Abstract
Ependymomas are glial tumors of the brain and spinal cord. Genetic aberrations associated with the development of these tumors have not been fully identified yet. In previous cytogenetic and comparative genomic hybridization studies, multiple genomic imbalances in ependymomas were found, including partial or whole chromosome losses (1p, 4q, 6q, 9, 10, 11, 13, 16, 17, 19q, 20q and 22q). The aim of this study was to map particularly the commonly affected regions in ependymomas. Thirty-three pairs of matched normal and tumor specimens from ependymoma patients were genotyped using 34 polymorphic microsatellite markers distributed over 15 chromosomes. Loss of heterozygosity (LOH) was found in 26 of 33 tumors (78.8%). The most frequent LOHs were found on the long arms of chromosomes 6 (30.3%) and 9 (27.3%). LOH was also detected on 3p14 (13.3%), 10q23 (10.3%) and 11q (18.2%). Because of the high percentage of LOH on chromosome 6 and 9, we conclude that important tumor suppressor genes are situated on these two chromosomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ependymomas occur predominantly in children and adolescents, comprise approximately 9% of childhood brain tumors, and represent the third most frequent kind of brain tumors in children. Similar to other malignant gliomas, anaplastic ependymomas (WHO grade III) differ from ependymomas (WHO grade II) by the presence of high mitotic activity, cellular pleomorphism, and nuclear anaplasia. However, even when present, anaplasia does not appear to be consistently associated with poor prognosis [29]. Age at diagnosis, extent of resection, tumor location, and proliferation indices seem to be significant prognostic factors in this disease. Moreover, spinal ependymomas are associated with a more favorable prognosis than intracranial ependymomas of the respective WHO grade [21]. Adult ependymoma patients usually have a better prognosis than children with histologically comparable tumors [19].
Little is known regarding molecular genetic alterations underlying the formation and progression of ependymomas. Cytogenetic and molecular genetic studies have revealed structural and numerical abnormalities of chromosomes 6, 7, 9, 10, 11, 13, 17, and 22 [2, 7]. In comparative genomic hybridization (CGH) studies, these tumors showed mostly complex aberration patterns with frequent deletions or gains of chromosomes. The main losses occurred on chromosomes 1p, 4q, 6q, 9, 10, 13q, 16, 17, 19q, 20q and 22q [10, 24, 28, 36, 38]. This method, however, allows the detection of genetic aberration over the genome only at a resolution of 10–20 Mbp. Previous LOH studies in ependymomas have been restricted by the small number of cases studied; only a limited number of microsatellite markers and genes were investigated at one time [6, 16, 17]. Recently, an LOH study in ependymomas with 384 microsatellite markers was published [35]. However, the investigators focused on ependymomas WHO grade II and did not examine either the relationships between various genetic abnormalities detected or the relationships between genetic abnormalities and clinical features. Our group has recently identified two common regions showing deletions on the long arm of chromosome 22 in 33 ependymomas of brain and spinal cord using microsatellite markers [11]. In the present study, we have conducted allelotyping of 33 ependymomas using 34 microsatellite markers distributed over 15 autosomes to detect possible aberrations characterizing distinct clinicopathological subgroups.
Materials and methods
Tumor samples and DNA extraction
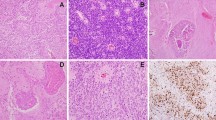
Tumor specimens (n=30) were obtained from patients treated at the Department of Neurosurgery, University Hospital of Würzburg (Würzburg, Germany) between 1992 and 2001 and 3 cases from the University Hospital of Münster (Münster, Germany). Histological diagnoses were established according to the WHO classification criteria [37]. Twenty-five cases were primary preoperatively untreated tumors; 8 tumors were recurrent. The series consisted of 5 myxopapillary ependymomas WHO grade I, 11 ependymomas WHO grade II, and 17 anaplastic ependymomas WHO grade III. 20 of the ependymomas were intracranial tumors; 13 were spinal cord lesions; 15 female and 18 male patients were included (Table 1). The mean patient age at diagnosis was 19 years (range 8 months to 69 years). For DNA extraction, only areas of the solid tumor specimens were analyzed; some cases required microdissection. DNA was prepared as described previously [11].
PCR and microsatellite analysis
We used a panel of 34 microsatellite repeats spread over 15 chromosomes for the analysis (Table 2). The repeats were chosen to cover loci of known and putative oncogenes or tumor suppressor genes and regions showing frequent aberrations detected in the previous CGH studies [10, 24, 28, 38]. Primer sequences for PCR amplification were retrieved from the Genome Database (http://gdbwww.gdb.org/). PCR primers were synthesized at MWG Biotech (Munich, Germany) and one oligonucleotide of each primer pair labeled with fluorescent dye phosphoramidites FAM, NED or HEX. Paired constitutional DNAs from peripheral blood leukocytes and tumor DNA samples of each patient were amplified with AmpliTaq Gold enzyme (ABI, Foster City, CA) in multiplex PCR reactions using 50 ng genomic DNA as template. Thirty cycles were carried out in a Mastercycler thermal cycler (Eppendorf, Hamburg, Germany). Aliquots of the PCR reactions were then mixed with ROX-labeled size standard and formamide, denatured, and subjected to electrophoresis on a 377 DNA Sequencer (ABI). The automatically collected data were analyzed by GENESCAN and GENOTYPER software as described in the manufacturer's manual. LOH and amplification were scored as described previously [11]. In summary, the unchanged allele was identified, and the ratios of the allele showing decreased or increased signal relative to the unchanged allele were calculated, first for control DNA, and then for the tumor. Decrease of the ratio by 40% in the tumor compared with the control was called LOH, increase by 40% amplification.
Statistical methods
Correlation between LOH results and clinicopathological variables (age, gender, tumor location, grade of differentiation) was evaluated by chi-square test. Associations between 6q LOH and LOH on chromosome 9 were also analyzed.
Results
LOH analysis
Representative examples of electropherograms are shown in Fig. 1. LOH with any of the 34 markers was observed in 26 of 33 tumors (78.8%). Out of 878 informative loci, 85 genotypes (9.7%) showed LOH. LOH frequency for individual chromosomal arms varied from 3.7% (20q13.1) to 26.7% (6q24-25.3). Amplifications were found in only 3 tumors (case 3 in 13q14, case 5 in 9q32-33 and case 24 in 20q13.1); microsatellite instability was found in one case. The frequency of genetic aberrations in specific regions is depicted in Fig. 2: 6q24-25.3 (26.7%), 6q15-16 (23.8%), 9p21 (22.6%), 6q24 (21.4%), 6q21-22.1 (19.2%), 11q23-24 (14.3%), 3p14.2 (13.3%), 11q13.1 (12.5%), 10q23 (10.3%), 13q14 (9.7%), 9q34 (9.4%), and 17p13.1 (9.3%). The long arm of chromosome 6 displayed the most frequent aberrations, 10 of 33 cases (30.3%) showing LOHs in two hot spots: 6q24-25.3 and 6q15-16 (Table 2 and Figs. 2, 3) as detected by markers D6S441 and D6S1709 in 8 (26.7% of informative cases) and 5 (23.8% of informative cases) tumors, respectively. The second most frequently altered chromosome was chromosome 9 displaying aberrations in 9 tumors (27.3% of informative cases) involving both its long and short arms (Fig. 3).
Representative LOH in the 11q23-24 region as detected with the D11S2179 microsatellite marker in patient 11. Control and tumor samples were amplified in a multiplex reaction with markers D11S2179 located in the 11q23-24 region and D15S231 used as internal control. Arrows indicate LOH (LOH loss of heterozygosity)
Clinicopathological correlations
Intracranial tumors were found more frequently in children (mean age 10.6 years) than in adult patients (mean age 31.8 years) who had more intraspinal tumors (P<0.01, χ2 test). While the vast majority (84%) of intraspinal ependymomas were histologically benign, corresponding to WHO grade II or I, most of the intracranial tumors (75%) were classified as anaplastic, WHO grade III (P<0.01, χ2 test, Table 1). The differences in tumor grade and location were also reflected in the differences in patient survival. Three patients had died by the time of this study, all of these cases were children with intracranial anaplastic ependymomas.
LOH on chromosome 9 was frequently associated with male patients (8 male versus 1 female patients, P=0.02, χ2 test). Five anaplastic ependymomas with LOH on chromosome 9 were intracranial: four of them with loss of 9p were infratentorial and one with loss of 9q was supratentorial (Table 1). While the numbers in each group were small, there was no significant difference in the incidence of LOH between the intracranial and spinal ependymomas or between infratentorial and the supratentorial ependymomas. There was no correlation between allelic loss and a specific tumor grade. However, a trend (P=0.09, χ2 test) was found between LOH and age distribution: adult ependymomas seemed to display more frequent LOHs than pediatric ependymomas (93.3% versus 72.2%). In particular, genotypes displaying LOH at D9S2136 were found more frequently in adults (23%) than in children (9%) (P=0.047, χ2 test). Comparing cases with LOH on chromosomal arm 6q and/or chromosome 9, we found 9 tumors showing only LOH on the long arm of chromosome 6 and 7 tumors only on chromosome 9. Only 2 out of 18 tumors showed concurrent LOH on 6q and on chromosome 9 (Fig. 3). However, a statistical inverse correlation between LOH 6q and LOH 9 failed to reach significance (P=0.5). We found no association between losses of the two chromosomes and loss of chromosome 22. There was no relationship between LOHs and whether the tumor was primary or recurrent.
Discussion
A previous study from our group suggested that LOH on the long arm of chromosome 22 plays an important role in pathogenesis of ependymoma. In this work, we have identified other chromosomal regions that may contain candidate genes involved in the development of ependymomas. The most frequent LOH occurred on 6q, as 30.3% of tumors tested showed a deletion of a part or the whole long arm of chromosome 6. Deletions and rearrangements involving 6q have been reported in a number of human malignancies, including gliomas [18], primitive neuroectodermal tumor [34], breast carcinoma [33], acute lymphoblastic leukemia [8], and thymoma [39]. Previous cytogenetic studies on ependymomas showed deletions or rearrangements of 6q with variable frequencies [15, 23]. Loss of 6q has been reported as the most common genetic aberration using the CGH approach [24]. Tong et al. [35] performed allelotyping studies of ependymomas using 384 microsatellite markers. A high frequency of LOH was detected on 6q (68.75%) and a hot spot deletion region was defined at chromosome 6q25.2-27. However, only 16 ependymomas (grade II) were included in that study and no relationship between genetic alterations and clinicopathological features was detected. To our knowledge, our study represents the largest series to date of ependymomas investigated by microsatellite analysis for genetic aberrations on the long arm of chromosome 6q. The 6q24-25.3 was the most frequent deletion region in this work, frequent aberrations were detected also in 6q15-16 and 6q21-22.1. In a previous lymphoma study, one of the hot spots was detected in the region 6q23.3-25.3 between the markers D6S310 to D6S441 overlapping our above-mentioned region [31]. This region contains several already cloned genes, e.g., IGF2R, MAP3K5, and ZAC. Interestingly, the ZAC tumor suppressor gene has been shown to inhibit tumor cell proliferation in vitro and in vivo in nude mice [30] and its expression was found to be lost or reduced in breast cancer cell lines and primary breast tumors [3]. Putative tumor suppressor loci at 6q22 and 6q23-q24 are involved in the malignant progression of sporadic endocrine pancreatic tumors [1]. Whatever gene is the target of deletions here, it seems to define a particularly important event in ependymoma pathogenesis. Regarding region 6q15-16, several studies reported the deletion of this region in breast tumors [26], acute lymphoblastic leukemia and non-Hodgkin's lymphomas [20]. A transcription factor, BACH2, which possesses an inhibitory effect on cell proliferation, was localized to this region [27]. Additional studies are in progress to narrow the 6q15-16 and 6q24-25.3 regions and identify potential tumor suppressor genes that are involved in ependymoma tumorigenesis.
Chromosome 9 was the second most frequently altered chromosome in this study. Region 9p21 contains CDKN2A (encoding p16INK4a) and CDKN2B (encoding p15INK4b), well-known tumor suppressor genes that are frequently altered in various types of human neoplasms, including brain tumors. The inactivation of CDKN2A may play a role in progression of thymoma and thymic carcinoma [9]. In brain tumor, CDKN2A deletions were also associated with evolution of neuroblastoma [32], glioblastomas [22] and worse prognosis in oligodendrogliomas [4]. CDKN2A inactivation may not play an important role in the malignant transformation of ependymomas [5]; however, inactivation of the p14ARF seems to be involved in ependymoma progression [14].
Comparing cases with LOH on chromosome 6q and/or chromosome 9, there appears to be a trend to inverse correlation between LOH on chromosome 6q and 9. This negative correlation was also found by CGH methods [28].
Regarding genetic aberrations on other chromosomes, relatively frequent LOHs were detected in regions 3p14.2, 10q23, 11q13.1, 11q23, 13q14, and 17p13. Of these chromosomal regions, 3p has rarely been reported in the previous studies of ependymomas. With conventional cytogenetics, losses of chromosome 10 were reported in about 9% of ependymomas [12] as well as in gliomas [13]. Losses of chromosome 13 were described in approximately 5% ependymomas [23]. The tumor suppressor genes Fhit, PTEN, MEN1, ATM, Rb and P53 were localized to the above-mentioned loci, respectively.
Interestingly, LOH-positive genotypes were found preferentially in adults (93.3%) as opposed to children (72.2%). Nevertheless, children ependymoma patients have a worse prognosis than adult patients with histopathologically comparable tumors [19]. This suggests that the clinical behavior of ependymomas may not be simply correlated to the number of LOHs per case. LOHs on chromosome 9 were preferentially associated with male patients (8 male versus 1 female patients, P=0.02). Our results support the notion that molecular biological analysis might show a different aberration pattern in various subtypes of ependymomas, as has already been shown for astrocytomas [25]. As most of the cases that we collected are fairly recent, a longer waiting period will be needed to correlate LOH results with patient survival.
In conclusion, our data demonstrate that ependymal tumors of all WHO grades suffer allelic losses during carcinogenesis. The most frequent LOHs were found on the long arm of chromosome 6 with hot spots in 6q15-16 or 6q24-25.3 and chromosome 9. We conclude that important tumor suppressor genes are situated on these two chromosomes.
Reference
Barghorn A, Speel EJ, Farspour B, Saremaslani P, Schmid S, Perren A, Roth J, Heitz PU, Komminoth P (2001) Putative tumor suppressor loci at 6q22 and 6q23-q24 are involved in the malignant progression of sporadic endocrine pancreatic tumors. Am J Pathol 158:1903–1911
Bhattacharjee MB, Armstrong DD, Vogel H, Cooley LD (1997) Cytogenetic analysis of 120 primary pediatric brain tumors and literature review. Cancer Genet Cytogenet 97:39–53
Bilanges B, Varrault A, Basyuk E, Rodriguez C, Mazumdar A, Pantaloni C, Bockaert J, Theillet C, Spengler D, Journot L (1999) Loss of expression of the candidate tumor suppressor gene ZAC in breast cancer cell lines and primary tumors. Oncogene 18:3979–3988
Bortolotto S, Chiadò-Piat L, Cavalla P, Bosone I, Chiò A, Mauro A, Schiffer D (2000) CDKN2A/p16 inactivation in the prognosis of oligodendrogliomas. Int J Cancer 88:554–557
Bortolotto S, Chiadò-Piat L, Cavalla P, Bosone I, Mauro A, Schiffer D (2001) CDKN2A/p16 in ependymomas. J Neurooncol 54:9-13
Ebert C, Haken M von, Meyer-Puttlitz B, Wiestler OD, Reifenberger G, Pietsch T, Deimling A von (1999) NF2 mutations and chromosome 22q loss occur preferentially in intramedullary spinal ependymomas. Am J Pathol 155:627–632
Hamilton RL, Pollack IF (1997) The molecular biology of ependymomas. Brain Pathol 7:807–822
Hayashi Y, Raimondi SC, Look AT, Behm FG, Kitchingman GR, Pui CH, Rivera GK, Williams DL (1990) Abnormalities of the long arm of chromosome 6 in childhood acute lymphoblastic leukemia. Blood 76:1626–1630
Hirabayashi H, Fujii Y, Sakaguchi M, Tanaka H, Yoon HE, Komoto Y, Inoue M, Miyoshi S, Matsuda H (1997) p16INK4, pRB, p53 and cyclin D1 expression and hypermethylation of CDKN2 gene in thymoma and thymic carcinoma. Int J Cancer 73:639–644
Hirose Y, Aldape K, Bollen A, James CD, Brat D, Lamborn K, Berger M, Feuerstein BG (2001) Chromosomal abnormalities subdivide ependymal tumors into clinically relevant groups. Am J Pathol 158:1137–1143
Huang B, Starostik P, Kühl J, Tonn JC, Roggendorf W (2002) Loss of heterozygosity on chromosome 22 in human ependymomas. Acta Neuropathol 103:415–420
James CD, He J, Carlbom E, Mikkelsen T, Ridderheim PA, Cavenee WK, Collins VP (1990) Loss of genetic information in central nervous system tumors common to children and young adults. Genes Chromosomes Cancer 2:94–102
Kim DH, Mohapatra G, Bollen A, Waldman FM, Feuerstein BG (1995) Chromosomal abnormalities in glioblastoma multiforme tumors and glioma cell lines detected by comparative genomic hybridization. Int J Cancer 60:812–819
Korshunov A, Golanov A, Timirgaz V (2001) p14ARF protein (FL-132) immunoreactivity in intracranial ependymomas and its prognostic significance: an analysis of 103 cases. Acta Neuropathol 102:271–277
Kramer DL, Parmiter AH, Rorke LB, Sutton LN, Biegel JA (1998) Molecular cytogenetic studies of pediatric ependymomas. J Neurooncol 37:25–33
Kraus JA, Millas W de, Sörensen N, Herbold C, Schichor C, Tonn JC, Wiestler OD, Deimling A von, Pietsch T (2001) Indications for a tumor suppressor gene at 22q11 involved in the pathogenesis of ependymal tumors and distinct from hSNF5/INI1. Acta Neuropathol 102:69–74
Lamszus K, Lachenmayer L, Heinemann U, Kluwe L, Finckh U, Höppner W, Stavrou D, Fillbrandt R, Westphal M (2001) Molecular genetic alterations on chromosomes 11 and 22 in ependymomas. Int J Cancer 91:803–808
Liang BC, Ross DA, Greenberg HS, Meltzer PS, Trent JM (1994) Evidence of allelic imbalance of chromosome 6 in human astrocytomas. Neurology 44:533–536
Lyons MK, Kelly PJ (1991) Posterior fossa ependymomas: report of 30 cases and review of the literature. Neurosurgery 28:659–664
Merup M, Moreno TC, Heyman M, Rönnberg K, Grandér D, Detlofsson R, Rasool O, Liu Y, Söderhäll S, Juliusson G, Gahrton G, Einhorn S (1998) 6q deletions in acute lymphoblastic leukemia and non-Hodgkin's lymphomas. Blood 91:3397–3400
Mork SJ, Loken AC (1977) Ependymoma: a follow-up study of 101 cases. Cancer 40:907–915
Nakamura M, Watanabe T, Klangby U, Asker C, Wiman K, Yonekawa Y, Kleihues P, Ohgaki H (2001) p14ARF deletion and methylation in genetic pathways to glioblastomas. Brain Pathol 11:159–168
Ransom DT, Ritland SR, Kimmel DW, Moertel CA, Dahl RJ, Scheithauer BW, Kelly PJ, Jenkins RB (1992) Cytogenetic and loss of heterozygoty studies in ependymomas, pilocytic astrocytomas, and oligodendrogliomas. Genes Chromosomes Cancer 5:348–356
Reardon DA, Entrekin RE, Sublett J, Ragsdale S, Li H, Boyett J, Kepner JL, Look AT (1999) Chromosome arm 6q loss is the most common recurrent autosomal alteration detected in primary pediatric ependymoma. Genes Chromosomes Cancer 24:230–237
Rickert CH, Sträter R, Kaatsch P, Wassmann H, Jürgens H, Dockhorn-Dworniczak B, Paulus W (2001) Pediatric high-grade astrocytomas show chromosomal imbalances distinct from adult cases. Am J Pathol 158:1525–1532
Rodriguez C, Causse A, Ursule E, Theillet C (2000) At least five regions of imbalance on 6q in breast tumors, combining losses and gains. Genes Chromosomes Cancer 27:76–84
Sasaki S, Ito E, Toki T, Maekawa T, Kanezaki R, Umenai T, Muto A, Nagai H, Kinoshita T, Yamamoto M, Inazawa J, Taketo MM, Nakahata T, Igarashi K, Yokoyama M (2000) Cloning and expression of human B cell-specific transcription factor BACH2 mapped to chromosome 6q15. Oncogene 19:3739–3749
Scheil S, Brüderlein S, Eicker M, Herms J, Herold-Mende C, Steiner HH, Barth TF, Möller P (2001) Low frequency of chromosomal imbalances in anaplastic ependymomas as detected by comparative genomic hybridization. Brain Pathol 11:133–143
Schiffer D, Giordana MT (1998) Prognosis of ependymoma. Child Nerv Syst 14:357–361
Spengler D, Villalba M, Hoffmann A, Pantaloni C, Houssami S, Bockaert J, Journot L (1997) Regulation of apoptosis and cell cycle arrest by Zac1, a novel zinc finger protein expressed in the pituitary gland and the brain. EMBO J 16:2814–2825
Starostik P, Greiner A, Schultz A, Zettl A, Peters K, Rosenwald A, Kolve M, Müller-Hermelink HK (2000) Genetic aberrations common in gastric high-grade large B-cell lymphoma. Blood 95:1180–1187
Takita J, Hayashi Y, Kohno T, Yamaguchi N, Hanada R, Yamamoto K, Yokota J (1997) Deletion map of chromosome 9 and p16 (CDKN2A) gene alterations in neuroblastoma. Cancer Res 57:907–912
Theile M, Seitz S, Arnold W, Jandrig B, Frege R, Schlag PM, Haensch W, Guski H, Winzer KJ, Barrett JC, Scherneck S (1996) A defined chromosome 6q fragment (at D6S310) harbors a putative tumor suppressor gene for breast cancer. Oncogene 13:677–685
Thomas GA, Raffel C (1991) Loss of heterozygosity on 6q, 16q, and 17p in human central nervous system primitive neuroectodermal tumors. Cancer Res 51:639–643
Tong CY, Zheng PP, Pang JC, Poon WS, Chang AR, Ng HK (2001) Identification of novel regions of allelic loss in ependymomas by high-resolution allelotyping with 384 microsatellite markers. J Neurosurg 95:9–14
Ward S, Harding B, Wilkins P, Harkness W, Hayward R, Darling JL, Thomas DG, Warr T (2001) Gain of 1q and loss of 22 are the most common changes detected by comparative genomic hybridisation in paediatric ependymoma. Genes Chromosomes Cancer 32:59–66
Wiestler OD, Schiffer D, Coons SW, Prayson RA, Rosenblum MK (2000) Ependymal tumours. In: Kleihues P, Cavenee WK (ed) Pathology and genetics of tumours of the nervous system. IARC Press, Lyon, pp 71–81
Zheng PP, Pang JC, Hui AB, Ng HK (2000) Comparative genomic hybridization detects losses of chromosomes 22 and 16 as the most common recurrent genetic alterations in primary ependymomas. Cancer Genet Cytogenet 122:18–25
Zhou R, Zettl A, Ströbel P, Wagner K, Müller-Hermelink HK, Zhang SJ, Marx A, Starostik P (2001) Thymic epithelial tumors can develop along two different pathogenetic pathways. Am J Pathol 159:1853–1860
Acknowledgements
We thank Prof. W. Paulus for stimulating discussion and providing samples and clinical data. We gratefully thank Dr. B. Puppe for statistical analyses. This research project has been supported by a grant from the Sander Foundation (no. 99.070.1).
Author information
Authors and Affiliations
Corresponding author
Additional information
Dedicated to Prof. Dr. H.K. Mueller-Hermelink's 60th birthday.
Rights and permissions
About this article
Cite this article
Huang, B., Starostik, P., Schraut, H. et al. Human ependymomas reveal frequent deletions on chromosomes 6 and 9. Acta Neuropathol 106, 357–362 (2003). https://doi.org/10.1007/s00401-003-0739-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-003-0739-5