employed a transepithelial electrical resistance breakdown assay using monolayers of the C7 subclone of Madin-Darby canine kidney (MDCK-C7) cells forming tight junctions similar to those of BBB endothelial cells. We found that glioblastoma primary cells co-cultured with the MDCK-C7 monolayer (without direct contact of the two cell types) resulted in marked breakdown of electrical resistance, whereas primary cultures derived from low-grade gliomas (fibrillary astrocytoma, oligoastrocytoma) showed delayed or no effects. These results suggest that malignant gliomas have acquired the ability to actively degrade tight junctions by secreting soluble factors, eventually leading to BBB disruption within invaded brain tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The blood-brain barrier (BBB) protects the microenvironment of the central nervous system, which is essential for its normal function. The BBB is formed by highly specialized endothelial cells characterized by lack of fenestrations, rare endocytotic vesicles and a network of complex tight junctions between endothelial cells [26, 31]. Normal astrocytes and possibly other cell types in the brain secrete factors that are required to induce BBB features of endothelial cells [1, 8, 26] and some of these factors have now been identified [13].
In malignant gliomas, such as glioblastoma, the BBB is leaky, as visualized by immunohistochemistry of plasma proteins using biopsy specimens [29] as well as by heterogeneous contrast enhancement upon neuroradiological examination [25]. In contrast, the BBB is usually preserved in low-grade (WHO grade II) gliomas such as astrocytoma and oligodendroglioma. The increased transcellular and paracellular passage of molecules across the defective BBB leads to brain edema and substantially contributes to patient morbidity [22]. Glioblastoma vessels, in particular those with endothelial hyperplasia, commonly show abnormal structural features of endothelial cells, such as frequent fenestrations, prominent pinocytotic vesicles, lack of perivascular glial endfeet, as well as opening, loss and/or abnormal morphology of tight junctions [6, 14]. Accordingly, immunohistochemical studies have revealed that some transmembrane tight junction components are down-regulated in glioblastoma microvessels, including occludin and claudin-3 [23, 32], while claudin-5 and the intracellular tight junction component ZO-1 are additionally down-regulated in hyperplastic vessels [14, 28]. Abnormal expression of these tight junction components has been associated with loosening of the BBB, as described for claudin-5-deficient mice [20].
Two hypotheses may explicate the pathogenesis of BBB breakdown in malignant gliomas. First, it is conceivable that dedifferentiated glioma cells have lost the ability of inducing BBB features in endothelial cells, making the exuberant de novo vascular proliferations typical of glioblastomas functionally defective. Second, glioma cells might secrete factors that actively open or degrade initially intact BBB tight junctions. The finding of structural and functional BBB impairment even in peritumoral brain and in the invasion area [2, 5] indeed suggests involvement of factors inactivating the BBB. However, experimental evidence supporting either hypothesis is so far missing. To examine the latter hypothesis, i.e., active opening of intact tight junctions, we have employed a transepithelial electrical resistance (TEER) breakdown assay using monolayers of the C7 subclone of Madin-Darby canine kidney (MDCK-C7) cells, which form tight junctions similar to those of BBB endothelial cells [16, 34]. In this functional assay, TEER breakdown indicates disrupted tight junction function.
Materials and methods
Cell culture
Primary cells from three glioblastomas (TB286, TB288, TB1338) (WHO grade IV), one fibrillary astrocytoma (WHO grade II) and one oligoastrocytoma (WHO grade II) were prepared from specimens of patients undergoing tumor resection at the University Hospital Münster. Neuroradiologically, glioblastomas exhibited heterogeneous contrast enhancement, whereas low-grade gliomas did not enhance. Histological diagnosis was performed according to the WHO classification [10] on both frozen sections (taken adjacent to the tissue used for experiments) and paraffin sections. Immediately after resection, tumor tissue was finely minced with two scalpels and incubated in cell culture medium (MEM containing 10% fetal calf serum, 100 U/ml penicillin and 100 µg/ml streptomycin) in a culture dish of 10 cm diameter (Nunc, Wiesbaden, Germany) at standard conditions (37°C, humidified air containing 5% CO2) for 48 h. Subsequently, the medium containing cell and tissue debris was aspirated and the plate was rinsed twice with phosphate-buffered saline (PBS). The remaining adherent cells were overlaid with medium and cultured under standard conditions. Cells of the first five passages were used for the experiments. The melanoma cell line A7, serving as a highly invasive control, and MDCK-C7 cells have been previously described [33, 34]. All cell culture reagents were purchased from Biochrom (Berlin, Germany).
TEER breakdown assay
A schematic model of the TEER breakdown assay is given in Fig. 1. MDCK-C7 cells were grown on filter membranes (growth area, 4.2 cm2; pore diameter, 0.4 µm; thickness, 20 µm; Falcon, Heidelberg, Germany). MDCK-C7 cells (106 cells) were seeded on the reverse side of an upside-down-oriented membrane filter cup. After 4 h, the supernatant was removed and the filter cup was placed in a six-well culture plate in the right orientation. Medium exchange and TEER measurement started 48 h after seeding MDCK-C7 cells. After another 4–20 days, tumor cells were added into the upper compartment of the filter cup, separated from MDCK-C7 cells by the filter membrane. The filter cup membrane had been tested for transmigration and found to be impermeable to MDCK-C7, melanoma and glioblastoma cells. For control experiments, MDCK-C7 but no tumor cells were seeded in the upper chamber. For experiments without tumor cells, lipopolysaccharide (LPS) from E. coli (0111:B4; lyophilized and sterilized by γ-irradiation; Sigma-Aldrich, St. Louis, MO) was applied in the upper compartment at final concentrations of 0.01, 1 or 100 µg/ml.
Schematic model of the TEER breakdown assay. MDCK-C7 cells (1) were grown on the reverse side of a polycarbonate filter cup (2) until they reached confluence. The filter cup was mounted in a 3-cm-diameter culture chamber (cavity of a six-well dish) (3) so that MDCK-C7 cells were located in the lower compartment. Tumor cells (4) were seeded in the upper compartment. Because of the 0.4-µm pore diameter of the filter, a direct cell-cell contact of glioma cells and MDCK-C7 cells was excluded. Resistance changes were measured using an ohmmeter (G) (TEER transepithelial electrical resistance)
For TEER measurements, published in detail previously[34], we used commercially available STX-2 chopstick electrodes (WPI, Sarasota, FL). Background electrical resistance built up by filter and medium only was constant and extremely low (25 Ω·cm2). MDCK-C7 cell monolayers were used after exhibiting a resistance of ≥8 kΩ·cm2. A resistance ≥1 kΩ·cm2 already implicates a tight MDCK-C7 monolayer. In contrast, the maximum transepithelial resistance of melanoma or glioma cells was 30 Ω·cm2, a value close to the background resistance of the filter membrane (25 Ω·cm2). TEER was measured at least once a day in six-well dishes. TEER values were corrected for background resistance. All experiments were performed in duplicate.
Results
Glioblastoma cells show electrical resistance breakdown similar to that of highly invasive melanoma cells
First, we tested the effect of glioblastoma primary cells (TB286) on the electrical resistance of the MDCK-C7 monolayer. Tumor cells (1×106) were seeded in the upper chamber of the filter membrane cup. Within 48 h glioblastoma cells led to a massive resistance breakdown, similar to findings obtained with A7 melanoma cells (Fig. 2a). An additional experiment using another glioblastoma primary culture (TB1338) resulted in similar effects (data not shown).
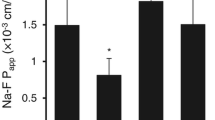
Course of TEER after adding glioma cells (a–c), MDCK-C7 cells (a–c) or LPS (d) into the upper compartment (indicated by arrow). MDCK-C7 cells (indicated by black dots) served as negative control (no TEER breakdown) and highly invasive A7 melanoma cells (indicated by black triangles) as positive control (marked TEER breakdown). a TB286 glioblastoma primary cells induced marked TEER breakdown, reaching the same low resistance as after application of A7 melanoma cells, although somewhat delayed; 1×106 cells were used in all experiments. b TB288 glioblastoma cells rapidly induced sudden TEER breakdown, whereas addition of low-grade (fibrillary) astrocytoma cells showed effects that were delayed by 24–72 h; 5×105 cells were used in all experiments. c TB288 glioblastoma cells showed massive TEER breakdown, whereas virtually no effect was seen with low-grade oligoastrocytoma cells; 3×105 cells were used in all experiments. d Addition of LPS to the upper compartment induced rapid, dose-dependent TEER breakdown. No effect was seen after application of solvent only
Effects of low-grade glioma cells on electrical resistance are weaker than those of glioblastoma cells
To study whether the grade of glioma malignancy affected resistance breakdown, we next compared glioblastoma (TB288) and fibrillary astrocytoma primary cells (Fig. 2b). Again, the addition of glioblastoma cells led to marked resistance breakdown. In contrast, resistance breakdown due to astrocytoma cells was delayed by 24–72 h, but the same low level resistance was eventually reached with all cells. In another experiment, we compared TB288 glioblastoma cells with oligoastrocytoma cells (Fig. 2c). As in the previous experiment, resistance breakdown by glioblastoma cells was massive and nearly complete, although somewhat delayed, presumably due to the lower number of cells applied. In contrast, the same number of oligoastrocytoma cells had virtually no effect.
MDCK-C7 monolayer resistance is sensitive to LPS
Since LPS is known to induce BBB permeability in vivo, we tested whether similar effects occur in our BBB model in vitro. We used the same experimental design as before, but added only LPS in different concentrations to the medium in the upper chamber. LPS dose-dependently induced resistance breakdown within 24 h (Fig. 2d).
Discussion
We used an in vitro TEER breakdown assay to measure the effects of high- and low-grade primary glioma cells on a tight test barrier that reproduces essential features of the BBB. We found marked TEER breakdown by glioblastoma cells, corresponding to data obtained with highly invasive melanoma cells, whereas no or delayed effects were observed with low-grade glioma cells. These data suggest that BBB breakdown in malignant gliomas in vivo is mediated, at least in part, by secretion of soluble substances by glioma cells, which inactivate endothelial tight junctions.
The TEER breakdown assay used here, which takes advantage of the extreme electrical tightness of MDCK-C7 epithelial cell monolayers, was first developed as a sensitive technique to investigate the invasive potential of melanoma and carcinoma cells [16, 34]. In these tumors, invasion is understood as the ability of tumor cells to penetrate epithelial barriers carrying tight junctions, which is a prerequisite to form metastases. In contrast, gliomas hardly ever systemically metastasize, while invasion here refers to diffuse tumor cell dissemination within the brain. Except for choroid plexus epithelial cells and highly specialized oligodendroglial structures, the only intracerebral cells carrying tight junctions are endothelial cells forming the BBB. Our assay, which measures tight junction leakiness, is therefore able to model and quantify not only carcinoma invasion, but also BBB breakdown. There is ample evidence indicating that tight junctions of MDCK cell monolayers and of cerebral endothelial cells are very similar (albeit not identical) from the structural, molecular and functional points of view. Thus, the ultrastructure of cerebral endothelial tight junctions is more similar to those of epithelial cells than to tight junctions of somatic endothelial cells [11]. Enzymatic composition and antigenic expression of MDCK cells resemble that of cerebral endothelial cells [30], although BBB tight junctions contain claudins-3, -5 and -12, while tight junctions of MDCK cells may contain claudins-1, -2 and -4 [7]. The validity of the MDCK-C7 assay has been further corroborated by our data showing that LPS, known to impair the BBB in vitro [4] and in vivo [19], dose-dependently induced TEER breakdown in MDCK-C7 cells. Moreover, the MCDK-C7 assay has the advantage of using a well-established cell line with stable tight junction morphology in vitro, whereas BBB models based on primary endothelial cells suffer from problems due to the loss of typical tight junctions in vitro [31]. Taken together, the MDCK-C7 assay appears to be a promising and valid model for analyzing the BBB in vitro.
The experimental setup, preventing tumor cells in the upper compartment from directly interacting with MDCK-C7 cells on the reverse side of the filter in the lower compartment, excludes mechanical forces exerted by tumor cells on the MDCK-C7 monolayer as well as gap junction-mediated interactions between the two cell types as basis of the observed effects. Rather, our findings suggest that soluble factors secreted by glioma cells have impaired tight junction function. The nature of these factors is unknown, but candidates include proteases, vascular endothelial growth factor (VEGF) and scatter factor/hepatocyte growth factor (SF/HGF). Specifically, a variety of proteases, including matrix metalloproteinase (MMP)-2 and MMP-9, plasminogen activators and cathepsin B may impair the BBB, and malignant gliomas express most of these proteases as well as MMP inducers such as CD147 at higher levels than low-grade gliomas [3, 15, 21, 27]. VEGF, which is produced at much higher levels by malignant gliomas than by low-grade gliomas, induces BBB opening and edema formation [17, 24]. Interestingly, there is a correlation between VEGF mRNA level, in vivo capillary permeability and vascular volume in gliomas [18]. Similarly, SF/HGF, which is up-regulated in glioma cells with increasing malignancy [12], increases endothelial cell permeability [9]. It remains to be determined whether these or other substances released by glioma cells actually affect tight junctions and BBB function of endothelial cells of the surrounding brain.
References
Abbott NJ (2002) Astrocyte-endothelial interactions and blood-brain barrier permeability. J Anat 200:629–638
Bertossi M, Virgintino D, Maiorano E, Occhiogrosso M, Roncali L (1997) Ultrastructural and morphometric investigation of human brain capillaries in normal and peritumoral tissues. Ultrastruct Pathol 21:41–49
Binder DK, Berger MS (2000) Proteases and the biology of glioma invasion. J Neurooncol 56:149–158
Descamps L, Coisne C, Dehouck B, Cecchelli R, Torpier G (2003) Protective effect of glial cells against lipopolysaccharide-mediated blood-brain barrier injury. Glia 42:46–58
Dinda AK, Sarkar C, Roy S, Kharbanda K, Mathur M, Khosla AK, Banerji AK (1993) A transmission and scanning electron microscopic study of tumoral and peritumoral microblood vessels in human gliomas. J Neurooncol 16:149–158
Engelhard HH, Groothuis DG (1999) The blood-brain barrier: structure, function, and response to neoplasia. In: Berger MD, Wilson CB (eds) Gliomas. Saunders, Philadelphia, pp 115–121
Furuse M, Furuse K, Sasaki H, Tsukita S (2001) Conversion of zonulae occludentes from tight to leaky strand type by introducing claudin-2 into Madin-Darby canine kidney cells. J Cell Biol 153:263–272
Janzer RC, Raff MC (1987) Astrocytes induce blood-brain barrier properties in endothelial cells. Nature 325:253–257
Jiang WG, Martin TA, Matsumoto K, Nakamura T, Mansel RE (1999) Hepatocyte growth factor/scatter factor decreases the expression of occludin and transendothelial resistance (TER) and increases paracellular permeability in human vascular endothelial cells. J Cell Physiol 181:319–329
Kleihues P, Cavenee WK (2000) World Health Organization classification of tumours. Pathology and genetics. Tumours of the nervous system. WHO, Lyon
Kniesel U, Wolburg H (2000) Tight junctions of the blood-brain barrier. Cell Mol Neurobiol 20:57–76
Lamszus K, Laterra J, Westphal M, Rosen EM (1999) Scatter factor/hepatocyte growth factor (SF/HGF) content and function in human gliomas. Int J Dev Neurosci 17:517–530
Lee SW, Kim WJ, Choi YK, Song HS, Son MJ, Gelman IH, Kim YJ, Kim KW (2003) SSeCKS regulates angiogenesis and tight junction formation in blood-brain barrier. Nat Med 9:900–906
Liebner S, Fischmann A, Rascher G, Duffner F, Grote EH, Kalbacher H, Wolburg H (2000) Claudin-1 and claudin-5 expression and tight junction morphology are altered in blood vessels of human glioblastoma multiforme. Acta Neuropathol 100:323–331
Lo EH, Wang X, Cuzner ML (2002) Extracellular proteolysis in brain injury and inflammation: role for plasminogen activators and matrix metalloproteinases. J Neurosci Res 69:1–9
Ludwig T, Ossig R, Graessel S, Wilhelmi M, Oberleithner H, Schneider SW (2002) The electrical resistance breakdown assay determines the role of proteinases in tumor cell invasion. Am J Physiol Renal Physiol 283:F319–F327
Machein MR, Plate KH (2000) VEGF in brain tumors. J Neurooncol 50:109–120
Machein MR, Kullmer J, Fiebich BL, Plate KH, Warnke PC (1999) Vascular endothelial growth factor expression, vascular volume, and capillary permeability in human brain tumors. Neurosurgery 44:732–740
Mun-Bryce S, Rosenberg GA (1998) Gelatinase B modulates selective opening of the blood-brain barrier during inflammation. Am J Physiol 274: R1203–R1211
Nitta T, Hata M, Gotoh S, Seo Y, Sasaki H, Hashimoto N, Furuse M, Tsukita S (2003) Size-selective loosening of the blood-brain barrier in claudin-5-deficient mice. J Cell Biol 161:653–660
Nuttall RK, Pennington CJ, Taplin J, Wheal A, Yong VW, Forsyth PA, Edwards DR (2003) Elevated membrane-type matrix metalloproteinases in gliomas revealed by profiling proteases and inhibitors in human cancer cells. Mol Cancer Res 1:333–345
Papadopoulos MC, Saadoun S, Davies DC, Bell BA (2001) Emerging molecular mechanisms of brain tumour oedema. Br J Neurosurg 15:101–108
Papadopoulos MC, Saadoun S, Woodrow CJ, Davies DC, Costa-Martins P, Moss RF, Krishna S, Bell BA (2001) Occludin expression in microvessels of neoplastic and non-neoplastic human brain. Neuropathol Appl Neurobiol 27:384–395
Pietsch T, Valter MM, Wolf HK, Deimling A von, Huang HJ, Cavenee WK, Wiestler OD (1997) Expression and distribution of vascular endothelial growth factor protein in human brain tumors. Acta Neuropathol 93:109–117
Roberts HC, Roberts TP, Brasch RC, Dillon WP (2000) Quantitative measurement of microvascular permeability in human brain tumors achieved using dynamic contrast-enhanced MR imaging: correlation with histologic grade. Am J Neuroradiol 21:891–899
Rubin LL, Staddon JM (1999) The cell biology of the blood-brain barrier. Annu Rev Neurosci 22:11–28
Sameshima T, Nabeshima K, Toole BP, Yokogami K, Okada Y, Goya T, Koono M, Wakisaka S (2000) Expression of emmprin (CD147), a cell surface inducer of matrix metalloproteinases, in normal human brain and gliomas. Int J Cancer 88:21–27
Sawada T, Kato Y, Kobayashi M, Takekekawa Y (2000) Immunohistochemical study of tight junction-related protein in neovasculature in astrocytic tumor. Brain Tumor Pathol 17:1–6
Seitz RJ, Wechsler W (1987) Immunohistochemical demonstration of serum proteins in human cerebral gliomas. Acta Neuropathol 73:145–152
Veronesi B (1996) Characterization of the MDCK cell line for screening neurotoxicants. Neurotoxicology 17:433–443
Wolburg H, Lippoldt A (2002) Tight junctions of the blood-brain barrier: development, composition, and regulation. Vascul Pharmacol 38:323–337
Wolburg H, Wolburg-Buchholz K, Kraus J, Rascher-Eggstein G, Liebner S, Hamm S, Duffner F, Grote EH, Risau W, Engelhardt B (2003) Localization of claudin-3 in tight junctions of the blood-brain barrier is selectively lost during experimental autoimmune encephalomyelitis and human glioblastoma multiforme. Acta Neuropathol 105:586–592
Wunsch S, Gekle M, Kersting U, Schuricht B, Oberleithner H (1995) Phenotypically and karyotypically distinct Madin-Darby canine kidney cell clones respond differently to alkaline stress. J Cell Physiol 164:164–171
Zak J, Schneider SW, Eue I, Ludwig T, Oberleithner H (2000) High-resistance MDCK-C7 monolayers used for measuring invasive potency of tumour cells. Pflugers Arch 440:179–183
Acknowledgement
This study was supported by grant Pa 328/5 from Deutsche Forschungsgemeinschaft.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schneider, S.W., Ludwig, T., Tatenhorst, L. et al. Glioblastoma cells release factors that disrupt blood-brain barrier features. Acta Neuropathol 107, 272–276 (2004). https://doi.org/10.1007/s00401-003-0810-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-003-0810-2