Abstract
We performed a neuropathological analysis, including in situ nick end labeling (ISEL) and immunohistochemistry, of two cases of clinicogenetically confirmed infantile spinal muscular atrophy (SMA) type II. Both cases showed severe reduction of the motor neurons and gliosis in the spinal cord and brain stem, although the occurrences of central chromatolysis and ballooned neurons were not frequent. Clark's and lateral thalamic nuclei, which are usually altered in SMA type I, were spared, whereas Betz cells in the precentral gyrus and large myelinated fibers in the lateral funiculus were reduced in number. Regarding apoptosis, only the younger case demonstrated a few ISEL-positive nuclei in the dorsal horn, with reduced Bcl-x expression level in the Purkinje cells. Unlike SMA type I, the expression of neurofilaments was not disturbed and the reduction in synaptophysin expression level in the anterior horn was mild. An oxidative stress-related product was deposited in atrophic motor neurons in the spinal cord, and neurons with nuclei immunoreactive for 8-hydroxy-2'-deoxyguanosine were found in the lateral thalamus. In contrast, the expression of glial glutamate transporters was not altered. These data suggest that oxidative stress and, to a lesser extent, apoptotic cell death, but not disturbed neurofilament metabolism or excitotoxicity, may be involved in neurodegeneration in SMA type II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infantile spinal muscular atrophy (SMA) is an autosomal recessively inherited disorder characterized by excessive degeneration of motor neurons of the spinal cord and brain stem, resulting in weakness and wasting of voluntary muscles. On the basis of age of onset and clinical course, SMA is classified into three types: type I (Werdnig-Hoffmann disease), type II (the intermediate form) and type III (Kugelberg-Welander disease) [3]. SMA type I is considered as the acute and most severe form characterized by early onset and hypotonia of voluntary muscles that is rapidly progressive terminating in fatal respiratory failure. SMA type II is a less severe form and SMA type III is the juvenile form. In addition to the major lesions in the motor neurons in the spinal cord and brain stem, SMA type I demonstrated involvement of the dorsal root ganglion, Clarke's column and lateral thalamic nucleus, especially in subjects with long survival periods [11, 21, 32]. On the other hand, there have been only a limited number of postmortem studies in SMA type III [1, 9, 13, 22, 34]. Most reports have described the degeneration of motor neurons in the anterior horn and/or nuclei of the cranial nerves and decreased myelinated fibers in the fasciculus gracilis. An exact neuropathological examination still remains to be carried out for SMA type II, because the number of patients with SMA type II is very small. On genetic analysis, several research groups detected deletions associated with SMA in chromosome 5q13, affecting different genes, including the survival motor neuron (SMN) gene [16] and neuron apoptosis inhibiting protein (NAIP) gene [24]. The SMN gene is present in humans in a telomeric copy, SMN1, and several centromeric copies, SMN2. Recently, several SMN-deficient mice models were created, and it was suggested that the absence of SMN1 was associated with SMA and SMN2 was a modifying gene in the disease severity of SMA [7]. In addition, although SMN itself has only a weak anti-apoptotic activity, co-expression of SMN with Bcl-2, another anti-apoptotic protein, confers a synergistic preventive effect against apoptosis [10]. For certain, apoptotic cell death occurs in the degenerated muscle fibers in the patients with SMA type I [30, 31]. In patients with SMA type I, apoptotic neuronal death was also detected in the spinal cord by TdT-mediated DIG-dUTP nick end labeling (ISEL) and electron microscopical analysis [27], although it was more frequently observed in the thalamus [5]. Furthermore, the apoptotic process that occurs in the anterior horn during the fetal period is enhanced in patients with SMA type I [28]. Besides apoptosis, it is speculated that oxidative stress and/or glutamate excitotoxicity may be involved in adult-onset motor neuron disorders, including amyotrophic lateral sclerosis (ALS) [2, 23], and these pathological mechanisms should be investigated in SMA and childhood-onset motor neuron disorders, but such trials have rarely been performed. On the other hand, SMA has different pathological characteristics from those in ALS, such as the frequent occurrence of ballooned neurons and the localization pattern of phosphorylated neurofilament and ubiquitin epitopes [12, 15, 18]. In the present study, we report two autopsy cases of clinicogenetically confirmed SMA type II. Immunohistochemical analysis, in addition to ISEL, was performed to clarify the pathological mechanisms in neurodegeneration in SMA.
Case report
Case 1
A female infant was born at term uneventfully to healthy and non-consanguineous parents. The family history was unremarkable. Her development was normal until 6 months of age, but after that there was a delay in her motor development and muscle hypotonia appeared in the lower extremities. At 15 months of age, she was brought to our hospital. Physical and neurological examinations revealed normal intelligence, muscle hypotonia and atrophy of the proximal parts of limbs, fasciculation of the tongue and limb muscles and reduced deep-tendon reflexes. Laboratory tests of serum enzymes disclosed no abnormalities. Electromyogram demonstrated that motor unit potentials were polyphasic and augmented in amplitude and duration. Her parents did not grant permission for muscle biopsy. A provisional diagnosis of SMA type II was made on the basis of clinical features and electromyography. She was able to sit unsupported but never became ambulant. She died of food poisoning at the age of 5 years.
Case 2
A female infant was born at term uneventfully. There was no history of consanguinity. She had two sisters and one brother. Her eldest sister was severely hypotonic at birth and died of pneumonia at 18 months of age, although the detailed course of her illness could not be ascertained. The other sister and brother did not suffer from any neuromuscular disorders. This case had normal development until 7 months of age, then muscle hypotonia occurred. She was able to sit unassisted and carry herself on her knees and her intelligence quotient was normal. Based on clinical and electrophysiological findings, a provisional diagnosis of SMA type II was made. Gradually muscle weakness developed and she became bedridden from the age of 13 years until her death. At the age of 17 years, she was referred to our hospital. The results of muscle biopsy performed at the age of 21 years demonstrated that the neurogenic changes were in accordance with SMA type II. Mild involuntary movements were sometimes observed in the face and upper limbs late in the disease course. Respiratory failure gradually developed, and she died of pneumonia at the age of 37 years.
Materials and methods
Quantitative multiplex PCR
The parents of both cases granted permission to perform genetic analyses in addition to autopsy. The competitive PCR based on the mismatch SMN primer described by Wirth et al. [35] was used to create different HinfI restriction sites in SMN1 and SMN2. The forward primer is mismatch primer designed based on the sequence of SMN1 exon 7 (SMN7F: 5´-CTTCCTTTTATTTTCCTTACAGGGATT-3´), and the reverse primer lay in intron 7 (SMN7R: 5´-TCCACAAACCATAAAGTTTTAC-3´). The uncut SMN-PCR products were 135-bp in length; SMN2-PCR products contained only one HinfI restriction site, resulting in 101- and 34-bp fragments, whereas SMN1-PCR products contained two HinfI restriction sites, resulting in three fragments of 78, 34 and 23 bp (Fig. 1A). The competitive PCR was performed according to method used in the previous study [35] with slight modifications. The PCR products were digested with 20 U DdeI (Boehringer Mannheim, Germany). Electrophoresis was carried out 2.5% agarose gels. The SMN2 exon 8 PCR products contained one DdeI restriction site, resulting in 123- and 65-bp fragments (Fig. 1B), whereas SMN1 exon 8 PCR products contained no restriction sites.
Demonstration of SMN gene deletions in SMA patients based on the presence or absence of specific PCR products by restriction site assay. Lane C DNA from control individual; lane 1 DNA from SMA case 1; lane 2 DNA from SMA case 2. A There are two PCR fragments (101 and 34 bp) derived from SMN2 exon 7 in SMA patients. The 123- and 65-bp fragments shown B in lanes 1 and 2 indicate the absence of SMN1 exon 8 products in patients with SMA
Neuropathology
The brain and spinal cord were fixed in a 10% buffered formalin solution. The formalin-fixed nervous tissues were cut coronally, embedded in paraffin and then subjected to hematoxylin and eosin (HE), Klüver-Barrera (KB), Bodian and Holzer stainings. We then performed a morphometric analysis of the density of large myelinated fibers in the lateral funiculus of the spinal cord. We used Bodian-stained sections from both SMA type II cases and the age-dependent disease controls, a 6-year-old male with a sequel of kernicterus and a 35-year-old male with Becker-type muscular dystrophy, who did not show any morphological changes in the spinal cord. The count of the large myelinated fibers was performed following manual labeling of appropriate fibers in ten non-overlapping microscopic subfields at a magnification of ×200 (area, 1 mm2 each) in the lateral funiculus of the cervical and thoracic segments of the spinal cord.
In situ nick end labeling
Double staining with ISEL and anti-synaptophysin immunohistochemistry was performed on the sections of the middle medulla oblongata, cervical, thoracic and lumbar segments of the spinal cord. The sections were stripped of proteins by incubation with 0.1% trypsin (Sigma, MO) at 37°C for 30 min. After rinsing, the sections were incubated in TdT buffer (30 mM Trizma base, pH 7.2, 140 mM sodium cacodylate, 1 mM cobalt chloride) containing TdT (0.3 U/µl) (Life Technologies, Md) and digoxigenin-dUTP (Roche Diagnostics, Mannheim, Germany) at 37°C for 60 min. The reaction was terminated in TB buffer (300 mM sodium chloride, 30 mM sodium citrate) at room temperature for 15 min. After rinsing, the sections were treated with a 1:500 dilution of alkaline phosphatase-labeled anti-digoxigenin antibodies (Roche Diagnostics) at room temperature for 1 h. The reaction was visualized by 4-nitroblue-tetrazolium-chloride/5-bromine-4-chloride-3-indolylphosphate (Sigma). After ISEL, the sections were treated with rabbit polyclonal antibody to synaptophysin (1:50, Dako, Glostrup, Denmark) at 4°C overnight and the immune reaction was visualized with an ABC/AEC staining kit (Dako).
Immunohistochemistry
Immunohistochemistry was performed on serial paraffin sections of the precentral cortex, the temporal cortex including the hippocampus, the striatum and thalamus, the cerebellum including the dentate nucleus, the middle medulla oblongata, and the cervical, thoracic and lumbar segments of the spinal cord in both the cases of SMA type II and the aforementioned disease controls. Each section was cut 6 µm thick, deparaffinized, and heated by microwaving in a citrate solution for 20 min. Endogenous peroxidase activity in the sections was quenched with 1% hydrogen peroxide. Mouse monoclonal and/or rabbit polyclonal antibodies to the following substances were employed at each optimal concentration: Bcl-2 (1:80), Bcl-x (1:500) (Santa Cruz Biotechnology), phosphorylated neurofilament (1:50), ubiquitin (1:400) (DAKO), nitrotyrosine (1:500) (Upstate Biotechnology, Lake Placid, NY), advanced glycation end product (AGE, 1:1,000), 4-hydroxy-2-nonenal-modified protein (4HNE, 1:1,000), 8-hydroxy-2'-deoxyguanosine (8-OHdG, 1:1,000), glutamate transporters including GLAST (1:300), GLT-1 (1:300) and EAAC1 (1:300) (Wako Pure Chemical Industries, Osaka, Japan). The immune reaction was visualized by the avidin-biotin-immunoperoxidase complex method following the manufacturer's protocol (Nichirei, Tokyo, Japan).
Results
DNA analyses
DNA analyses by the PCR method using the frozen tissues of the autopsied livers and the paraffin-embedded nervous tissues from the autopsied brain were performed in cases 1 and 2, respectively. In both cases, the deletions of exons 7 and 8 in the SMN gene were detected (Fig. 1), while those of exons 5 and 6 in the NAIP gene were not detected. Accordingly, the diagnosis of SMA type II was genetically confirmed in both cases.
Neuropathological findings
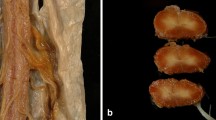
The brains weighed 1,260 g and 1,125 g in cases 1 and 2 at autopsy, respectively. Both cases presented similar pathological findings. The major changes existed in the spinal cord, including severe reduction in the number of the motor neurons, frequent formations of empty cell beds and gliosis in the anterior horn (Fig. 2A). Nevertheless, the motor neurons in the anteromedial zone at the third, fourth and fifth cervical segments of the spinal cord, the phrenic motor neurons, were comparatively preserved (data not shown). The remaining motor neurons showed atrophic changes but not central chromatolysis or ballooning. Similar changes were noted in the hypoglossal nucleus in both cases (Fig. 2B) and in the facial nucleus only in case 2. In addition, the numbers of large myelinated fibers in the spinal pyramidal tract of the lateral funiculus were reduced slightly in case 1 and significantly in case 2 when compared with the age-matched disease controls (Fig. 2C, D and Table 1). However, there was no fibrillary gliosis in the lateral funiculus. Case 2 also showed mild loss of myelinated fibers with gliosis in the fasciculus gracilis (Fig. 2E). The ventral root demonstrated atrophic changes and loss of the large myelinated fibers in both cases, whereas the dorsal root ganglia were comparatively preserved in both cases. Furthermore, glial bundles were abundantly observed in the proximal portions of the ventral roots and occasionally in the dorsal roots of the cervical and lumbosacral segments in case 1 (Fig. 2F), while they were observed only in the thoracic segment in case 2. There were a few heterotopic neurons in the anterior funiculus in the lumbosacral segment of the spinal cord in case 1. Clarke's and Onuf's nuclei were spared. In the cerebrum, Betz cells in the precentral gyrus of the frontal lobe exhibited a decrease in number in both cases compared with the age-matched controls (data not shown), but there was no gliosis. The hippocampus, basal ganglia, thalamus, hypothalamus and cerebellum exhibited no neuronal loss, gliosis, chromatolytic changes, ballooned neurons or neuronophagia.
Histochemical features. A The anterior horn shows frequent formations of empty cell beds at the cervical segment of the spinal cord in case 1. B The hypoglossal nucleus demonstrates neuronal loss and/or atrophy in case 2. C, D Compared with the age-matched disease control (C), the large myelinated fibers in the lateral funiculus of the spinal cord are reduced in number in case 2 (D). E Case 2 shows moderate loss of the myelinated fibers in the fasciculus gracilis. F In case 1, glial bundles are present in the dorsal root ganglia. A, B, E, F Klüver-Barrera staining; C, D Bodian staioning. A–D, F ×200; E ×40
In situ nick end labeling
Neither of the disease controls demonstrated ISEL-positive nuclei in any brain regions examined. In the spinal cord, a few ISEL-positive nuclei were observed in the atrophic neurons, surrounded with synaptophysin-immunoreactive granules in the dorsal horn of the lower lumbar and/or sacral segments only in case 1 (Fig. 3A). On the other hand, there were no ISEL-positive nuclei in the brain stem including the hypoglossal and facial nuclei, cerebellum, basal ganglia, thalamus and cerebral cortex, although ISEL-positive neurons were frequently observed in the lateral thalamus in cases of SMA type I [5].
. Immunohistological features. A ISEL-positive nuclei are found in the dorsal horn of the spinal cord in case 1 (arrows). B Immunoreactivity for synaptophysin in the cell surface of the remaining motor neurons is preserved in case 1. C, D Although the Purkinje cells in the cerebellar cortex constitutively express Bcl-x in a 6-year-old male with a sequel of kernicterus (C), Bcl-x expression level is severely reduced in case 1 (D). A 35-year-old male with Becker type muscular dystrophy does not reveal any deposition of oxidative stress-related products (E), whereas 4HNE deposition is observed in the cytoplasm in the atrophic motor neurons in the spinal cord in case 2 (F). G The nuclei of neurons in the lateral thalamus are immunoreactive for 8-OHdG in case 2 (arrows). H The expression of glial glutamate transporters GLT-1 is comparatively preserved in the anterior horn in the cervical segment of the spinal cord in case 2 (ISEL in situ nick end labeling, 4HNE 4-hydroxy-2-nonenal-modified protein, 8-OHdG 8-hydroxy-2'-deoxyguanosine). A, C–G ×200; B ×400; H ×40
Immunohistochemical findings
No abnormal structures were identified by immunostaining against either the phosphorylated neurofilament or ubiquitin epitope. On the other hand, synaptophysin immunoreactivity was slightly reduced in the anterior horn, as observed previouosly in cases of SMA type I [8]. However, the staining intensity of the cell surface in the remaining motor neurons was preserved (Fig. 3B), although it was reported to be augmented in cases of SMA type I [8]. Only case 1 exhibited a slight change in the expression level of cell death proteins. Some neurons were stained by anti-Bcl-2 immunostaining in the dorsal horn and intermediolateral portion of the spinal cord (data not shown). The Purkinje cells constitutively expressed Bcl-x in the disease controls (Fig. 3C) [14], although the Bcl-x immunoreactivity slightly decreased in the cerebellar cortex in case 1 (Fig. 3D). Neither of the disease controls showed deposition of oxidative stress-related products (oxidative products) or nuclei immunoreactivity for 8-OHdG in the brain areas examined (Fig. 3E). An abnormal deposition of 4HNE but not nitrotyrosine or AGE was detected in the cytoplasm of atrophic motor neurons in the spinal cord in both cases (Fig. 3F). Additionally, in case 2, neurons exhibiting nuclei immunoreactivity for 8-OHdG were noted in the lateral thalamus (Fig. 3G) and cerebellar granular layer. The expression of both neuronal (EAAC1) and glial (GLAST, GLT-1) glutamate transporters was comparatively preserved (Fig. 3H).
Discussion
To our knowledge, this is the first autopsy report of SMA type II, in which the diagnosis was confirmed clinically and genetically. Previously, only a brief note has described the devastation of the anterior horn cells in a 12-year-old girl in whom the disease was diagnosed at the age of 6 months [4]. However, genetic confirmation is a prerequisite for the diagnosis of SMA type II, since sibling cases of SMA type II without deletions of either SMN or NAIP have been reported [19]. Accordingly, there have been no detailed neuropathological studies on SMA type II. Although the molecular basis of the different clinical phenotypes remains unclear, a common genetic defect in SMA may account for a specific mechanism leading to the denervation process [29]. This denervation process may start early in utero in both SMA types I and II, while it also occurs after birth SMA type III, leading to a different clinical course in affected patients [3]. SMA type II has a more benign course than SMA type I, as observed in our cases, and reinnervation of atrophic muscle by surviving neurons may occur. Despite the clinical differences, our cases of SMA type II shared the major pathological findings in the central nervous system found in SMA type I and/or III. The motor neurons in the brain stem and spinal cord with the ventral and dorsal roots were affected, in addition to the comparative preservation of phrenic motor neurons and Onuf's nucleus. However, neither of our cases showed neuronal changes in the Clark's column and lateral thalamus, which are commonly observed in SMA type I [11, 26, 32]. They rather demonstrated changes in the upper motor neurons consisting of reduction in the number of both the Betz cells in the precentral gyrus and large myelinated fibers in the spinopyramidal tract. Demyelination in the lateral column in SMA type III has been rarely reported [22], but the absence of gliosis in our cases may suggest maldevelopment or anomalous changes rather than degeneration or demyelination. The changes in the upper motor neurons may be one of neuropathological cues to differentiate SMA type II from SMA types I and III, although the exact mechanisms underlying their differences in disease course remain to be clarified. On the other hand, the posterior column change observed in older case has usually been addressed in SMA type III [9, 22, 34]. It should be noted that the occurrence of motor neurons with central chromatolysis and ballooned neurons was rare in SMA type II. In SMA type I, ballooned neurons were frequently observed in the anterior horn, Clark's nucleus, dorsal root ganglion and thalamus, in which antibodies against phosphorylated neurofilament and ubiquitin epitopes preferentially stained the peripheral perikarya with proximal neurites and the center of the ballooned neurons, respectively [12, 15, 18]. Moreover, it has been proposed that the disturbed neurofilament metabolism may induce neuronal degeneration [18]. It is also speculated that the reduced immunoreactivity for synaptophysin around the ballooned neurons may indicate the disconnection of presynaptic terminals of afferent fibers from the degenerated motor neurons [8]. In contrast, inasmuch as ballooned neurons and pathological epitopes of phosphorylated neurofilament and ubiquitin epitopes were rarely identified in either of our cases of SMA type II, the neurofilament metabolism seemed to be spared, unlike in SMA type I. Similarly, in immunohistochemistry for synaptophysin, both our cases of SMA type II demonstrated staining profiles that differed from those of SMA type I [8]. The reduction in immunoreactivity in the anterior horn was mild, and the staining intensity of the cell surface in the remaining motor neurons was not augmented in SMA type II. Hence, the decrease of presynaptic terminals in the anterior horn was not severe. The differences in disease severity and/or other factors such as the functional effects of the number of copies of SMN2, the NAIP gene deletion and other unknown factors between SMA type I and type II may contribute to the discrepancy in the occurrence of ballooned neurons and the expression levels of neurofilament and synaptophysin between the two types of SMA.
The natural apoptotic neuronal process that occurs in the anterior horn during fetal period is enhanced in SMA type I [28], and the spinal motor neurons in SMA type I were observed to die by apoptosis, in addition to a mild reduction in the cytoplasmic Bcl-2 expression level [27], although the number of apoptotic motor neurons itself was relatively low [5, 27]. Consequently, the interrelationships between motor neuron death and apoptosis remains to be investigated in SMA. In this study, only the younger case showed ISEL-positive nuclei in the dorsal horn and slightly altered expression of anti-apoptotic Bcl-x expression in the cerebellar cortex. Since the postnatal expression level of Bcl-2 in the central nervous system declines with aging, and is retained in the granule cells in the cerebellar cortex and hippocampal dentate gyrus in adult subjects [17], it is difficult to evaluate the level of Bcl-2 expression in the spinal motor neurons in our cases aged over 5 years unlike infantile cases of SMA type I [27]. Although apoptotic cell death may be involved in neurodegeneration in SMA type II, the number of apoptotic neurons pathologically confirmed is low and the change in the expression level of cell death proteins is minimum. Besides apoptosis, oxidative stress and disturbed glutamate transport have been demonstrated to be involved in ALS [2, 23]. Increased nitrotyrosine due to excessive nitration of tyrosine by peroxynitrite has been observed in the spinal cord in ALS [2]. Glutamate transport is critical for preventing glutamate excitotoxicity, and disturbed glutamate transport has been proposed to be the cause of the motor neuron degeneration in ALS [23]. Previously, we performed the immunohistological examinations of the deposition of oxidative products and the expressions of glutamate transporters in SMA type I [6]. We demonstrated deposition of 4HNE but not of nitrotyrosine or AGE in the motor neurons and 8-OHdG-immunoreactive nuclei in the thalamus, cerebellar cortex and precentral cortex. Similarly, in SMA type II, both our cases demonstrated 4HNE deposition, and, in addition, case 2 had 8-OHdG-immunoreactive nuclei in the thalamus and cerebellar cortex. 4HNE is a reactive lipid aldehyde that is produced by membrane oxidation, and its level is increased in other neurodegenerative disorders such as Alzheimer's and Parkinson's diseases [25, 36]. It is likely that reactive lipid aldehyde may induce motor neuron degeneration in SMA types I and II. Oxidative damage to DNA can induce 8-OHdG and its abnormal deposition has also been reported in adult neurodegenerative disorders [20, 33]. In SMA, nuclei immunoreactive for 8-OHdG were present in the lateral thalamus and cerebellar cortex, while peroxidation of DNA did not seem to be predominant in the motor neuron devastation. Our previous study on apoptosis in SMA type I clarified DNA fragmentation in neurons of the lateral thalamus [5]. The lateral thalamic nuclei are usually affected in SMA type I cases, particularly with long survival on an artificial respirator [26]. Therefore, DNA fragmentation and oxidized nucleosides in the lateral thalamus may suggest latent thalamic degeneration, although routine histochemistry failed to identify neuronal loss and gliosis in the thalamus. On the other hand, the disturbed glutamate transport or glutamate excitotoxicity could not be verified in SMA type II, because the expressions of glial and neuronal glutamate transporters were comparatively preserved in both our cases. In contrast, three out of five cases of SMA type I showed reduced expression level of GLAST in the lateral thalamus in our previous study [6]. Although the detailed background for the difference in the thalamic expression level of GLAST between SMA types I an II remains to be investigated, it is probable that the latent thalamic degeneration may be more prominent in SMA type I, because ISEL-immunoreactive nuclei were identified in the lateral thalamus in SMA type I [5] but not in type II in this study.
In conclusion, the neuropathological features of SMA type II contained changes both similar to and different from those noted in SMA types I and III, and it is possible that oxidative stress and, to a lesser extent, apoptotic cell death, but not disturbed neurofilament metabolism or excitotoxicity, may be involved in neurodegeneration in SMA type II.
References
Aberfeld DC, Namba T (1969) Progressive opthalmoplegia in Kugelberg-Welander disease. Arch Neurol 20:253–256
Beal MF, Ferrante RJ, Browne SE, Matthews RT, Kowall NW, Brown RH Jr (1997) Increased 3-nitrotyrosine in both sporadic and familial amyotrophic lateral sclerosis. Ann Neurol 42:644–654
Dubowitz V (1995) Disorders of the lower motor neurone. The spinal muscular atrophy. In: Dubowitz V (ed) Muscle disorders in childhood, 2nd edn. Saunders, London, pp 325–369
Gardner-Medwin D, Hudgson P, Walton JN (1967) Benign spinal muscular atrophy arising in childhood and adolescence. J Neurol Sci 5:121–158
Hayashi M, Arai N, Murakami T, Morimatsu Y, Oda M, Matsuyama H (1998) A study of cell death in Werdnig-Hoffmann disease brain. Neurosci Lett 243:117–120
Hayashi M, Araki S, Arai N, Kumada S, Itoh M, Tamagawa K, Oda M, Morimatsu Y (2002) Oxidative stress and disturbed glutamate transport in spinal muscular atrophy. Brain Dev 24:770–775
Hsieh-Li HM, Chang JG, Jong YJ, Wu MH, Wang NM, Tsai CH, Li H (2000) A mouse model for spinal muscular atrophy. Nat Genet 24:66–70
Ikemoto A, Hirano A, Matsumoto S, Akiguchi I, Kimura J (1996) Synaptophysin expression in the anterior horn of Werdnig-Hoffmann disease. J Neurol Sci 136:94–100
Ikuta F, Ohama E, Nakanishi T, Mannen T, Toyokura Y (1979) Postmortem findings in a case of KW disease; presence of underdeveloped Schwann cells and axons. In: Japan Medical Research Foundation (ed) Amyotrophic lateral sclerosis. University of Tokyo Press, Tokyo, pp 277–284
Iwahashi h, Eguchi Y, Yasuhara N, Hanafusa T, Matsuzawa Y, Tsujimoto Y (1997) Synergistic anti-apoptotic activity between Bcl-2 and SMN implicated in spinal muscular atrophy. Nature 390:413–417
Iwata M, Hirano A (1978) A neuropathological study of the Werdnig-Hoffmann disease. Neurol Med Chir 8:40–53
Kato S, Hirano A (1990) Ubiquitin and phosphorylated neurofilament epitopes in ballooned neurons of the extraocular muscle nuclei in a case of Werdnig-Hoffmann disease. Acta Neuropathol 80:334–337
Kohn R (1968) Postmortem findings in a case of Wohlfart-Kugelberg-Welander disease. Confin Neurol 30:253–260
Kumada S, Hayashi M, Mizuguchi M, Nakano I, Morimatsu Y, Oda M (2000) Cerebellar degeneration in hereditary dentatorubral-pallidoluysian atrophy and Machado-Joseph disease. Acta Neuropathol 99:48–54
Lee S, Park YD, Yen SHC, Ksiezak-Redling H, Goldman JE, Dickson DW (1988) A study of infantile motor neuron disease with neurofilament and ubiquitin immunocytochemistry. Neuropediatrics 20:107–111
Lefebvre S, Burglen L, Revoullet S, Clermont O, Burlet P, Viollet L, Benichou B, Cruaud C, Millasseau P, Zeviani M, Paslier DL, Frezal J, Cohen D, Weissenbach J, Munnich A, Melki J (1995) Identification and characterization of a spinal muscular atrophy-determining gene. Cell 80:155–165
Merry DE, Veis DJ, Hickey WF, Korsmeyer SJ (1994) Bcl-2 protein expression is widespread in the developing nervous system and retained in the adult PNS. Development 120:301–311
Murayama S, Bouldin TW, Suzuki K (1991) Immunocytochemical and ultrastructural studies of Werdnig-Hoffmann disease. Acta Neuropathol 81:408–417
Nevo Y, Kramer U, Legum C, Shomrat R, Fatal A, Soffer D, Harel S, Shapira Y (1998) SMA type II unrelated to chromosome 5q13. Am J Med Genet 75:193–195
Nunomura A, Perry G, Alive G, Hirai K, Takeda A, Balraj EK, Jones PK, Ghanbari H, Wataya T, Shimohama S, Chiba S, Atwood CS, Petersen RB, Smith MA (2001) Oxidative damage is the earliest event in Alzheimer disease. J Neuropathol Exp Neurol 60:759–767
Osawa M, Shishikura K (1991) Werdnig-Hoffmann disease and variants. Handb Clin Neurol 15:51–80
Paulson GW, Liss L, Sweeney PJ (1980) Late onset spinal muscle atrophy—a sex linked variant of Kugelberg-Welander. Acta Neurol Scand 61:49–55
Rothstein JD, Kammen M van, Levey AI, Martin LJ, Kuncl RW (1995) Selective loss of glial glutamate transporter GLT-1 in amyotrophic lateral sclerosis. Ann Neurol 38:73–84
Roy N, Mahadevan MS, McLean M, Shutler G, Yaraghi Z, Farahani R, Baird S, Besner-Johnston A, Lefebvre C, Kang X, Salih M, Aubry H, Tamai K, Guan X, Ioannou P, Crawford TO, Joung PJ de, Surh L, Ikeda J, Korneluk RG, MacKenzie A (1995) The gene for neuronal apoptosis inhibitory protein is partially deleted in individuals with spinal muscular atrophy. Cell 80:167–178
Sayre LM, Zalasko DA, Harris PLR, Perry G, Salomon RG, Smith MA (1997) 4-Hydroxynonenal-derived advanced lipid peroxidation end products are increased in Alzheimer's disease. J Neurochem 68:2092–2097
Shishikura K, Hara M, Sasaki Y, Misugi K (1983) A neuropathological study of Werdnig-Hoffmann disease with special reference to the thalamus and posterior roots. Acta Neuropathol (Berl) 60:99–106
Simic G, Seso-Simic D, Lucassen PJ, Islam A, Krsnik Z, Cviko A, Jelasic D, Barisic N, Winbland B, Kostovic I, Kruslin B (2000) Ultrastructural analysis and TUNEL demonstrate motor neuron apoptosis in Werdnig-Hoffmann disease. J Neuropathol Exp Neurol 59:398–407
Soler-Botija C, Ferrer I, Gich I, Baiget M, Tizzano EF (2002) Neuronal death is enhanced and begins during foetal development in type I spinal muscular atrophy spinal cord. Brain 125:1624–1634
Soubrouillard C, Pellissier JF, Lepidi H, Mancini J, Rougon G, Figarella-Branger D (1995) Expression of developmentally regulated cytoskeleton and cell surface proteins in childhood spinal muscular atrophy. J Neurol Sci 133:155–163
Tews DS, Goebel HH (1996) DNA fragmentation and bcl-2 expression in infantile spinal muscular atrophy. Neuromuscl Disord 6:265-273
Tews DS, Goebel HH (1997) Apoptosis-related proteins in skeletal muscle fibers of spinal muscular atrophy. J Neuropathol Exp Neurol 56:150–156
Towfighi J, Young RSK, Ward RM (1985) Is Werdnig-Hoffmann disease a pure lower motor neuron disorder? Acta Neuropathol (Berl) 65:270–280
Toyokuni S (1999) Reactive oxygen species-induced molecular damage and its application in pathology. Pathol Int 49:91–102
Winder TR, Auer RN (1989) Sensory neuron degeneration in familial Kugelberg-Welander disease. Can J Neurol Sci 16:67–70
Wirth B, Herz M, Wetter A, Moskau S, Hahnen E, Rudnik-Schoneborn S, Wienker T, Zerres K (1999) Quantitative analysis of survival motor neuron copies: identification of subtle SMN1 mutations in patients with spinal muscular atrophy, genotype-phenotype correlation, and implication for genetic counseling. Am J Hum Genet 64:1340–1356
Yoritaka A, Hattori N, Uchida K, Tanaka M, Stadtman ER, Mizuno Y (1996) Immunohistochemical detection of 4-hydroxynonenal protein adducts in Parkinson disease. Proc Natl Acad Sci USA 93:2696–2701
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Araki, S., Hayashi, M., Tamagawa, K. et al. Neuropathological analysis in spinal muscular atrophy type II. Acta Neuropathol 106, 441–448 (2003). https://doi.org/10.1007/s00401-003-0743-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-003-0743-9